42 Questions
What is the primary function of the respiratory zone?
To provide a site for gas exchange between the lungs and bloodstream
What is the name of the thin, double-layered serosa that surrounds the lungs?
Pleurae
What is the approximate thickness of the respiratory membrane?
0.5-μm-thick
Which type of cells in the alveolar walls secrete surfactant and antimicrobial proteins?
Type II cells
What is the term for the pressure difference between the intrathoracic pressure and the pressure inside the lungs?
Transpulmonary pressure
What is the primary function of the pulmonary circulation?
To deliver systemic venous blood to the lungs
What is the atmospheric pressure at sea level?
760 mm Hg
Which of the following statements is true about intrapleural pressure?
It is always negative.
What is the primary function of the opposing forces in the thoracic cavity?
To promote lung collapse.
What type of pressure is described as less than 760 mm Hg?
Negative respiratory pressure.
Which of the following forces tends to enlarge the lungs?
One outward force.
What is the primary effect of increased airway resistance on breathing?
More strenuous breathing movements
What is the purpose of surfactant in the alveoli?
To reduce surface tension and discourage alveolar collapse
What is the relationship between the partial pressure of a gas and its percentage in a mixture?
The partial pressure is directly proportional to its percentage
What is the primary factor that influences the amount of gas that dissolves in a liquid?
Solubility of the gas
What is the purpose of the ventilation-perfusion coupling in the lungs?
To match ventilation and perfusion for efficient gas exchange
What is the effect of a decrease in pH on hemoglobin's affinity for oxygen?
It decreases hemoglobin's affinity for oxygen
What is the primary mechanism of CO2 transport in the blood?
Transported as bicarbonate ions
What is the effect of increased intrapulmonary pressure on lung compliance?
It decreases lung compliance
What is the role of the medullary respiratory centers in the control of breathing?
To integrate information and regulate breathing
What is the relationship between the partial pressure of oxygen in the lungs and its binding to hemoglobin?
As oxygen partial pressure increases, hemoglobin's affinity for oxygen increases
What is the primary reason why intrapleural pressure is always negative?
Due to the balance between the two opposing forces in the thoracic cavity
What is the relationship between intrapulmonary pressure and intrapleural pressure during inspiration?
Intrapulmonary pressure increases, while intrapleural pressure decreases
What is the effect of increased intrapleural pressure on lung compliance?
It decreases lung compliance
What is the relationship between intrapulmonary pressure and intrapleural pressure?
Intrapulmonary pressure is always lower than intrapleural pressure
What is the relationship between intrapulmonary pressure and atmospheric pressure during expiration?
Intrapulmonary pressure is greater than atmospheric pressure
What is the primary function of the alveolar macrophages in the respiratory zone?
To keep alveolar surfaces sterile
What is the primary force that promotes lung expansion during inspiration?
Diaphragmatic contraction
What is the effect of increased airway resistance on lung compliance?
It decreases lung compliance
What is the primary function of the pulmonary circulation?
To deliver systemic venous blood to the lungs
What is the relationship between the partial pressure of a gas and its percentage in a mixture?
The partial pressure of a gas is directly proportional to its percentage in a mixture
What is the primary factor that influences the amount of gas that dissolves in a liquid?
The partial pressure of the gas
What is the primary effect of a decrease in alveolar surface tension on lung compliance?
It increases lung compliance
Which of the following is a consequence of inadequate ventilation-perfusion coupling in the lungs?
Decreased gas exchange
What is the primary mechanism by which CO2 is transported in the blood?
As carbaminohemoglobin and bicarbonate ions
What is the effect of an increase in intrapulmonary pressure on the respiratory membrane?
It decreases the surface area of the respiratory membrane
What is the primary factor that influences the amount of oxygen that binds to hemoglobin in the lungs?
Partial pressure of oxygen
What is the effect of a decrease in lung compliance on breathing?
It makes breathing more difficult
Which of the following is a consequence of emphysema?
Decreased surface area for gas exchange
What is the primary function of the medullary respiratory centers?
Regulation of breathing rate
What is the effect of an increase in airway resistance on lung compliance?
It decreases lung compliance
What is the relationship between the partial pressure of a gas and its solubility in a liquid?
The partial pressure of a gas is directly proportional to its solubility in a liquid
Study Notes
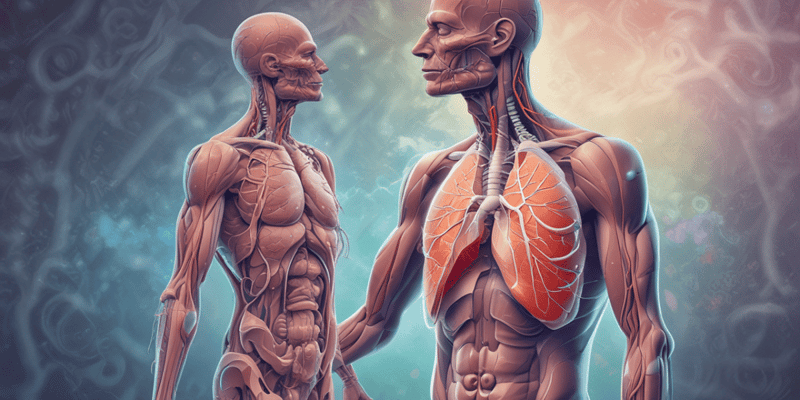
Trachea Functional Anatomy
- Respiratory zone: site of gas exchange, consisting of microscopic structures (respiratory bronchioles, alveolar ducts, and alveoli)
- Conducting zone: conduits to gas exchange sites, includes all other respiratory structures
- Respiratory muscles: diaphragm and other muscles that promote ventilation
The Upper Respiratory Tract
- Bronchi and subdivisions: 23 orders of branching, forming the bronchial (respiratory) tree
- Conducting zone structures:
- Trachea → right and left main (primary) bronchi
- Each main bronchus enters the hilum of one lung
- Right main bronchus is wider, shorter, and more vertical than the left
- Each main bronchus branches into lobar (secondary) bronchi (three right, two left)
- Each lobar bronchus supplies one lobe
Respiratory Zone
- Respiratory bronchioles, alveolar ducts, alveolar sacs (clusters of alveoli)
- ~300 million alveoli account for most of the lungs’ volume and are the main site for gas exchange
- Alveoli are surrounded by fine elastic fibers and contain open pores that connect adjacent alveoli and allow air pressure throughout the lung to be equalized
Respiratory Membrane
- ~0.5-μm-thick air-blood barrier where alveolar and capillary walls meet
- Alveolar walls consist of a single layer of squamous epithelium (type I cells) and scattered type II cells that secrete surfactant and antimicrobial proteins
Pleura of the Lungs
- Thin, double-layered serosa
- Parietal pleura on thoracic wall and superior face of diaphragm
- Visceral pleura on external lung surface
- Pleural fluid fills the slitlike pleural cavity, providing lubrication and surface tension
Blood Supply
- Pulmonary circulation (low pressure, high volume):
- Pulmonary arteries deliver systemic venous blood
- Pulmonary veins carry oxygenated blood from respiratory zones to the heart
- Systemic circulation (high pressure, low volume):
- Bronchial arteries provide oxygenated blood to lung tissue
- Bronchial veins carry most venous blood back to the heart
Mechanics of Breathing
- Pulmonary ventilation consists of two phases:
- Inspiration: gases flow into the lungs
- Expiration: gases exit the lungs
- Pressure relationships in the thoracic cavity:
- Atmospheric pressure: 760 mm Hg at sea level
- Respiratory pressures are described relative to 760 mm Hg
- Negative respiratory pressure is less than 760 mm Hg
- Positive respiratory pressure is greater than 760 mm Hg
Intrapulmonary Pressure and Intrapleural Pressure
- Intrapulmonary (intra-alveolar) pressure: pressure in the alveoli, fluctuates with breathing
- Intrapleural pressure: pressure in the pleural cavity, fluctuates with breathing, and is always negative
Airway Resistance and Lung Compliance
- Airway resistance: as resistance rises, breathing movements become more strenuous
- Lung compliance: a measure of the change in lung volume that occurs with a given change in transpulmonary pressure
- Normally high due to distensibility of lung tissue and alveolar surface tension
- Diminished by nonelastic scar tissue (fibrosis), reduced production of surfactant, and decreased flexibility of the thoracic cage
Gas Exchanges
- External respiration: exchange of O2 and CO2 between the lungs and the atmosphere
- Internal respiration: exchange of O2 and CO2 between the blood and tissues
Dalton's Law of Partial Pressures
- Total pressure exerted by a mixture of gases is the sum of the pressures exerted by each gas
- The partial pressure of each gas is directly proportional to its percentage in the mixture
Henry's Law
- When a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure
- At equilibrium, the partial pressures in the two phases will be equal
- The amount of gas that will dissolve in a liquid also depends on its solubility
Test your understanding of lung compliance, airway resistance, and their effects on breathing. Learn how changes in airway resistance can impact ventilation and how medications like epinephrine can help. This quiz covers the importance of alveolar surface tension and its role in the respiratory system.
Make Your Own Quizzes and Flashcards
Convert your notes into interactive study material.
Get started for free