Questions and Answers
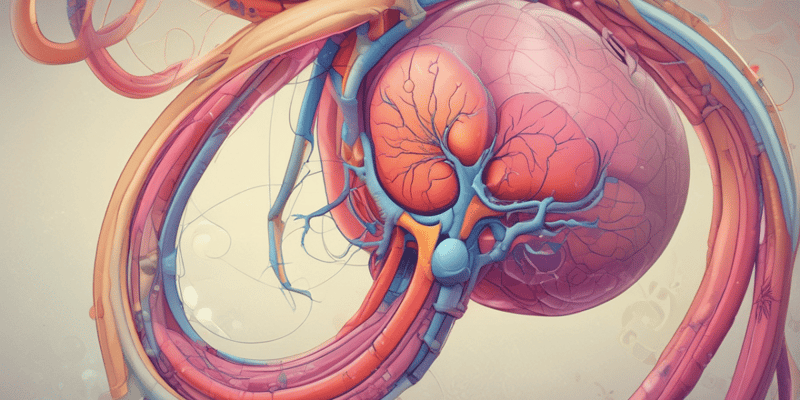
Which of the following best describes the hilum of the kidneys?
The hilum is the entry and exit site on the medial side of each kidney.
Which of the following correctly describes what enters and exits through the hilum of the kidney?
The renal artery enters, while the renal vein exits through the hilum.
What is the first part of the renal tubule?
Proximal convoluted tubule
What is the main process that occurs in the proximal convoluted tubule?
Signup and view all the answers
What is the juxtaglomerular apparatus?
Signup and view all the answers
What is the site of blood filtration in the kidney?
Signup and view all the answers
Which of the following best describes why the ascending loop of Henle is referred to as the "diluting segment"?
Signup and view all the answers
Why is the descending loop of Henle called the concentrating segment?
Signup and view all the answers
What is the primary function of the Distal Convoluted tubule ( DCT)?
Signup and view all the answers
What are the three processes involved in the formation of urine?
Signup and view all the answers
Which arterioles do blood from the renal arteries enter the nephrons through?
Signup and view all the answers
What is the outer layer of the kidneys called?
Signup and view all the answers
What is the function of the renal papilla?
Signup and view all the answers
Which arterioles does blood leaving the glomerulus exit through?
Signup and view all the answers
What is the process that occurs in the distal convoluted tubule (DCT)?
Signup and view all the answers
What is the primary function of the ureters?
Signup and view all the answers
What is the deeper inner layer of the kidneys called?
Signup and view all the answers
What is the function of the trigone region in the urinary bladder?
Signup and view all the answers
In which segments of the renal tubule does ADH primarily act?
Signup and view all the answers
What is the effect of ADH on urine concentration?
Signup and view all the answers
What structure transports urine from the bladder to the outside of the body?
Signup and view all the answers
What is the function of aldosterone?
Signup and view all the answers
Does ADH cause the loss of water in urine or gain of water in urine?
Signup and view all the answers
What is the function of reabsorption in the nephron?
Signup and view all the answers
What is the result of ADH causing the gain of water in urine?
Signup and view all the answers
What is the primary function of the bladder?
Signup and view all the answers
Which of the following best describes the function of the urethra?
Signup and view all the answers
What is the triangular area in the urinary bladder formed by the two ureteral openings and the urethral opening?
Signup and view all the answers
What is the function of secretion in the nephron?
Signup and view all the answers
Where does most reabsorption occur in the renal tubules?
Signup and view all the answers
What is the origin of urea?
Signup and view all the answers
What substance does the Juxtaglomerular cells secrete to restore blood pressure?
Signup and view all the answers
What is micturition?
Signup and view all the answers
What type of molecules are not filtered into the capsule of the nephron?
Signup and view all the answers
What is the primary function of the glomerulus in the nephron?
Signup and view all the answers
Which part of the loop of Henle is permeable to solutes?
Signup and view all the answers
What is the purpose of the descending loop of Henle in the nephron?
Signup and view all the answers
What part of the nephron loop is permeable to water?
Signup and view all the answers
What is the primary function of angiotensin-converting enzyme (ACE)?
Signup and view all the answers
Where is angiotensinogen primarily produced?
Signup and view all the answers
What is the effect of renin on angiotensinogen?
Signup and view all the answers
What is the role of angiotensin in the body?
Signup and view all the answers
What protein does renin activate?
Signup and view all the answers
Where is angiotensin-converting enzyme (ACE) primarily produced?
Signup and view all the answers
What is ACE?
Signup and view all the answers
Which of the following describes the effect of angiotensin II on blood vessels
Signup and view all the answers
What is ADH?
Signup and view all the answers
What endocrine structure produces ADH? Release it?
Signup and view all the answers
What is the primary effect of angiotensin 2 on the hypothalamus?
Signup and view all the answers
What is the primary function of aldosterone in the body?
Signup and view all the answers
Where is aldosterone produced in the body?
Signup and view all the answers
Which of the following best describes vasopressin?
Signup and view all the answers
What is the effect of vasopressin on the body?
Signup and view all the answers
What is the outcome of angiotensin 2 stimulating the hypothalamus?
Signup and view all the answers
What is the primary function of aldosterone in the body?
Signup and view all the answers
Where is aldosterone produced in the body?
Signup and view all the answers
What is the function of vasopressin in the body?
Signup and view all the answers
What is the result of angiotensin 2 stimulating the hypothalamus?
Signup and view all the answers
What are the components of the filtration membrane in the renal system?
Signup and view all the answers
What are the three effects of Angiotensin 2?
Signup and view all the answers
How do the kidneys regulate glomerular filtration rate (GFR) when blood pressure is low?
Signup and view all the answers
What is the primary function of Angiotensin II in the body?
Signup and view all the answers
What is the role of the visceral membrane in the filtration membrane?
Signup and view all the answers
What triggers the activation of the renin-angiotensin-aldosterone system?
Signup and view all the answers
What is the primary function of LDL in the body?
Signup and view all the answers
Which of the following lipoproteins is often referred to as 'good cholesterol'?
Signup and view all the answers
What is the primary effect of high levels of LDL in the body?
Signup and view all the answers
Which of the following systems is responsible for regulating blood pressure in response to changes in blood volume or sodium content?
Signup and view all the answers
What is the direct role of the electron transport chain in oxidative phosphorylation?
Signup and view all the answers
During oxidative phosphorylation, what is the primary function of the protons pumped into the intermembrane space?
Signup and view all the answers
What is the primary mechanism by which ATP is formed during oxidative phosphorylation?
Signup and view all the answers
Which of the following describes how ATP is formed during oxidative phosphorylation?
Signup and view all the answers
Study Notes
- Ureters transport urine from the kidneys to the bladder.
- The bladder stores urine until micturition, the process of urination, the voluntary release of urine from the bladder to the outside of the body.
- The urethra transports urine from the bladder to the outside of the body.
- Antidiuretic hormone (ADH) promotes water reabsorption in the kidneys, decreasing urine volume and increasing urine concentration.
- ADH primarily acts on the distal convoluted tubule and the collecting duct.
- Aldosterone promotes sodium reabsorption and potassium secretion in the distal convoluted tubule and collecting duct, increasing blood volume and pressure.
- In the presence of ADH, urine is concentrated, and ADH causes the gain of water in urine, reducing urine output.
- The trigone is a triangular area in the urinary bladder formed by the two ureteral openings and the urethral opening.
- The outer layer of the kidneys is called the renal cortex, and the deeper inner layer is called the renal medulla.
- The renal papilla is the tip of the renal pyramid that releases urine into the minor calyx.
- Renal tubules are structures that lead away from the glomerulus and include the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and the collecting duct.
- The three processes involved in the formation of urine are glomerular filtration, tubular reabsorption, and tubular secretion.
- The major process in the distal convoluted tubule (DCT) is the selective reabsorption and secretion of ions to fine-tune salt and water balance.
- The juxtaglomerular apparatus is a structure in the kidney that regulates the function of each nephron, the functional units of the kidney.
- The macula densa cells monitor and respond to changes in the sodium chloride (NaCl) concentration of the fluid in the distal convoluted tubule and adjust GFR and renin release accordingly.
- Blood is filtered in the glomerulus, and renal tubules are structures that lead away from the glomerulus.
- The main process that occurs in the PCT is the reabsorption of water, ions, and all organic nutrients.
- The PCT is the first part of the renal tubule.
- The descending loop of Henle is called the concentrating segment because it is permeable to water but not to solutes, leading to increased solute concentration as water is reabsorbed.
- The ascending loop of Henle is called the diluting segment because it is impermeable to water but allows solutes to be reabsorbed, thus diluting the fluid.
- Blood from the renal arteries enters the nephrons through the afferent arterioles, and blood leaving the glomerulus must exit through the efferent arterioles.
- Most reabsorption occurs in the proximal convoluted tubule.
- Secretion eliminates substances from the blood to the tubule, while reabsorption returns substances from the tubule to the blood.
- Urea is a waste product formed in the liver from the breakdown of proteins and is excreted in the urine.
- Juxtaglomerular cells secrete renin, which helps restore blood pressure by activating the renin-angiotensin-aldosterone system.
- The glomerulus is a network of capillaries at the beginning of a nephron that performs the first step of filtering blood to form urine.
- Large molecules such as proteins and blood cells are not filtered into the capsule.
- Renin is an enzyme that converts angiotensinogen into angiotensin I, and ACE converts angiotensin I to angiotensin II.
- Angiotensin II stimulates the hypothalamus to release ADH, which increases water reabsorption in the kidneys.
- Aldosterone helps regulate blood pressure by increasing sodium and water reabsorption in the kidneys, and it is produced in the adrenal cortex.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge of kidney anatomy with this quiz! Learn about the hilum, renal cortex, renal medulla, and renal papilla.