Questions and Answers
What is the primary function of the kidneys in the urinary system?
To regulate blood pH by controlling hydrogen ion concentration
What is the name of the hormone produced by the kidneys that stimulates red blood cell production?
Erythropoietin
What is the name of the tube that carries urine from the kidneys to the bladder?
Ureters
What is the primary function of the bladder in the urinary system?
Signup and view all the answers
What is the role of the kidneys in regulating blood volume and blood pressure?
Signup and view all the answers
What is the name of the process by which the body eliminates waste from the body?
Signup and view all the answers
What is the function of the urethra in the urinary system?
Signup and view all the answers
What is the role of the kidneys in producing vitamin D?
Signup and view all the answers
Match the components of the urinary system with their functions:
Signup and view all the answers
Match the processes with the organs involved in the urinary system:
Signup and view all the answers
Match the urinary system components with their interactions:
Signup and view all the answers
Match the hormones with their functions in the urinary system:
Signup and view all the answers
Match the processes with their importance in the urinary system:
Signup and view all the answers
Match the components of the urinary system with their importance:
Signup and view all the answers
Match the kidney structures with their functions:
Signup and view all the answers
Match the kidney components with their roles:
Signup and view all the answers
Match the nephron components with their functions:
Signup and view all the answers
Match the processes with the location where they occur in the nephron:
Signup and view all the answers
Match the blood vessels with their functions in the kidney:
Signup and view all the answers
Match the nephron structures with their relationships:
Signup and view all the answers
Match the kidney processes with their purposes:
Signup and view all the answers
Match the kidney components with their characteristics:
Signup and view all the answers
Match the kidney processes with their importance:
Signup and view all the answers
What is the primary function of the kidneys in the body?
Signup and view all the answers
Which part of the nephron is responsible for filtration?
Signup and view all the answers
How many nephrons are approximately present in each kidney?
Signup and view all the answers
What is the name of the vessel that carries blood that needs to be filtered and modified into the kidney?
Signup and view all the answers
Where does reabsorption occur in the nephron?
Signup and view all the answers
What is the function of the efferent arteriole in the nephron?
Signup and view all the answers
What is the purpose of the peritubular capillaries in the nephron?
Signup and view all the answers
What is the name of the vessel that carries filtered blood out of the kidney?
Signup and view all the answers
What is the functional unit of the kidney?
Signup and view all the answers
What are the three main processes that occur in the nephron?
Signup and view all the answers
What percentage of water, ions, glucose, urea, and other substances is forced out of the blood during glomerular filtration?
Signup and view all the answers
What is the purpose of the filtration barrier in the glomerulus?
Signup and view all the answers
What is the role of podocytes in the glomerulus?
Signup and view all the answers
What is the result of the afferent arteriole having a larger diameter than the efferent arteriole?
Signup and view all the answers
What is the significance of glomerular filtration rate (GFR) in the kidneys?
Signup and view all the answers
What is dependent on blood pressure and the need to retain or remove fluid volume?
Signup and view all the answers
What is the purpose of regulating the diameter of the afferent arteriole?
Signup and view all the answers
What is the direction of fluid flow in the glomerulus?
Signup and view all the answers
What is the role of hydrostatic pressure in glomerular filtration?
Signup and view all the answers
What is the result of the filtration barrier in the glomerulus?
Signup and view all the answers
Match the following components of the glomerulus with their functions:
Signup and view all the answers
Match the following with their roles in regulating glomerular filtration rate (GFR):
Signup and view all the answers
Match the following with their characteristics in the glomerulus:
Signup and view all the answers
Match the following with their effects on glomerular filtration:
Signup and view all the answers
Match the following with their roles in the urinary system:
Signup and view all the answers
Match the following with their effects on the filtration barrier:
Signup and view all the answers
Match the following with their roles in the nephron:
Signup and view all the answers
Match the following with their characteristics in glomerular filtration:
Signup and view all the answers
What percentage of water is reabsorbed in the proximal convoluted tubule?
Signup and view all the answers
What happens when glucose is not reabsorbed into the bloodstream?
Signup and view all the answers
What is the minimum plasma concentration of a substance that will result in its excretion in the urine?
Signup and view all the answers
Which of the following is NOT reabsorbed in the proximal convoluted tubule?
Signup and view all the answers
What is the function of the proximal convoluted tubule in the nephron?
Signup and view all the answers
How much blood is filtered by the kidneys daily?
Signup and view all the answers
What is the result of high glucose levels in the blood?
Signup and view all the answers
What is the role of glucose in the urinary system?
Signup and view all the answers
How much urine is produced daily by the kidneys?
Signup and view all the answers
Match the following kidney processes with their importance in the urinary system:
Signup and view all the answers
Match the components of the nephron with their functions:
Signup and view all the answers
Match the terms with their definitions in the urinary system:
Signup and view all the answers
Match the kidney structures with their functions in the urinary system:
Signup and view all the answers
What is the primary function of the loop of Henle in the nephron?
Signup and view all the answers
Which hormone regulates the amount of water reabsorbed from the collecting duct as it passes through the medulla?
Signup and view all the answers
What is the significance of the loop of Henle being longer in desert animals like the kangaroo rat?
Signup and view all the answers
What is the direction of water flow in the descending loop of Henle?
Signup and view all the answers
What is the effect of the accumulation of salt in the interstitial fluid in the loop of Henle?
Signup and view all the answers
What is the adaptation that allows the kangaroo rat to conserve water more efficiently?
Signup and view all the answers
What is the direction of salt movement in the ascending limb of the loop of Henle?
Signup and view all the answers
Match the structures of the loop of Henle with their permeability characteristics:
Signup and view all the answers
Match the following nephron structures with their functions:
Signup and view all the answers
Match the components of the nephron with their functions in the loop of Henle:
Signup and view all the answers
Match the characteristics of the medulla with their effects on the kidney:
Signup and view all the answers
Match the following substances with their reabsorption rates in the nephron:
Signup and view all the answers
Match the following hormones with their functions in the nephron:
Signup and view all the answers
Match the components of the nephron with their functions in water reabsorption:
Signup and view all the answers
What is the primary function of the kidneys in regulating electrolyte balance?
Signup and view all the answers
What happens when the body becomes too acidic (acidosis)?
Signup and view all the answers
In which part of the nephron does reabsorption of glucose, amino acids, and salts occur?
Signup and view all the answers
What is the result of the loop of Henle creating a hyperosmotic medulla?
Signup and view all the answers
What is the function of the kidneys in regulating blood pH?
Signup and view all the answers
What is the function of the ascending limb of the loop of Henle?
Signup and view all the answers
What is the result of the kidneys regulating electrolyte levels?
Signup and view all the answers
What is the function of the descending limb of the loop of Henle?
Signup and view all the answers
What is the role of hormones in the distal convoluted tubule and collecting duct?
Signup and view all the answers
Match the kidney structures with their primary functions:
Signup and view all the answers
Match the kidney regions with their permeability characteristics:
Signup and view all the answers
Match the kidney processes with their purposes:
Signup and view all the answers
Match the kidney components with their relationships:
Signup and view all the answers
Match the kidney regions with their functions in the urinary system:
Signup and view all the answers
Match the kidney processes with their effects on the body:
Signup and view all the answers
Match the kidney structures with their roles in regulating blood pH:
Signup and view all the answers
What triggers the release of ADH?
Signup and view all the answers
What is the primary function of ADH in the kidney?
Signup and view all the answers
What is the effect of ADH on blood vessels?
Signup and view all the answers
What is the significance of the hyperosmotic medulla in the kidney?
Signup and view all the answers
What is the effect of chronic elevation of blood pressure due to ADH?
Signup and view all the answers
What is the target of ADH in the kidney?
Signup and view all the answers
What is the result of increased blood volume due to ADH?
Signup and view all the answers
What is another name for ADH?
Signup and view all the answers
Match the following structures with their functions in the regulation of ADH:
Signup and view all the answers
Match the following effects with the location where they occur in the kidney:
Signup and view all the answers
Match the following terms with their definitions related to ADH:
Signup and view all the answers
Match the following with their roles in the regulation of blood water levels:
Signup and view all the answers
Match the following with their effects on the body:
Signup and view all the answers
Match the following structures with their functions in the kidney:
Signup and view all the answers
Match the following with their effects on the kidney:
Signup and view all the answers
What type of hormone is aldosterone?
Signup and view all the answers
What stimulates the adrenal cortex to release aldosterone?
Signup and view all the answers
What is the effect of aldosterone on potassium levels in the blood?
Signup and view all the answers
What is the response to a drop in blood volume and blood pressure?
Signup and view all the answers
What is the result of aldosterone's action on the kidney?
Signup and view all the answers
What triggers the release of aldosterone in response to elevated potassium levels in the blood?
Signup and view all the answers
What system does aldosterone play a role in?
Signup and view all the answers
What is the effect of aldosterone on blood volume and blood pressure?
Signup and view all the answers
Match the hormones with their effects on blood volume and blood pressure:
Signup and view all the answers
Match the components of the renin-angiotensin-aldosterone system with their functions:
Signup and view all the answers
Match the triggers with their corresponding responses in the renin-angiotensin-aldosterone system:
Signup and view all the answers
Match the components of the renin-angiotensin-aldosterone system with their sites of production:
Signup and view all the answers
Match the effects of the renin-angiotensin-aldosterone system on blood pressure with their corresponding mechanisms:
Signup and view all the answers
Study Notes
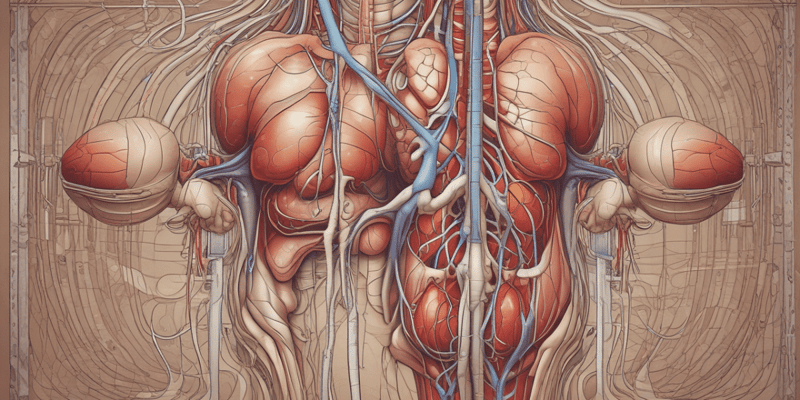
- The urinary system, also known as the renal system, is part of the excretory system, working together with the skin, respiratory system, and digestive system to eliminate waste from the body.
- The urinary system consists of the kidneys, ureters, bladder, and urethra, with the kidneys being located in the back area and the ureters carrying urine from the kidneys to the bladder.
- The bladder, also known as the urinary bladder, stores urine until it is ready to be expelled, and smooth muscles allow the urine to leave the body through the urethra during urination.
- The kidneys play a major role in filtering the blood, removing waste products such as urea, maintaining water and salt balance, regulating ion concentrations, and producing urine.
- The kidneys regulate blood pH by controlling hydrogen ion concentration, and they also help regulate blood volume and blood pressure by getting rid of excess water or retaining it when necessary.
- The kidneys function as an endocrine tissue, producing erythropoietin (EPO), a hormone that stimulates red blood cell production, and they are responsible for producing the active form of vitamin D, which is essential for calcium regulation and bone health.
- The kidneys are involved in all functions of the urinary system except for the excretion part, which is accomplished through the urethra.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.