Podcast
Questions and Answers
Which of the following is the most common causative agent of vulvovaginal candidiasis?
Which of the following is the most common causative agent of vulvovaginal candidiasis?
- Candida tropicalis
- Candida albicans (correct)
- Candida krusei
- Candida glabrata
Which of the following is NOT a risk factor for developing vulvovaginal candidiasis?
Which of the following is NOT a risk factor for developing vulvovaginal candidiasis?
- Diabetes
- Recent antibiotic use
- Immunocompromise
- Hyperthyroidism (correct)
What is the typical presentation of a patient with vulvovaginal candidiasis?
What is the typical presentation of a patient with vulvovaginal candidiasis?
- Fever and chills
- Pruritis and a thick, curd-like vaginal discharge (correct)
- Abdominal pain and nausea
- Dysuria and hematuria
Which of the following diagnostic methods is NOT mentioned in the text for vulvovaginal candidiasis?
Which of the following diagnostic methods is NOT mentioned in the text for vulvovaginal candidiasis?
What is the recommended treatment for uncomplicated vulvovaginal candidiasis?
What is the recommended treatment for uncomplicated vulvovaginal candidiasis?
How should vulvovaginal candidiasis be treated in an immunocompromised patient?
How should vulvovaginal candidiasis be treated in an immunocompromised patient?
What is the recommended treatment for vulvovaginal candidiasis in a pregnant patient?
What is the recommended treatment for vulvovaginal candidiasis in a pregnant patient?
What is the recommended treatment for recurrent vulvovaginal candidiasis?
What is the recommended treatment for recurrent vulvovaginal candidiasis?
What is the most common causative agent of Bacterial Vaginosis?
What is the most common causative agent of Bacterial Vaginosis?
Which of the following is a risk factor for developing Bacterial Vaginosis?
Which of the following is a risk factor for developing Bacterial Vaginosis?
How is Bacterial Vaginosis diagnosed according to Amsel's Criteria?
How is Bacterial Vaginosis diagnosed according to Amsel's Criteria?
What symptom is commonly seen in patients with Bacterial Vaginosis?
What symptom is commonly seen in patients with Bacterial Vaginosis?
Which treatment is recommended for all symptomatic patients with Bacterial Vaginosis?
Which treatment is recommended for all symptomatic patients with Bacterial Vaginosis?
Do male partners of women with Bacterial Vaginosis require treatment?
Do male partners of women with Bacterial Vaginosis require treatment?
Asymptomatic patients with Bacterial Vaginosis do not need treatment
Asymptomatic patients with Bacterial Vaginosis do not need treatment
Trichomoniasis commonly presents with Bacterial Vaginosis.
Trichomoniasis commonly presents with Bacterial Vaginosis.
The gold standard for diagnosis of Trichomoniasis is a wet mount that shows motile, flagellated organisms.
The gold standard for diagnosis of Trichomoniasis is a wet mount that shows motile, flagellated organisms.
What is a key cervical finding in a patient with Trichomoniasis?
What is a key cervical finding in a patient with Trichomoniasis?
What is the gold standard for diagnosis of Trichomoniasis?
What is the gold standard for diagnosis of Trichomoniasis?
What is the initial test for Trichomoniasis?
What is the initial test for Trichomoniasis?
What is the recommended treatment for women with Trichomoniasis?
What is the recommended treatment for women with Trichomoniasis?
What is the recommended treatment for men with Trichomoniasis?
What is the recommended treatment for men with Trichomoniasis?
What is a common symptom of chlamydia in women?
What is a common symptom of chlamydia in women?
Which statement about chlamydia is false?
Which statement about chlamydia is false?
What is the first line treatment for chlamydia in non-pregnant patients?
What is the first line treatment for chlamydia in non-pregnant patients?
What diagnostic method is considered the gold standard for chlamydia?
What diagnostic method is considered the gold standard for chlamydia?
Which group should return for a test of cure 3 months post-treatment for chlamydia?
Which group should return for a test of cure 3 months post-treatment for chlamydia?
What is a possible consequence of untreated chlamydia in women?
What is a possible consequence of untreated chlamydia in women?
In addition to genital infections, where else can chlamydia cause infections?
In addition to genital infections, where else can chlamydia cause infections?
What is a common symptom of chlamydia in men?
What is a common symptom of chlamydia in men?
Which antibiotic can pregnant women with chlamydia safely take for treatment?
Which antibiotic can pregnant women with chlamydia safely take for treatment?
What is the purpose of a 'test of cure' after chlamydia treatment?
What is the purpose of a 'test of cure' after chlamydia treatment?
Patients on doxycycline are advised to avoid sunlight due to:
Patients on doxycycline are advised to avoid sunlight due to:
What is the recommended first-line treatment for Gonorrhea?
What is the recommended first-line treatment for Gonorrhea?
What is the diagnostic gold standard for Gonorrhea?
What is the diagnostic gold standard for Gonorrhea?
What is the common co-infection found with Gonorrhea?
What is the common co-infection found with Gonorrhea?
What is the potential consequence of untreated Gonorrhea in women?
What is the potential consequence of untreated Gonorrhea in women?
How often is routine screening recommended for Gonorrhea in patients 25 years of age and younger?
How often is routine screening recommended for Gonorrhea in patients 25 years of age and younger?
What is the causative agent of Gonorrhea?
What is the causative agent of Gonorrhea?
What is the recommended duration of abstinence from sex post-treatment for Gonorrhea?
What is the recommended duration of abstinence from sex post-treatment for Gonorrhea?
What is the hallmark symptom of Pelvic Inflammatory Disease (PID)?
What is the hallmark symptom of Pelvic Inflammatory Disease (PID)?
Which of the following is NOT part of the outpatient treatment for PID?
Which of the following is NOT part of the outpatient treatment for PID?
What is the most common age range for PID?
What is the most common age range for PID?
Which of the following is a medical emergency that needs to be ruled out in a patient with suspected PID?
Which of the following is a medical emergency that needs to be ruled out in a patient with suspected PID?
What is the recommended follow-up time frame for a patient with PID who is not sent to the emergency room?
What is the recommended follow-up time frame for a patient with PID who is not sent to the emergency room?
What is the most common cause of PID?
What is the most common cause of PID?
Which of the following is NOT part of the inpatient treatment for PID?
Which of the following is NOT part of the inpatient treatment for PID?
Which of the following is NOT a symptom of acute PID?
Which of the following is NOT a symptom of acute PID?
How can a medical provider make a presumptive clinical diagnosis of PID?
How can a medical provider make a presumptive clinical diagnosis of PID?
What complication of PID is characterized by perihepatitis and right upper quadrant pain with "violin string" adhesions?
What complication of PID is characterized by perihepatitis and right upper quadrant pain with "violin string" adhesions?
A patient with suspected PID who has high fevers greater than 102.2F along with nausea and vomiting should be sent to the:
A patient with suspected PID who has high fevers greater than 102.2F along with nausea and vomiting should be sent to the:
Which of the following is a complication of untreated Pelvic Inflammatory Disease (PID)?
Which of the following is a complication of untreated Pelvic Inflammatory Disease (PID)?
A pregnant patient with suspected Pelvic Inflammatory Disease (PID) should be:
A pregnant patient with suspected Pelvic Inflammatory Disease (PID) should be:
PID is an _______ acute infection of the upper genital tract
PID is an _______ acute infection of the upper genital tract
Which pathogen is most commonly responsible of cases of Non-Gonococcal Urethritis with no clear etiology?
Which pathogen is most commonly responsible of cases of Non-Gonococcal Urethritis with no clear etiology?
Which of the following antibiotics is recommended for the treatment of non-gonococcal urethritis?
Which of the following antibiotics is recommended for the treatment of non-gonococcal urethritis?
What is the key diagnostic finding in herpes simplex virus on a Tzanck smear?
What is the key diagnostic finding in herpes simplex virus on a Tzanck smear?
What is the preferred mode of delivery for a pregnant woman with an active herpes simplex virus infection to prevent transmission to the infant?
What is the preferred mode of delivery for a pregnant woman with an active herpes simplex virus infection to prevent transmission to the infant?
How long should primary outbreaks of herpes simplex virus be treated with antivirals?
How long should primary outbreaks of herpes simplex virus be treated with antivirals?
Which virus can remain latent in the nerve root ganglion and be reactivated by changes in the immune system?
Which virus can remain latent in the nerve root ganglion and be reactivated by changes in the immune system?
What is considered the first episode of symptoms in a patient (such as genital warts, HSV-2) that is already diagnosed with herpes simplex virus infection (HSV-1)?
What is considered the first episode of symptoms in a patient (such as genital warts, HSV-2) that is already diagnosed with herpes simplex virus infection (HSV-1)?
Which of the following is a common symptom that precedes an outbreak of painful vesicles in herpes simplex virus infections?
Which of the following is a common symptom that precedes an outbreak of painful vesicles in herpes simplex virus infections?
What term is used to describe a patient with a new strain of herpes simplex virus but already has antibodies to the other strain?
What term is used to describe a patient with a new strain of herpes simplex virus but already has antibodies to the other strain?
'SEM' is a complication seen in neonates exposed to which viral infection during delivery?
'SEM' is a complication seen in neonates exposed to which viral infection during delivery?
'Disseminated disease' is a potential consequence seen in neonates exposed to which viral infection?
'Disseminated disease' is a potential consequence seen in neonates exposed to which viral infection?
What is the recommended duration of antiviral treatment for a recurrent outbreak of HSV?
What is the recommended duration of antiviral treatment for a recurrent outbreak of HSV?
Which of the following antivirals is NOT mentioned in the text for the treatment of HSV?
Which of the following antivirals is NOT mentioned in the text for the treatment of HSV?
When is prophylaxis with antivirals recommended for pregnant patients with recurrent HSV infection?
When is prophylaxis with antivirals recommended for pregnant patients with recurrent HSV infection?
How long do most outbreaks of HSV typically resolve spontaneously?
How long do most outbreaks of HSV typically resolve spontaneously?
What is the primary reason for starting antiviral prophylaxis in pregnant patients with recurrent HSV infection?
What is the primary reason for starting antiviral prophylaxis in pregnant patients with recurrent HSV infection?
What is the primary reason for vaccinating patients against HPV?
What is the primary reason for vaccinating patients against HPV?
How long does it typically take for most patients to clear an HPV infection?
How long does it typically take for most patients to clear an HPV infection?
What is the appearance of visible anogenital warts caused by HPV?
What is the appearance of visible anogenital warts caused by HPV?
Which of the following statements about HPV testing is true?
Which of the following statements about HPV testing is true?
How is the HPV vaccine Gardasil 9 administered?
How is the HPV vaccine Gardasil 9 administered?
How soon after coming in contact with a syphilis lesion does it take to create a painless chancre?
How soon after coming in contact with a syphilis lesion does it take to create a painless chancre?
What is the first test ordered if a provider suspects syphilis?
What is the first test ordered if a provider suspects syphilis?
How does secondary syphilis typically present?
How does secondary syphilis typically present?
What is the recommendation for the treatment of syphilis?
What is the recommendation for the treatment of syphilis?
What is the characteristic of a chancre in syphilis?
What is the characteristic of a chancre in syphilis?
Why is a treponemal test ordered after a positive non-treponemal test?
Why is a treponemal test ordered after a positive non-treponemal test?
What can be visible under darkfield microscopy in syphilis?
What can be visible under darkfield microscopy in syphilis?
When does late (tertiary) syphilis occur?
When does late (tertiary) syphilis occur?
If a patient with syphillis reports a penicillin allergy, what is recommended
If a patient with syphillis reports a penicillin allergy, what is recommended
There is early screening for syphilis in pregnancy because it can cross the placental barrier and cause stillbirth on fetus
There is early screening for syphilis in pregnancy because it can cross the placental barrier and cause stillbirth on fetus
What is the primary target of the Human Immunodeficiency Virus (HIV)?
What is the primary target of the Human Immunodeficiency Virus (HIV)?
What is the highest risk mode of transmission for HIV?
What is the highest risk mode of transmission for HIV?
A patient presents with a painful tender, genital ulcer that produces foul smelling discharge. The patient tests negative for HSV and Syphilis. What is likely?
A patient presents with a painful tender, genital ulcer that produces foul smelling discharge. The patient tests negative for HSV and Syphilis. What is likely?
What is the primary stage of Lymphogranuloma Venereum (LGV) characterized by?
What is the primary stage of Lymphogranuloma Venereum (LGV) characterized by?
Which of the following is the recommended treatment for Lymphogranuloma Venereum (LGV)?
Which of the following is the recommended treatment for Lymphogranuloma Venereum (LGV)?
What is the most accurate diagnostic test for Lymphogranuloma Venereum (LGV)?
What is the most accurate diagnostic test for Lymphogranuloma Venereum (LGV)?
Which of the following is a characteristic of the secondary stage of Lymphogranuloma Venereum (LGV)?
Which of the following is a characteristic of the secondary stage of Lymphogranuloma Venereum (LGV)?
What is the late stage presentation of Lymphogranuloma Venereum (LGV)?
What is the late stage presentation of Lymphogranuloma Venereum (LGV)?
A patient presents with intense pubic itching with the presence of lice. What is the treatment?
A patient presents with intense pubic itching with the presence of lice. What is the treatment?
Who should receive annual trichomonas, syphilis, gonorrhea, and chlamydia screening?
Who should receive annual trichomonas, syphilis, gonorrhea, and chlamydia screening?
Which STIs are considered reportable according to the text?
Which STIs are considered reportable according to the text?
Which group of individuals need HIV screening at least once?
Which group of individuals need HIV screening at least once?
Who needs to be screened annually for Gonorrhea and Chlamydia?
Who needs to be screened annually for Gonorrhea and Chlamydia?
What are STATE reportable to partner conditions?
What are STATE reportable to partner conditions?
Study Notes
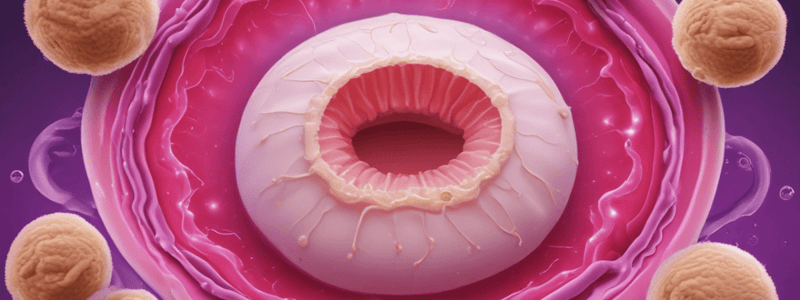
Vulvovaginal Candidiasis (Yeast Infection)
- Caused by candida albicans
- Risk factors: recent antibiotic use, immunocompromise, diabetes, medications like SGLT2 and contraceptives, and pregnancy
- Symptoms: pruritis, burning pain, thick, curd-like vaginal discharge
- Diagnosis: clinical history, findings, and wet mount with KOH
- Treatment: fluconazole (single dose or 150mg every 72 hours for 3 doses) or topical azole medication (short course of 1-3 days)
Trichomoniasis
- Caused by a single-celled flagellated protozoan
- Often presents with bacterial vaginosis
- Symptoms: vaginal irritation, malodorous, froth, yellow/green discharge
- Key cervical finding: punctate hemorrhages on vaginal and cervix
- Diagnosis: gold standard is Nucleic Acid Amplification Test (NAAT) using Genprobe, initial test is wet mount showing motile, flagellated organisms
- Treatment: metronidazole (500mg twice a day for 7 days for women, 2g single dose for men)
- Partner treatment and abstinence from sex for 2 weeks post-treatment are necessary
Bacterial Vaginosis (BV)
- Caused by Gardnerella vaginalis
- Not a sexually transmitted infection (STI)
- Risk factors: being sexually active with a new partner or multiple partners, women who have sex with women, douching, and smoking
- Symptoms: thin white/gray vaginal discharge with a fishy odor
- Diagnosis: Amsel's Criteria (at least 3 of the following: gray/white discharge, clue cells on wet mount, vaginal fluid pH > 4.5, positive whiff/amine test)
- Treatment: metronidazole or clindamycin cream
- Male partners do not need treatment
- Asymptomatic patients do not need treatment
Chlamydia
- Highest reported STI in the United States
- Risk factors: young age, new or multiple sex partners, history of STIs, and/or inconsistent condom use
- Symptoms: cervicitis, cervical discharge, lower abdominal pain, fever, chills, and adnexal tenderness in women; urethritis, penile discharge, and dysuria in men
- Diagnosis: gold standard is Nucleic Acid Amplification Test (NAAT) using Genprobe
- Treatment: doxycycline (100mg twice a day for 7 days) or Azithromycin (1g single dose)
- Partner treatment and testing for cure in 3 months are necessary
Human Papillomavirus (HPV)
- Group of nonenveloped, icosahedral viruses classified within the family Papillomaviridae
- Composed of double-stranded DNA and divided into two major functional regions: early (E) and late (L) regions
- Highly species-specific, infecting humans exclusively
- Transmitted primarily through skin-to-skin contact
- Can persist in the host for varying durations, cleared by the immune system in most cases
- Clinical presentation varies depending on the affected site and type of virus
- Associated with various forms of cancer (anal, cervical, vulvar, vaginal, and oropharyngeal)
- Laboratory studies: detection using molecular techniques like polymerase chain reaction (PCR)
- Prevention strategies: promoting safe sexual practices, improving hygiene, and encouraging vaccination
Gonorrhea
- Found with a co-infection of chlamydia in 50% of cases
- Recommended routine screening annually for patients 25 years of age and younger
- Caused by Neisseria Gonorrhea, a gram-negative diplococci
- Presents exactly the same as Chlamydia
- Diagnostic gold standard: NAAT Genprobe
- Treatment: ceftriaxone (500mg IM injection single dose) or azithromycin (1g single dose)
- Partner treatment and abstinence from sex for 2 weeks post-treatment are necessary
Syphilis
- Caused by Treponema pallidum
- Transmitted through direct contact with an infected lesion
- Symptoms: painless papules that ulcerate into a 1-2 cm chancre with raised indurated margins
- Secondary syphilis: diffuse, symmetric maculopapular eruption involving the entire trunk and extremities
- Diagnosis: non-treponemal test (first test to screen for the bacteria), treponemal test (to confirm the diagnosis by finding syphilis antibodies)
- Treatment: penicillin (IM injection), even if an allergy is present
- Late (tertiary) syphilis: patient often presents with neurological deficits, blindness, and dementia, and internal organ damage
Human Immunodeficiency Virus (HIV)
- Retrovirus that targets and infects key components of the human immune system
- Three stages: asymptomatic HIV infection, clinical latency, and AIDS
- Stages can progress from initial infection to advanced disease
- Symptoms: may not experience any symptoms, may appear healthy, but can still transmit the virus
- Diagnosis: NAAT Genprobe
- Treatment: antiretroviral therapy (ART)
Lymphogranuloma Venereum (LGV)
- Subtype of Chlamydia trachomatis
- Presents in three stages: primary, secondary, and late
- Primary: genital ulcer or mucosal inflammation reaction at the site of inoculation
- Secondary: local direct extension of the infection to the regional lymph nodes, called "buboes"
- Late: fibrosis and strictures in the anogenital tract
- Diagnosis: NAAT
- Treatment: doxycycline (100mg twice a day for 21 days)
Pelvic Inflammatory Disease (PID)
- Ascending acute infection of the upper genital tract
- Caused by untreated Gonorrhea and Chlamydia
- Symptoms: lower abdominal pain, vaginal discharge, cervical discharge, fever, dyspareunia
- Diagnosis: presumptive clinical diagnosis using history and physical exam findings
- Treatment: ceftriaxone (500mg IM for one dose), doxycycline (100mg twice a day for 14 days), and metronidazole (500mg twice a day for 14 days)
- Complications: infertility, increased risk of ectopic pregnancies, and Fitz-Hugh-Curtis Syndrome
Non-Gonococcal Urethritis (NGU)
-
Inflammation of the urethra that is not caused by Neisseria gonorrhea
-
Diagnosis: urinalysis, microscopic examination of first-void urine sediment, urethral swabs, and culture testing
-
Causes: Chlamydia trachomatis, Mycoplasma genitalium, Trichomonas vaginalis, Ureaplasma urealyticum, Haemophilus vaginalis, and Herpes simplex virus
-
Treatment: azithromycin or doxycycline are commonly prescribed for Chlamydia trachomitis infections
-
CDC recommends considering M.genitalium infection in cases of persistent or recurrent urethritis### Genital Herpes (Herpes Simplex)
-
Caused by strains HSV1 and/or HSV2
-
Highly common disease that can present with latency
-
HSV can remain latent in the nerve root ganglion and be reactivated by changes in the immune system
-
Patients tend to report a prodrome of burning, tingling, and itching, followed by an outbreak of painful vesicles on an erythematous base
-
Most outbreaks resolve spontaneously after 10-19 days
Diagnosis and Treatment
- Diagnosed in the clinical setting with viral cultures or PCR swabs if the patient has active lesions
- A Tzanck smear finding of “multi nucleated giant cells” is a key diagnostic finding in HSV
- Primary outbreaks should be treated for 7-10 days with antivirals
- Recurrent outbreaks should be treated for 1-5 days with antivirals
- Antivirals used for HSV include Acyclovir, Valacyclovir, and Famicilovir
- Patients with recurrent HSV infection or pregnant patients can take a daily dose of antivirals to suppress the virus and decrease the risk of spreading the disease to partners
Transmission and Prevention
- Can be transmitted from mother to infant before, during, and after delivery
- Prophylaxis is recommended to be started at 36 weeks gestation in known cases of HSV
- A c-section is preferred if a pregnant woman has an active infection of HSV at time of delivery
- Neonatal HSV can cause localized skin, eye mouth disease (SEM), CNS disease, and/or disseminated disease
Human Papilloma Virus (HPV)
- Most prevalent STI, with at least 50% of sexually active people contracting the virus in their lifetime
- Most patients will clear an HPV infection within 2 years
- Can present as a cutaneous viral infection with flat, common, and plantar warts
- Can present as a mucocutaneous viral infection with genital warts, squamous intraepithelial lesions, or carcinomas of the vagina, vulva, cervix, anus, or penis
- Can impact the oral and respiratory mucosa
- Most patients with HPV are asymptomatic
- Visible anogenital warts present as “soft, flesh colored single or multiple flat, cauliflower-like lesions”
- HPV 16 and 18 account for 70% of cervical cancers
- Gardasil 9 vaccine can be given as a 2 dose series, 6 months apart, if started between ages 9 to 14
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Explore the characteristics and risk factors associated with vulvovaginal candidiasis, commonly known as a yeast infection. Learn about the clinical presentation, diagnosis, and common causes of this condition.