Questions and Answers
Why is it important to elevate the foot of the bed in a patient on traction?
To prevent the patient from sliding down the bed
What is the primary cause of edema in fractures?
Bleeding and damage to surrounding soft tissues
What occurs between the fractured bone ends during the process of bone repair?
A fibrin meshwork forms
Which of the following symptoms of fractures may cause an extremity to bend backwards or assume an unusual shape?
Signup and view all the answers
What occurs to the muscles near the fracture site?
Signup and view all the answers
What is the primary function of osteoclasts in the process of bone remodeling?
Signup and view all the answers
What is the goal of medical management in fracture care?
Signup and view all the answers
What is the main difference between intracapsular and extracapsular hip fractures?
Signup and view all the answers
Why are older adults more susceptible to hip fractures?
Signup and view all the answers
What is a potential complication of intracapsular hip fractures?
Signup and view all the answers
What is assessed during a thorough neurological examination of a patient with a vertebral fracture?
Signup and view all the answers
What is the primary purpose of electrical stimulation in delayed fracture healing?
Signup and view all the answers
What is the primary purpose of skeletal pin external fixation?
Signup and view all the answers
What is the primary goal of medical management in shock?
Signup and view all the answers
What is the characteristic of fat embolism?
Signup and view all the answers
What is the purpose of fasciotomy in compartment syndrome?
Signup and view all the answers
What is the primary method of evaluating kidney damage in a patient with a pelvic fracture?
Signup and view all the answers
What is the primary purpose of traction in fracture care?
Signup and view all the answers
What should be included in patient education prior to cast application?
Signup and view all the answers
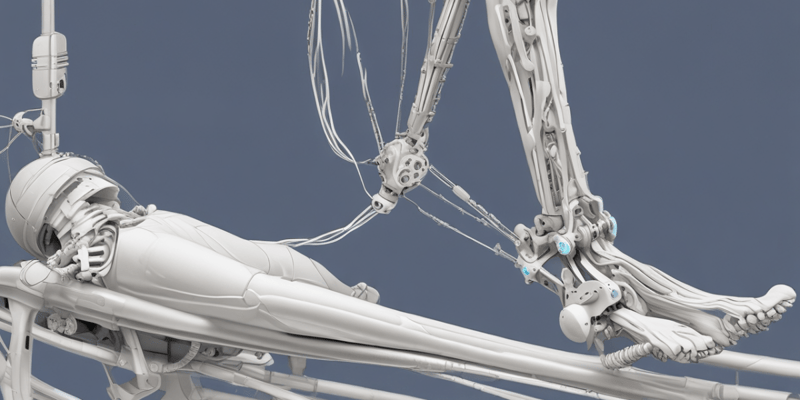
What is the purpose of using a CircOlectric Bed?
Signup and view all the answers
Study Notes
Signs and Symptoms of Fractures
- Fractures vary in location and function of the involved bone, strength of muscle attachment, and type of fracture
- Common signs and symptoms:
- Pain, increasing with movement and pressure
- Loss of function and skeletal muscular impairment
- Deformity, crepitus, and false motion
- Edema, spasms, and loss of sensation or paralysis
- Bruising or hematoma
Process of Bone Repair
- Periosteum and surrounding blood vessels are torn, leading to:
- Soft tissue inflammation and swelling
- Blood clotting and fibrin meshwork formation
- Osteoblasts and osteoclasts working together to remodel the callus into trabecular bone
- Bone repair process involves inflammation, soft callus formation, and bony callus formation
Assessment of Fractures
- Seven Ps of orthopedic assessment:
- Pain, pallor, paresthesia, paralysis, polar temperature, puffiness, and pulselessness
- Collection of subjective and objective data, including:
- Pain, loss of sensation or movement, and cause of injury
- Warmth, edema, ecchymosis, and signs of systemic shock
Diagnosis and Management of Fractures
- Radiographic examination, fluoroscopy, and other diagnostic tests
- Medical management goals:
- Establishing function and continuity of the bone
- Immediate management:
- Splinting, preservation of body alignment, and elevation
- Application of cold packs and analgesics
- Secondary management:
- Simple fracture: optimal reduction and immobilization
- Compound fracture: surgical debridement, antibiotics, and wound closure
Hip Fracture
- Prevalence and incidence:
- Most common type of fracture, especially in older adults
- Women are at a higher risk due to osteoporosis and longer life expectancy
- Types of hip fractures:
- Intracapsular: fracture inside the joint, may disrupt blood supply to the femur head
- Extracapsular: fracture outside the joint, more common and has adequate blood supply
- Symptoms:
- Severe pain, tenderness, and shortening of the affected leg
- External rotation of the leg and foot
- Diagnostic testing:
- X-ray and CBC to evaluate for blood loss
- Treatment:
- Temporary immobilization and traction
- Surgical repairs, including internal fixation and joint replacement
Vertebrae Fracture
- Etiology and pathophysiology:
- Fractures may involve vertebral body, lamina, or articulating processes
- Displacement may put pressure on spinal nerves, causing paralysis
- Clinical manifestations:
- Pain, partial or complete loss of mobility or sensations
- Evidence of fractures on radiographic examination
- Assessment:
- Subjective data: pain, numbness, tingling, and inability to move
- Objective data: neurological assessment, vital signs, and signs of hemorrhage
- Diagnosis:
- Radiographic studies and spinal tap
- Medical management:
- Stable injuries: pain management and anticoagulant therapy
- Unstable injuries: fracture reduction, postural positioning, and cranial-skeletal traction
Pelvic Fracture
- Etiology and pathophysiology:
- Fractures result from trauma, especially falls from heights or automobile accidents
- Hemorrhage and blood loss can be extensive
- Clinical manifestations:
- Unable to bear weight without discomfort
- Tenderness, edema, and hematuria
- Hemorrhage, which can be life-threatening
- Assessment:
- Subjective data: pelvic pain, tenderness, and anxiety
- Objective data: muscle spasm, ecchymosis, and inability to raise legs
- Vital signs, including hypotension, tachycardia, and tachypnea
Compartment Syndrome
- Definition: a condition caused by increased tissue pressure within a compartment, leading to ischemia and tissue death
- Signs and symptoms:
- Pain, numbness, and tingling in the affected extremity
- Inability to flex fingers or toes
- Coolness, pale or blue skin, and slow capillary refill
- Medical management:
- Fasciotomy to relieve pressure and allow return to normal blood flow
- Prompt management to prevent permanent disability
- Nursing interventions:
- Analgesics, elevation, and cold packs
- Removing constricting material and monitoring for signs of shock
Shock
- Definition: a condition caused by inadequate blood flow and oxygenation to the body's tissues
- Assessment:
- Subjective data: restless, anxiety, and weakness
- Objective data: hypotension, tachycardia, tachypnea, and oliguria
- Medical management:
- Restore blood volume using blood volume expanders and oxygen
- Central line insertion and shock trousers
- Nursing interventions:
- Monitoring vital signs and urinary output
- Avoiding sedatives, tranquilizers, and narcotics
- Maintaining the patient flat in bed and NPO
Fat Embolism
- Definition: a condition caused by the combination of platelets and fat in the pulmonary circulation, leading to brain hypoxia and tissue death
- Assessment:
- Subjective data: mental disturbances, irritability, and chest pain
- Objective data: tachypnea, dyspnea, hypoxemia, and petechiae
- Diagnosis:
- Blood gases, CBC, and urine tests
- Sedimentation rate and echocardiogram
- Medical management:
- Directed at prevention, including careful immobilization and shock interventions
- Oxygen therapy and steroid therapy
Gas Gangrene
- Definition: a severe infection of the skeletal muscle caused by gram-positive bacteria, especially in the presence of compound fractures
- Assessment:
- Subjective data: pain, toxic delirium, and characteristic gas bubbles
- Objective data: crepitus, skin necrosis, and thin watery discharge
- Medical management:
- Establishing a larger wound to promote drainage
- Antibiotic therapy and amputation
- Nursing interventions:
- Wound care with strict medical asepsis
- Contact isolation and autoclaving contaminated equipment
Thromboembolus
- Definition: a condition in which a blood vessel is occluded by an embolus
- Assessment:
- Subjective data: pain, tenderness, and swelling in the lower extremities
- Objective data: erythema, warmth, and edema
- Diagnosis:
- Labs, Doppler ultrasonography, and CT scan
- Medical management:
- Anticoagulant therapy, thromboectomy, and antiembolic stockings
- Nursing interventions:
- Bedrest with foot of bed elevated
- Active exercise, hot compresses, and monitoring for signs of bleeding### Delayed Fracture Healing
- Failure of the ends of the fractured bones to unite within 6-9 months
- Non-union: failure of the ends of the fractured bones to unite within 6-9 months
- Electrical stimulation: a new method of treatment in promoting healing, electrical probes stimulate bone production
External Fixation Devices
- Used to hold bone fragments in normal position
- Casts, skeletal and skin traction, braces, and metal pins are examples
- Skeletal pin external fixation:
- Technique immobilizes fractures by the use of pins inserted through the bone and attached to rigid external metal frame
- Provides support of comminuted open fractures, infected nonunions, and infected unstable joints
- Performed under general anesthesia
- Placed in balance suspension traction- helps relieve edema
- Pins are inserted and checked q 4 hrs with careful observation of signs of infection and loose pins
- Remove dried exudates from around the pins as ordered, with the prescribed cleaning agent and surgical asepsis
Casts
- Purpose:
- Hold bone in place while it heals
- Types:
- Short arm cast - extends from below the elbow
- Long leg cast - extends from the upper thigh to the base of the toes
- Spica (body) cast - covers the trunk and one or two extremities
- Bivalve cast: splitting the cast on 2 sides to provide support but relieve pressure
- Initial Assessment of a New Cast:
- Establish baseline measurements and assess neurovascular status before cast application
- Palpate distal pulses, assess color, temperature, and capillary refill of the appropriate fingers or toes
- Check skin at cast edges for erythema and irritation
- Check for odors and drainage coming from cast
- Elevate the affected extremity on pillows until danger of edema is over- usually 24-48 hours
- Nursing Interventions/ Patient Teaching:
- Patient Education:
- Explain why the cast is being applied and how it will be applied
- Advise that the plaster cast will feel warm as it dries
- Explain extent of immobilization
- Explain care of the cast
- Instruct not to insert sharp objects down the cast
- Handling of the cast:
- Support wet cast with flat of the hand (palm) or on pillows: avoid indentations that will cause pressure
- Expose the cast to air
- Place cotton blankets or absorbent material under cast
- Use cast dryer or hair dryer- warm setting
- Do not apply paint, varnish, or shellac to the cast
- Skin care:
- Inspect skin at edges
- Remove plaster crumbs from the skin with a washcloth
- Use creams and lotions sparingly
- Waterproof material around perineal area
- Attend to complaints of pain
- Turning:
- Turn to any position
- Do not grasp abductor bar (spica cast)
- Toileting:
- Use fracture pan with pad
- Elevate head of bed
- Immobilization:
- Weight-bearing discretion of MD
- Cast shoe or walking heel
- Patient Education:
Traction
- The process of putting an extremity, bone, or group of muscles under tension by means of weights and pulleys
- Used to:
- Align and stabilize the patient's fractured bone ends and immobilize until healing occurs
- Relieve pressure on nerves as in the case of herniated disk syndrome
- Maintains correct positioning
- Decrease muscle spasms and relieves pain
- Prevent deformities
- Types of traction:
- Skeletal traction: applied directly to a bone
- Skin traction: uses weight that pulls on sponge rubber, moleskin, and elastic bandage attached to the skin below the fracture site
- Balanced suspension traction- most common form of skeletal traction for treatment of patients with fractures of the femoral shaft or humerus
- Buck's extension: simplest and most common type of skin traction
- Russell's traction: skin traction
Nursing Care of the Patient in Traction
- Check frequently to see that the patient hand or foot is warm and of normal color
- Neurovascular assessment of affected limb, no numbness or tingling should be present
- Check to be sure that all ropes are in the grooves of the pulleys
- Ensure patient is always in prescribed position
- Provide for meticulous skin care
- Provide pin care q8h with appropriate cleansing solution per MD orders and observe pin or wire insertion sites for signs of infection frequently
Frames, Splints, Crutches, and Braces
- Frames: used to assist with turning and positioning while maintaining proper alignment
- Balkan frame
- Bradford frame
- Stryker wedge turning frame and Foster bed
- CircOlectric Bed
- RotoRest Bed
- Splints, Crutches, and Braces: used to immobilize and assist with ambulation
- Numerous types of splints and braces
- Safety is the first concern when ambulatory devices are used
- Crutch safety involves proper measurements, rubber tips on the ends of crutches, and adequate muscle strength in the upper extremities
- Cane walking is more popular with older patients and is used for balance and support
- Walkers are also used by the older adult and will assist the patient in maintaining balance
- Roll-A-Bout walkers are designed for patients with an injury below the knee
Fractures: Signs, Symptoms, and Management
- Fractures vary in signs and symptoms according to location, function, and type of fracture, as well as the amount of related damage.
- Common signs and symptoms:
- Pain, especially with movement or pressure
- Loss of function or mobility
- Deformity or abnormal alignment
- Crepitus (grating sound of bone ends moving)
- False motion
- Edema or swelling
- Spasms
- Loss of sensation or paralysis
- Bruising or hematoma
Process of Bone Repair
- Initial stages:
- Periosteum and surrounding blood vessels are torn, causing hemorrhage and edema
- Soft tissue surrounding the fracture becomes inflamed and swollen
- Blood in the area clots, forming a fibrin meshwork
- Bone repair process:
- Osteoblasts cross the fibrin meshwork, holding it firm while collagen deposits calcium
- A callus (bony deposits) forms between and around the bone ends
- Osteoblasts and osteoclasts work together to remodel the callus into trabecular bone
Assessment and Diagnosis of Fractures
- Seven Ps of orthopedic assessment:
- Pain
- Pallor
- Paresthesia (numbness or tingling)
- Paralysis
- Polar temperature (skin temperature)
- Puffiness (edema or swelling)
- Pulselessness
- Collection of subjective and objective data
- Radiographic examination (e.g., X-ray, fluoroscopy) for diagnosis
Medical Management of Fractures
- Goals:
- Establish function and continuity of the bone
- Prevent complications
- Immediate management:
- Splinting to prevent edema
- Preservation of body alignment
- Elevation of the affected part
- Application of cold packs
- Analgesics and pain management
- Observation for signs of shock
- Secondary management:
- Reduction of the fracture (e.g., closed reduction, open reduction with internal fixation)
- Immobilization (e.g., casts, splints, traction)
Nursing Interventions and Patient Teaching
- Nursing interventions:
- Pain management
- Prevention of complications (e.g., DVT, PE, fat embolus)
- Wound care and infection prevention
- Support and positioning
- Monitoring for signs of shock and infection
- Patient teaching:
- Proper positioning and alignment
- Pain management techniques
- Wound care and infection prevention
- Signs and symptoms of complications
- Importance of follow-up care
Hip Fractures
- Prevalence:
- Most common type of fracture treated in the hospital
- Mostly seen in older adults due to physiological changes
- Types:
- Intra-capsular (inside the joint)
- Extra-capsular (outside the joint)
- Symptoms:
- Severe pain and tenderness
- Shortening and edema of the affected leg
- External rotation of the leg and foot
- Treatment:
- Temporary immobilization and traction
- Surgical repairs (e.g., internal fixation, arthroplasty)
Vertebrae Fractures
- Clinical manifestations:
- Pain at the site of injury
- Partial or complete loss of mobility or sensation
- Evidence of fracture or dislocation on radiographic examination
- Assessment:
- Subjective data (e.g., pain, numbness, tingling)
- Objective data (e.g., neurological examination, vital signs)
- Diagnosis:
- Radiographic studies (e.g., X-ray, CT scan, myelography)
- Spinal tap (presence of blood indicates trauma)
- Medical management:
- Stable injuries: pain management and bracing
- Unstable injuries: fracture reduction, postural positioning, and cranial-skeletal traction
Pelvic Fractures
- Clinical manifestations:
- Unable to bear weight without discomfort
- Tenderness, edema, and hematuria (blood in urine)
- Hemorrhage and shock
- Assessment:
- Subjective data (e.g., pelvic pain, tenderness)
- Objective data (e.g., muscle spasm, ecchymosis, inability to raise legs)
- Diagnosis:
- Radiographic studies (e.g., X-ray, CT scan, IV pyelogram)
- Lab tests (e.g., CBC, urine, stool)
- Medical management:
- Remains on bedrest
- Symphysis pubis fracture with same side iliac fracture: surgery and skeletal traction
- Bilateral pelvic fracture: pelvic sling, skeletal traction, and spica cast
Compartment Syndrome
- Signs and symptoms:
- Pain and numbness or tingling in the affected extremity
- Inability to flex fingers or toes
- Coolness, pale, or blue skin
- Absence of pulse
- Slow capillary refill
- Medical management:
- Fasciotomy to relieve pressure and allow return to normal blood flow
- Prompt management to prevent permanent disability
- Nursing interventions:
- Analgesics
- Elevation of the affected limb
- Application of cold packs
- Accurate monitoring of vital signs
Shock
- Assessment:
- Subjective data (e.g., level of consciousness, restlessness, anxiety)
- Objective data (e.g., hypotension, tachycardia, tachypnea, oliguria)
- Medical management:
- Restore blood volume
- Blood volume expanders (e.g., LR, D5NS, whole blood, plasma, or plasma substitutes)
- Oxygen
- Central line for accurate vital sign monitoring
- Shock trousers to counteract hypotension
- Nursing interventions:
- Check IV fluids and rate
- Monitor IV site for infiltration
- Accurate monitoring of vital signs
- Urinary output monitoring
- Flat in bed
- NPO
Fat Embolism
- Assessment:
- Subjective data (e.g., mental disturbances, irritability, restless, disoriented)
- Objective data (e.g., tachypnea, dyspnea, hypoxemia, crackles, and wheezes)
- Medical management:
- Directed at prevention
- Careful immobilization of the long bone fracture
- Shock interventions (e.g., fluids, oxygen)
- Nursing interventions:
- Accurate monitoring of ABGs
- IV fluids
- Steroid therapy
- Digoxin
- Oxygen
- Incentive spirometry### Lung Sounds and Anticoagulants
- Assess lung sounds every 4 hours
- Monitor PT, PTT, and INR for anticoagulants
Fracture Healing
- Delayed fracture healing: fails to heal within the usual time
- Non-union: failure of the fracture ends to unite within 6-9 months
- Electrical stimulation: a new method of treatment promoting healing by stimulating bone production
External Fixation Devices
- Used to hold bone fragments in normal position
- Examples: casts, skeletal and skin traction, braces, and metal pins
- Skeletal pin external fixation:
- Technique immobilizes fractures by using pins inserted through the bone and attached to a rigid external metal frame
- Provides support for comminuted open fractures, infected nonunions, and infected unstable joints
- Performed under general anesthesia
- Placed in balance suspension traction to relieve edema
- Pins are inserted and checked every 4 hours with careful observation of signs of infection and loose pins
Casts
- Purpose: hold bone in place while it heals
- Types:
- Short arm cast: extends from below the elbow
- Long leg cast: extends from the upper thigh to the base of the toes
- Spica (body) cast: covers the trunk and one or two extremities
- Bivalve cast: splitting the cast on two sides to provide support but relieve pressure
- Initial assessment:
- Establish baseline measurements and assess neurovascular status before cast application
- Palpate distal pulses, assess color, temperature, and capillary refill of the appropriate fingers or toes
- Check skin at cast edges for erythema and irritation
- Check for odors and drainage coming from the cast
- Nursing interventions:
- Patient education:
- Explain why the cast is being applied and how it will be applied
- Advise that the plaster cast will feel warm as it dries
- Explain the extent of immobilization
- Explain care of the cast
- Instruct not to insert sharp objects down the cast
- Handling of the cast:
- Support wet cast with the flat of the hand or on pillows
- Expose the cast to air
- Place cotton blankets or absorbent material under the cast
- Use a cast dryer or hair dryer on a warm setting
- Skin care:
- Inspect skin at edges
- Remove plaster crumbs from the skin with a washcloth
- Use creams and lotions sparingly
- Waterproof material around the perineal area
- Attend to complaints of pain
- Turning:
- Turn to any position
- Do not grasp the abductor bar (spica cast)
- Toileting:
- Use a fracture pan with a pad
- Elevate the head of the bed
- Patient education:
Traction
- Definition: the process of putting an extremity, bone, or group of muscles under tension by means of weights and pulleys
- Types:
- Skeletal traction: applied directly to a bone
- Skin traction: uses a weight that pulls on sponge rubber, moleskin, and elastic bandage attached to the skin below the fracture site
- Principles of nursing care:
- Check frequently to see that the patient's hand or foot is warm and of normal color
- Check to be sure that all ropes are in the grooves of the pulleys
- Ensure the patient is always in the prescribed position
- Provide for meticulous skin care
- Provide pin care every 8 hours with appropriate cleansing solution per MD orders and observe pin or wire insertion sites for signs of infection frequently
Frames
- Definition: can be used for orthopedic patients to assist with turning and positioning while maintaining proper alignment
- Types:
- Balkan frame: wooden or steel attachment to the hospital bed with adjustable pulleys and a trapeze bar attached to an overhead bar
- Bradford frame: rectangular steel with two pieces of canvas stretched tightly and laced to the frame
- Stryker wedge turning frame and Foster bed: similar and assist in changing the patient's position from supine to prone
- CircOlectric Bed: vertical turning bed that can be operated electrically by one person and can be placed in a variety of positions
- RotoRest Bed: can rock a patient as much as 62 degrees, 17 times an hour, to heal pressure ulcers, prevent venous thrombosis, and reduce kidney stone formation
Splints, Crutches, and Braces
- Definition: used to immobilize and assist with ambulation
- Types:
- Numerous types of splints and braces
- Safety:
- Proper measurements and application of each device
- Crutch safety involves:
- Proper measurements (weight must be on hands, not axillae, to avoid plexus paralysis)
- Rubber tips on the ends of crutches to prevent slippage
- Adequate muscle strength in the upper extremities to support the patient's weight
- Cane walking: used for balance and support, especially for older patients
- Walkers: used to assist older adults in maintaining balance
- Roll-A-Bout walkers: designed for patients with an injury below the knee
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge on orthopedic traction methods, devices, and patient care. Assess your understanding of Russell's traction, distal pulses, Balkan frames, and CircOlectric Beds.