Podcast
Questions and Answers
What is the primary characteristic of Chronic Obstructive Pulmonary Disease (COPD)?
What is the primary characteristic of Chronic Obstructive Pulmonary Disease (COPD)?
Which of the following is a factor that can trigger asthma symptoms?
Which of the following is a factor that can trigger asthma symptoms?
Chronic bronchitis is primarily defined by which of the following symptoms?
Chronic bronchitis is primarily defined by which of the following symptoms?
How is asthma categorized when there are no known triggers or allergies involved?
How is asthma categorized when there are no known triggers or allergies involved?
Signup and view all the answers
What type of asthma is specifically caused by exposure to certain medications?
What type of asthma is specifically caused by exposure to certain medications?
Signup and view all the answers
Which cells are involved in the inflammatory response seen in asthma?
Which cells are involved in the inflammatory response seen in asthma?
Signup and view all the answers
What distinguishes emphysema from other lung conditions like chronic bronchitis?
What distinguishes emphysema from other lung conditions like chronic bronchitis?
Signup and view all the answers
What is a major feature of COPD compared to asthma?
What is a major feature of COPD compared to asthma?
Signup and view all the answers
What effect can beta2 agonists have on blood pressure?
What effect can beta2 agonists have on blood pressure?
Signup and view all the answers
Which of the following is a common central nervous system effect of beta-adrenergic agonists?
Which of the following is a common central nervous system effect of beta-adrenergic agonists?
Signup and view all the answers
What is a major risk when combining beta-adrenergic agonists with nonselective beta blockers?
What is a major risk when combining beta-adrenergic agonists with nonselective beta blockers?
Signup and view all the answers
Which xanthine derivative is commonly used for bronchodilation?
Which xanthine derivative is commonly used for bronchodilation?
Signup and view all the answers
What is an adverse effect commonly associated with anticholinergic medications?
What is an adverse effect commonly associated with anticholinergic medications?
Signup and view all the answers
Salmeterol is indicated for which role in asthma management?
Salmeterol is indicated for which role in asthma management?
Signup and view all the answers
What is an important consideration when using albuterol?
What is an important consideration when using albuterol?
Signup and view all the answers
Which of the following effects is NOT associated with xanthine derivatives?
Which of the following effects is NOT associated with xanthine derivatives?
Signup and view all the answers
What effect do anticholinergics primarily have on airway secretions?
What effect do anticholinergics primarily have on airway secretions?
Signup and view all the answers
What is one potential cardiovascular side effect of using xanthine derivatives?
What is one potential cardiovascular side effect of using xanthine derivatives?
Signup and view all the answers
What is an indicator for carefully monitoring patients on beta-adrenergic agonists if they have diabetes?
What is an indicator for carefully monitoring patients on beta-adrenergic agonists if they have diabetes?
Signup and view all the answers
Which anticholinergic is often described as the oldest and most commonly used?
Which anticholinergic is often described as the oldest and most commonly used?
Signup and view all the answers
Which of the following is a potential adverse effect of both anticholinergics and xanthines?
Which of the following is a potential adverse effect of both anticholinergics and xanthines?
Signup and view all the answers
Which inhaled corticosteroid is indicated for treating asthma in both adults and children?
Which inhaled corticosteroid is indicated for treating asthma in both adults and children?
Signup and view all the answers
What is a primary role of inhaled corticosteroids in asthma management?
What is a primary role of inhaled corticosteroids in asthma management?
Signup and view all the answers
Inhaled corticosteroids are NOT suitable for patients with which condition?
Inhaled corticosteroids are NOT suitable for patients with which condition?
Signup and view all the answers
What common side effect may occur when starting treatment with inhaled corticosteroids?
What common side effect may occur when starting treatment with inhaled corticosteroids?
Signup and view all the answers
Which corticosteroid is available in both inhaled and intranasal forms?
Which corticosteroid is available in both inhaled and intranasal forms?
Signup and view all the answers
Inhaled corticosteroids may increase the risk of which oral condition?
Inhaled corticosteroids may increase the risk of which oral condition?
Signup and view all the answers
Which medication is classified as an inhaled corticosteroid specifically for asthma management?
Which medication is classified as an inhaled corticosteroid specifically for asthma management?
Signup and view all the answers
Which of the following medication interactions may decrease the effectiveness of inhaled corticosteroids?
Which of the following medication interactions may decrease the effectiveness of inhaled corticosteroids?
Signup and view all the answers
What is an important aspect of patient education regarding inhaler use?
What is an important aspect of patient education regarding inhaler use?
Signup and view all the answers
Which inhaled corticosteroid is known for having a longer duration of action compared to others?
Which inhaled corticosteroid is known for having a longer duration of action compared to others?
Signup and view all the answers
What is the therapeutic range for theophylline blood levels ideally recommended by most clinicians?
What is the therapeutic range for theophylline blood levels ideally recommended by most clinicians?
Signup and view all the answers
Which drug is indicated for use in infants with bradycardia?
Which drug is indicated for use in infants with bradycardia?
Signup and view all the answers
What is the primary action of leukotriene receptor antagonists (LTRAs)?
What is the primary action of leukotriene receptor antagonists (LTRAs)?
Signup and view all the answers
What severe side effects should be monitored in patients taking Montelukast?
What severe side effects should be monitored in patients taking Montelukast?
Signup and view all the answers
Which of the following is NOT a characteristic of corticosteroids?
Which of the following is NOT a characteristic of corticosteroids?
Signup and view all the answers
In which form is aminophylline administered?
In which form is aminophylline administered?
Signup and view all the answers
Which class of drugs is primarily used to prevent asthma attacks rather than treating acute symptoms?
Which class of drugs is primarily used to prevent asthma attacks rather than treating acute symptoms?
Signup and view all the answers
What is an adverse effect commonly associated with leukotriene receptor antagonists?
What is an adverse effect commonly associated with leukotriene receptor antagonists?
Signup and view all the answers
Which LTRA is specifically indicated for treating allergic rhinitis symptoms?
Which LTRA is specifically indicated for treating allergic rhinitis symptoms?
Signup and view all the answers
How do corticosteroids primarily improve asthma treatment?
How do corticosteroids primarily improve asthma treatment?
Signup and view all the answers
What is the main benefit of inhaled corticosteroids compared to oral corticosteroids?
What is the main benefit of inhaled corticosteroids compared to oral corticosteroids?
Signup and view all the answers
Which of the following is a potential complication of long-term corticosteroid use?
Which of the following is a potential complication of long-term corticosteroid use?
Signup and view all the answers
What symptom can bronchoconstriction cause?
What symptom can bronchoconstriction cause?
Signup and view all the answers
What effect do leukotriene receptor antagonists have on mucus secretion in the lungs?
What effect do leukotriene receptor antagonists have on mucus secretion in the lungs?
Signup and view all the answers
What is a primary characteristic of chronic bronchitis?
What is a primary characteristic of chronic bronchitis?
Signup and view all the answers
Which of the following is a common cause of chronic bronchitis?
Which of the following is a common cause of chronic bronchitis?
Signup and view all the answers
What is the effect of emphysema on the alveoli?
What is the effect of emphysema on the alveoli?
Signup and view all the answers
How do short-acting beta-agonists (SABAs) primarily function?
How do short-acting beta-agonists (SABAs) primarily function?
Signup and view all the answers
What is a notable characteristic of long-acting beta-agonists (LABAs)?
What is a notable characteristic of long-acting beta-agonists (LABAs)?
Signup and view all the answers
In which situation are LABAs not recommended for use?
In which situation are LABAs not recommended for use?
Signup and view all the answers
Which medication type is indicated for rapid relief during acute asthma attacks?
Which medication type is indicated for rapid relief during acute asthma attacks?
Signup and view all the answers
What mechanism is triggered by beta-adrenergic agonists after binding to the beta2 receptor?
What mechanism is triggered by beta-adrenergic agonists after binding to the beta2 receptor?
Signup and view all the answers
Which condition can beta-adrenergic agonists be used to treat besides respiratory issues?
Which condition can beta-adrenergic agonists be used to treat besides respiratory issues?
Signup and view all the answers
What is a contraindication for the use of beta-adrenergic agonists?
What is a contraindication for the use of beta-adrenergic agonists?
Signup and view all the answers
What role do anticholinergics play in bronchial treatment?
What role do anticholinergics play in bronchial treatment?
Signup and view all the answers
What is a primary function of bronchodilators?
What is a primary function of bronchodilators?
Signup and view all the answers
Which type of adrenergics only stimulate beta2 receptors?
Which type of adrenergics only stimulate beta2 receptors?
Signup and view all the answers
Study Notes
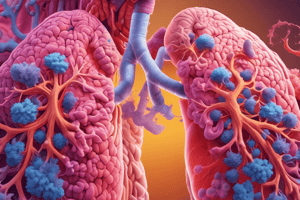
Chronic Obstructive Pulmonary Disease (COPD)
- COPD is a group of lung diseases that cause airflow obstruction.
- It includes chronic bronchitis and emphysema.
- Lung damage is generally irreversible.
- COPD is characterized by an irreversible airflow obstruction in the lungs.
Bronchial Asthma
- Bronchial asthma is a chronic inflammatory disease that causes recurring episodes of wheezing, breathlessness, chest tightness, and coughing.
- Airway inflammation, bronchospasm, and mucus hypersecretion lead to airway obstruction.
- Asthma can be intrinsic, extrinsic, exercise-induced, or drug-induced.
Chronic Bronchitis
- Chronic bronchitis is characterized by persistent inflammation and low-grade infection of the bronchi.
- Inflammation leads to excessive mucus secretion and changes in the bronchial structure, causing breathing difficulties.
- It often results from exposure to bronchial irritants like cigarette smoke or air pollution.
Emphysema
- Emphysema damages the alveoli, the tiny air sacs in the lungs.
- It leads to reduced gas exchange and makes it difficult to get enough oxygen.
- Symptoms include shortness of breath, wheezing, and chronic cough.
Pharmacologic Overview: Bronchodilators
- Bronchodilators relax bronchial smooth muscle, widening the bronchi and bronchioles.
- They include beta-adrenergic agonists, anticholinergics, and xanthine derivatives.
Bronchodilators: Beta-Adrenergic Agonists
-
Short-acting Beta-Agonists (SABAs) provide quick relief from bronchospasm.
- Examples include albuterol.
- They're often used as rescue inhalers.
-
Long-acting Beta-Agonists (LABAs) provide long-lasting relief from asthma symptoms, lasting for 12 hours or more.
- Examples include salmeterol and formoterol.
- They are for long-term management of asthma symptoms.
-
Newest LABAs include indacaterol and vilanterol, often available in combination with other medications.
- "Ellipta" refers to a dry powder inhaler delivery system.
Beta-Adrenergic Agonists: Mechanism of Action
- Beta-adrenergic agonists stimulate beta2 receptors, leading to bronchodilation.
- Stimulation of beta2 receptors triggers the production of cyclic adenosine monophosphate (cAMP).
- cAMP relaxes smooth muscle in the airways, improving airflow.
Anticholinergics
- Anticholinergics block the action of acetylcholine, a neurotransmitter that constricts bronchioles.
- Examples include ipratropium, tiotropium, and aclidinium.
- They prevent bronchoconstriction by blocking acetylcholine from binding to muscarinic receptors in the airway, promoting airway relaxation and dilation.
Xanthine Derivatives
- Xanthines, such as theophylline, inhibit phosphodiesterase, increasing cAMP levels, leading to bronchodilation.
- They stimulate the central nervous system and cardiovascular system.
Nonbronchodilating Respiratory Drugs
-
Leukotriene Receptor Antagonists (LTRAs) block the action of leukotrienes, substances that cause inflammation, bronchoconstriction, and mucus production.
- Examples include montelukast, zafirlukast, and zileuton.
- Corticosteroids reduce inflammation in the airways.
- Mast Cell Stabilizers prevent the release of histamine, a substance that causes inflammation and airway constriction in the lungs.
Leukotriene Receptor Antagonists (LTRAs)
- They are used to prevent asthma attacks, not to treat acute attacks.
- They offer an alternative to traditional asthma medications.
Corticosteroids
- They have potent anti-inflammatory effects, reducing inflammation in the airways.
- They are crucial for managing chronic asthma, preventing exacerbations.
- Oral corticosteroids have systemic effects, while inhaled forms are more localized.
Inhaled Corticosteroids
- Examples include beclomethasone dipropionate.
- Used for long-term control of asthma.
Inhaled Corticosteroids: Overview
- Purpose: Primarily used for long-term asthma control, reducing exacerbations, and treating persistent asthma.
- Commonly Used: Budesonide, Ciclesonide, Flunisolide, Fluticasone, Mometasone, Triamcinolone acetonide.
- Mechanism: Control inflammation in the airways by suppressing inflammatory cells and mediators.
- Administration: Inhaled corticosteroids are delivered directly to the lungs, minimizing systemic effects.
Inhaled Corticosteroids: Contraindications
- Drug Allergy: Avoid in patients with known allergy to inhaled corticosteroids.
- Acute Asthma Attacks: Not a primary treatment for acute attacks; bronchodilators are used instead.
- Hypersensitivity: Contraindicated in those with hypersensitivity to glucocorticoids.
- Fungal Infection: Avoid in patients with systemic fungal infections or positive sputum tests for Candida.
Inhaled Corticosteroids: Adverse Effects
- Common: Pharyngeal irritation, coughing, dry mouth, oral fungal infections.
- Systemic Effects (Rare): Adrenal suppression, osteoporosis, cataracts (with high doses or prolonged use).
Inhaled Corticosteroids: Drug Interactions
- Systemic vs. Inhaled: Drug interactions are more likely with systemic corticosteroids; inhaled corticosteroids are generally safe and well-tolerated.
-
Common Interactions:
- Antidiabetic Drugs: May increase serum glucose levels; dosage adjustments may be needed.
- Cyclosporine & Tacrolimus: Increased risk of infections, especially in renal impairment.
- Itraconazole, Ketoconazole, Strong CYP3A4 inhibitors: Potential increase in adverse effects of inhaled corticosteroids.
- Phenytoin, Phenobarbital, Rifampin: Reduced effectiveness of inhaled corticosteroids.
Inhaler: Patient Education
-
Inhaler Technique:
- Teach proper technique for effective medication delivery.
- Demonstrate and practice inhaler use.
- Emphasize correct timing of inhalation and activation.
- Provide a spacer for patients with coordination difficulties.
-
Dose Tracking:
- Ensure patients can monitor their medication use.
- Educate on how to count remaining doses.
- Encourage refilling before running out.
- Advise patients to keep inhalers in a safe, accessible location.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers various chronic lung diseases, including Chronic Obstructive Pulmonary Disease (COPD), bronchial asthma, chronic bronchitis, and emphysema. Learn about their characteristics, causes, and effects on lung function. Test your knowledge on the differences and similarities between these respiratory conditions.