Podcast
Questions and Answers
Which component is part of the structure of thyroid-stimulating hormone?
Which component is part of the structure of thyroid-stimulating hormone?
What is the half-life of thyroid-stimulating hormone in the plasma?
What is the half-life of thyroid-stimulating hormone in the plasma?
Which action is NOT a result of thyroid-stimulating hormone activity?
Which action is NOT a result of thyroid-stimulating hormone activity?
How does TSH primarily exert its effects on target cells?
How does TSH primarily exert its effects on target cells?
Signup and view all the answers
Which component is primarily responsible for the storage of thyroid hormones within the follicles of the thyroid gland?
Which component is primarily responsible for the storage of thyroid hormones within the follicles of the thyroid gland?
Signup and view all the answers
What role does the hypothalamus play in regulating thyroid hormone secretion?
What role does the hypothalamus play in regulating thyroid hormone secretion?
Signup and view all the answers
What feedback mechanism regulates the secretion of thyroid hormones?
What feedback mechanism regulates the secretion of thyroid hormones?
Signup and view all the answers
How does the weight of the thyroid gland generally differ between genders?
How does the weight of the thyroid gland generally differ between genders?
Signup and view all the answers
Which tissue does NOT show an increase in metabolic activity due to thyroxine?
Which tissue does NOT show an increase in metabolic activity due to thyroxine?
Signup and view all the answers
Which of the following hormones is primarily responsible for controlling the secretion of thyroid hormones?
Which of the following hormones is primarily responsible for controlling the secretion of thyroid hormones?
Signup and view all the answers
In hyperthyroidism, how much does the basal metabolic rate increase compared to normal levels?
In hyperthyroidism, how much does the basal metabolic rate increase compared to normal levels?
Signup and view all the answers
What is the main function of the colloidal substance within the thyroid gland?
What is the main function of the colloidal substance within the thyroid gland?
Signup and view all the answers
In which stage does the function of the thyroid gland typically increase?
In which stage does the function of the thyroid gland typically increase?
Signup and view all the answers
What effect does thyroxine generally have on the force of contraction of the heart?
What effect does thyroxine generally have on the force of contraction of the heart?
Signup and view all the answers
In hyperthyroidism, what can happen to the heart muscle due to excess activity?
In hyperthyroidism, what can happen to the heart muscle due to excess activity?
Signup and view all the answers
What is the anatomical structure that connects the two lobes of the thyroid gland?
What is the anatomical structure that connects the two lobes of the thyroid gland?
Signup and view all the answers
What is the primary role of iodine in the thyroid gland?
What is the primary role of iodine in the thyroid gland?
Signup and view all the answers
What is cardiac decompensation?
What is cardiac decompensation?
Signup and view all the answers
How does thyroxine affect blood vessels?
How does thyroxine affect blood vessels?
Signup and view all the answers
The hypothalamus and pituitary regulate thyroid function primarily through which mechanism?
The hypothalamus and pituitary regulate thyroid function primarily through which mechanism?
Signup and view all the answers
What is the typical effect of thyroxine on mean arterial blood pressure?
What is the typical effect of thyroxine on mean arterial blood pressure?
Signup and view all the answers
What are the effects of thyroxine on the respiratory rate?
What are the effects of thyroxine on the respiratory rate?
Signup and view all the answers
What digestive effects does thyroxine typically induce in the gastrointestinal tract?
What digestive effects does thyroxine typically induce in the gastrointestinal tract?
Signup and view all the answers
Why is thyroxine essential for the central nervous system?
Why is thyroxine essential for the central nervous system?
Signup and view all the answers
What is the primary reason T4 has a longer duration of action than T3?
What is the primary reason T4 has a longer duration of action than T3?
Signup and view all the answers
Which hormone forms the majority of thyroid hormone secretion?
Which hormone forms the majority of thyroid hormone secretion?
Signup and view all the answers
How much iodine is required weekly to synthesize normal quantities of thyroid hormones?
How much iodine is required weekly to synthesize normal quantities of thyroid hormones?
Signup and view all the answers
What percentage of total thyroid secretion does T3 represent?
What percentage of total thyroid secretion does T3 represent?
Signup and view all the answers
Which cells synthesize and secrete thyroglobulin?
Which cells synthesize and secrete thyroglobulin?
Signup and view all the answers
What is significant about T3's affinity for plasma proteins?
What is significant about T3's affinity for plasma proteins?
Signup and view all the answers
What essential dietary component is iodized in common table salt to prevent deficiency?
What essential dietary component is iodized in common table salt to prevent deficiency?
Signup and view all the answers
What mechanism is responsible for transporting iodide from blood into follicular cells?
What mechanism is responsible for transporting iodide from blood into follicular cells?
Signup and view all the answers
What happens to the concentration of iodide in the thyroid gland during hyperactivity?
What happens to the concentration of iodide in the thyroid gland during hyperactivity?
Signup and view all the answers
Which enzyme is crucial for the oxidation of iodide to elementary iodine?
Which enzyme is crucial for the oxidation of iodide to elementary iodine?
Signup and view all the answers
What is the term for the process where iodine binds to thyroglobulin within the follicular cavity?
What is the term for the process where iodine binds to thyroglobulin within the follicular cavity?
Signup and view all the answers
Which of the following is NOT a product of iodinated tyrosine coupling reactions?
Which of the following is NOT a product of iodinated tyrosine coupling reactions?
Signup and view all the answers
What is the role of iodinase in the synthesis of thyroid hormones?
What is the role of iodinase in the synthesis of thyroid hormones?
Signup and view all the answers
What configurations result from the coupling of iodotyrosine residues?
What configurations result from the coupling of iodotyrosine residues?
Signup and view all the answers
How are thyroid hormones stored after synthesis?
How are thyroid hormones stored after synthesis?
Signup and view all the answers
What is the primary effect of hypersecretion of thyroxine on body temperature?
What is the primary effect of hypersecretion of thyroxine on body temperature?
Signup and view all the answers
How does thyroxine influence growth in children?
How does thyroxine influence growth in children?
Signup and view all the answers
What are the effects of increased thyroxine secretion on body weight?
What are the effects of increased thyroxine secretion on body weight?
Signup and view all the answers
What role does thyroxine play in erythropoiesis?
What role does thyroxine play in erythropoiesis?
Signup and view all the answers
What is an important clinical indicator for diagnosing hypothyroidism and hyperthyroidism?
What is an important clinical indicator for diagnosing hypothyroidism and hyperthyroidism?
Signup and view all the answers
What happens to children with inadequate levels of thyroid hormone at birth?
What happens to children with inadequate levels of thyroid hormone at birth?
Signup and view all the answers
What effect does thyroid hormone have on metabolic processes in the body?
What effect does thyroid hormone have on metabolic processes in the body?
Signup and view all the answers
What is the impact of thyroid hormone on the growth of bones in hyperthyroid children?
What is the impact of thyroid hormone on the growth of bones in hyperthyroid children?
Signup and view all the answers
Study Notes
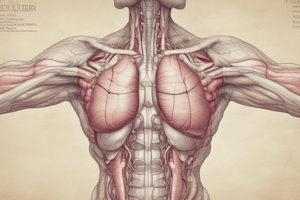
Physiology of Thyroid Gland
- The thyroid gland is an endocrine gland located at the base of the neck, consisting of two lobes connected by an isthmus
- It develops from an evagination of the floor of the pharynx
- It weighs approximately 20-40 grams in adults, larger in females
- Thyroid function varies across the menstrual cycle, increasing during pregnancy and lactation, and decreasing during menopause
- Iodine is crucial for thyroid hormone synthesis and transport, controlled by mechanisms in the gland
- Thyroglobulin, a large glycoprotein, is the major component of the colloid within thyroid follicles
- Thyroid hormones, T3 and T4 (thyroxine), are synthesized and stored in the follicles
- T3 is significantly more potent than T4. T4 has a longer half-life than T3
- Thyroid hormones are crucial for metabolic rate, growth, and development
Histology of Thyroid Gland
- Thyroid tissue is composed of closed follicles
- Follicular cells line the follicles and secrete thyroglobulin
- Colloid, a substance secreted by follicular cells, is contained in the follicles' cavities
- Parafollicular cells are interspersed between follicles and release calcitonin
Chemistry of Thyroid Hormones
- T3 and T4 are iodine-containing derivatives of tyrosine
- T3 is four times more potent than T4
- T4 has a longer half-life
- Thyroid hormones bind to plasma proteins, influencing their release rate
- Total T3 levels are around 0.15µg/dL
- Total T4 levels are around 8µg/dL
Synthesis of Thyroid Hormones (6 steps)
- Thyroglobulin synthesis: Endoplasmic reticulum and Golgi apparatus synthesize thyroglobulin, a large glycoprotein containing tyrosine
- Iodide trapping: Active transport of iodide into follicular cells against electrochemical gradient
- Iodide oxidation: Iodide is oxidized to iodine by thyroid peroxidase, a crucial step
- Iodine transport into the follicle: Iodine is transported from the follicular cells into the follicular cavity by an iodide-chloride pump (pendrin)
- Iodination of tyrosine: Iodine combines with tyrosine residues in thyroglobulin to form monoiodotyrosine (MIT) and diiodotyrosine (DIT).
- Coupling reactions: MIT and DIT residues couple to form T3 and T4 within thyroglobulin
Stages of Thyroid Hormone Synthesis
- Thyroid hormones remain within thyroglobulin until needed.
- During release, colloid is internalized by thyrocytes via endocytosis
- Peptide bonds within thyroglobulin are hydrolysed, releasing T3 and T4
Thyroid Hormone Transport and Metabolism
- Thyroid hormones are transported by proteins in the blood (thyroxine-binding globulin, prealbumin, albumin)
- Most T4 is converted to T3 in peripheral tissues, making T3 the more active form
- T4 has a longer half-life than T3
- Degradation occurs in muscles, liver, and kidneys through deiodination
Regulation of Thyroid Hormone Secretion
- Thyrotropin-releasing hormone (TRH) from the hypothalamus stimulates the release of thyroid-stimulating hormone (TSH) from the anterior pituitary
- Thyroid hormones exert negative feedback control on the release of TRH and TSH, maintaining homeostasis
- TSH is a crucial factor in regulating thyroid hormone synthesis and release
Function of Thyroid Hormones
- Basal Metabolic Rate (BMR): Thyroid hormones increase metabolic activity in most tissues
- Protein Metabolism: Thyroid hormones increase protein synthesis and breakdown
- Carbohydrate Metabolism: Thyroid hormones increase glucose uptake and glycogen breakdown
- Fat Metabolism: Thyroid hormones mobilize fat, decreasing storage and increasing free fatty acid levels
- Growth and Development: Essential for normal development, especially of the brain
- Body Temperature: Thyroid hormones increase body temperature, leading to heat production
- Cardiovascular System: Thyroid hormones increase heart rate and force of contraction
- Sleep: Normal thyroxine levels are necessary to maintain normal sleep patterns
- Sexual Function: Thyroid hormones are crucial for normal sexual function in both men and women
- Other Endocrine Glands: Thyroxine increases the demand for secretion from other endocrine glands
- Gastrointestinal Tract: Thyroxine increases secretions and movements of the gastrointestinal tract.
- Central Nervous System: Essential for normal development and function of the central nervous system (CNS).
- Skeletal Muscle: Essential for normal activity of skeletal muscles
- Respiration: Thyroid hormones increase respiration indirectly by increasing the body's demand for oxygen and carbon dioxide
Thyroid Function Tests
- T3 and T4 levels, TSH levels
Interpretation of Thyroid Function Tests (TSH, T4, T3)
- Results vary depending on abnormalities of the thyroid gland (primary, subclinical, central hypo/hyperthyroidism)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the essential aspects of the thyroid gland's physiology and histology. It delves into the structure, function, hormone synthesis, and significance of iodide and thyroglobulin. Ideal for those studying human anatomy and endocrinology.