Podcast
Questions and Answers
What is the estimated transmission risk for receptive anal intercourse with ejaculation?
What is the estimated transmission risk for receptive anal intercourse with ejaculation?
- 1/70 (correct)
- 1/1250
- 1/440
- 1/155
Which type of intercourse has the lowest estimated risk of HIV transmission?
Which type of intercourse has the lowest estimated risk of HIV transmission?
- Receptive vaginal intercourse (RVI)
- Insertive anal intercourse (IAI) circumcised
- Insertive vaginal intercourse (IVI)
- Receptive or insertive oral intercourse (correct)
What is the estimated risk of HIV transmission for needle-stick injury?
What is the estimated risk of HIV transmission for needle-stick injury?
- 1/900
- 1/440 (correct)
- 1/2500
- 1/125
Which of the following has a higher estimated transmission risk than insertive anal intercourse (uncircumcised)?
Which of the following has a higher estimated transmission risk than insertive anal intercourse (uncircumcised)?
What is the estimated risk for circumcised insertive anal intercourse?
What is the estimated risk for circumcised insertive anal intercourse?
Which method is emphasized for history taking in STI assessments?
Which method is emphasized for history taking in STI assessments?
What is a key aspect of maintaining patient confidentiality during STI consultations?
What is a key aspect of maintaining patient confidentiality during STI consultations?
What should be included in a patient's sexual history during STI assessments?
What should be included in a patient's sexual history during STI assessments?
Why is it important to ask about a patient's vaccination history during STI evaluations?
Why is it important to ask about a patient's vaccination history during STI evaluations?
How should a clinician approach the subject of sexual partners in non-heteronormative relationships?
How should a clinician approach the subject of sexual partners in non-heteronormative relationships?
What aspect of a patient's history helps in assessing risk during STI evaluations?
What aspect of a patient's history helps in assessing risk during STI evaluations?
What should clinicians avoid when discussing sexual history with patients?
What should clinicians avoid when discussing sexual history with patients?
Which factor is crucial for encouraging patients to disclose sensitive information during STI assessments?
Which factor is crucial for encouraging patients to disclose sensitive information during STI assessments?
Flashcards are hidden until you start studying
Study Notes
Introduction & Approach
- Major pathogens pose a global public health threat and are often treatable if diagnosed early.
- Early intervention in treatment can prevent severe health outcomes.
- Some infections are preventable through vaccination.
- Education and behavioral change play crucial roles in prevention.
- Diagnosis requires a comprehensive approach, including patient history, physical examination, and lab tests.
History-Taking
- Approach history-taking with calmness, care, and respect for patient confidentiality.
- Establish trust by understanding the reason for the patient's visit (symptoms, concerns, potential exposure).
- Inquire about symptoms like discharge or ulceration, using proper anatomical terminology.
- Assess past STI history and current/recent partner details, avoiding colloquial language.
- Clarify forms of sexual intercourse and use of protection (condoms, dental dams).
- Ask about sexual practices during menstruation and vaccination history (e.g., HBV, HPV).
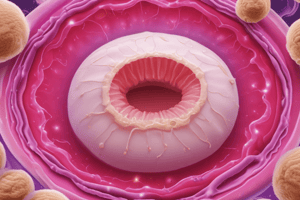
Risk Assessment for HIV Transmission
- Transmission risks vary significantly based on the type of sexual exposure:
- Receptive anal intercourse (RAI) has a transmission risk of 1/70, higher with ejaculation.
- Insertive anal intercourse (uncircumcised) carries a risk of 1/160; circumcised reduces risk to 1/900.
- Receptive vaginal intercourse (RVI) has a risk of 1/1250; insertive vaginal intercourse (IVI) at 1/2500.
- Receptive or insertive oral intercourse presents an extremely low, unquantified risk.
- Contaminated injecting equipment has a risk of 1/125.
- Needle-stick injuries have a risk of 1/440.
Additional History Considerations
- Inquire about the number of sexual partners over recent months/years.
- Assess if the patient has worked as a Commercial Sex Worker (CSW), as regular testing is required.
- Obtain information about partners from overseas or involvement in chem-sex scenarios.
- Discuss sensitive topics such as past sexual assaults or high-risk behaviors.
- Document general medical history, including drug allergies and reproductive history (miscarriages, terminations).
- Recognize that sexual activity is not limited to young people; older adults may also be sexually active.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.