Podcast
Questions and Answers
What substance is critical for the synthesis of thyroid hormones?
What substance is critical for the synthesis of thyroid hormones?
Which thyroid hormone has a longer half-life in the blood?
Which thyroid hormone has a longer half-life in the blood?
What is the primary hormone responsible for stimulating the production of T3 and T4 in the thyroid?
What is the primary hormone responsible for stimulating the production of T3 and T4 in the thyroid?
Which cells in the thyroid gland are responsible for producing thyroid hormones?
Which cells in the thyroid gland are responsible for producing thyroid hormones?
Signup and view all the answers
What is a major source from which T3 is predominantly produced in the body?
What is a major source from which T3 is predominantly produced in the body?
Signup and view all the answers
Which thyroid function test is considered the most useful in evaluating thyroid function?
Which thyroid function test is considered the most useful in evaluating thyroid function?
Signup and view all the answers
How does an increase in T3 and T4 levels affect TSH secretion?
How does an increase in T3 and T4 levels affect TSH secretion?
Signup and view all the answers
What is the approximate dietary intake of iodide required to maintain thyroid function in adults?
What is the approximate dietary intake of iodide required to maintain thyroid function in adults?
Signup and view all the answers
What is the recommended first-line treatment for Graves's disease?
What is the recommended first-line treatment for Graves's disease?
Signup and view all the answers
What characterizes factitious thyrotoxicosis?
What characterizes factitious thyrotoxicosis?
Signup and view all the answers
Which condition is associated with activating mutations in the TSH receptor gene?
Which condition is associated with activating mutations in the TSH receptor gene?
Signup and view all the answers
What finding is expected on a thyroid uptake scan for a patient with a toxic nodule?
What finding is expected on a thyroid uptake scan for a patient with a toxic nodule?
Signup and view all the answers
What defines subclinical hyperthyroidism?
What defines subclinical hyperthyroidism?
Signup and view all the answers
Why is it important to normalize thyroid hormone levels before radioactive iodine treatment?
Why is it important to normalize thyroid hormone levels before radioactive iodine treatment?
Signup and view all the answers
What is a common risk factor for patients with toxic adenoma when exposed to iodine excess?
What is a common risk factor for patients with toxic adenoma when exposed to iodine excess?
Signup and view all the answers
What symptom may indicate a particularly large goiter with compressive symptoms?
What symptom may indicate a particularly large goiter with compressive symptoms?
Signup and view all the answers
How long after hospitalization should thyroid function tests be repeated in a clinically euthyroid patient?
How long after hospitalization should thyroid function tests be repeated in a clinically euthyroid patient?
Signup and view all the answers
What percentage of patients receiving amiodarone can develop hypothyroidism or thyrotoxicosis?
What percentage of patients receiving amiodarone can develop hypothyroidism or thyrotoxicosis?
Signup and view all the answers
Which class of thyrotoxicosis is characterized by iodine-induced excess thyroid hormone synthesis?
Which class of thyrotoxicosis is characterized by iodine-induced excess thyroid hormone synthesis?
Signup and view all the answers
Which treatment is effective for type II thyrotoxicosis caused by amiodarone?
Which treatment is effective for type II thyrotoxicosis caused by amiodarone?
Signup and view all the answers
In pregnant women, TSH screening is indicated for which of the following groups?
In pregnant women, TSH screening is indicated for which of the following groups?
Signup and view all the answers
What is the typical initial treatment for severe cases of thyrotoxicosis?
What is the typical initial treatment for severe cases of thyrotoxicosis?
Signup and view all the answers
What is the effect of increased estrogen levels during pregnancy on thyroxine-binding globulin?
What is the effect of increased estrogen levels during pregnancy on thyroxine-binding globulin?
Signup and view all the answers
What is the main treatment for hypothyroidism in patients taking amiodarone?
What is the main treatment for hypothyroidism in patients taking amiodarone?
Signup and view all the answers
In post-partum thyroiditis, what laboratory finding is typically present?
In post-partum thyroiditis, what laboratory finding is typically present?
Signup and view all the answers
At what week of gestation does fetal thyroid tissue become functional?
At what week of gestation does fetal thyroid tissue become functional?
Signup and view all the answers
Which of the following is a common precipitating factor for thyroid storm?
Which of the following is a common precipitating factor for thyroid storm?
Signup and view all the answers
How is thyroid storm generally diagnosed?
How is thyroid storm generally diagnosed?
Signup and view all the answers
What is the expected fate of most women who experience post-partum thyroiditis?
What is the expected fate of most women who experience post-partum thyroiditis?
Signup and view all the answers
Which of the following treatments is recommended to inhibit the release of T4 and T3 during thyroid storm?
Which of the following treatments is recommended to inhibit the release of T4 and T3 during thyroid storm?
Signup and view all the answers
What symptom is most commonly associated with thyroid storm?
What symptom is most commonly associated with thyroid storm?
Signup and view all the answers
What is the role of antithyroid drugs in cases of impaired thyroid hormone synthesis?
What is the role of antithyroid drugs in cases of impaired thyroid hormone synthesis?
Signup and view all the answers
What is the characteristic temperature indicative of hypothermia in myxedema coma?
What is the characteristic temperature indicative of hypothermia in myxedema coma?
Signup and view all the answers
Which of the following is a common mental status change associated with myxedema coma?
Which of the following is a common mental status change associated with myxedema coma?
Signup and view all the answers
What is the initial treatment for suspected adrenal insufficiency in a patient with myxedema coma?
What is the initial treatment for suspected adrenal insufficiency in a patient with myxedema coma?
Signup and view all the answers
Which condition is NOT a precipitating event for myxedema coma?
Which condition is NOT a precipitating event for myxedema coma?
Signup and view all the answers
Which laboratory test is crucial to differentiate between euthyroid sick syndrome and overt thyroid dysfunction?
Which laboratory test is crucial to differentiate between euthyroid sick syndrome and overt thyroid dysfunction?
Signup and view all the answers
What type of supportive care is commonly administered to patients with myxedema coma?
What type of supportive care is commonly administered to patients with myxedema coma?
Signup and view all the answers
What is a key clinical manifestation typically present in myxedema coma?
What is a key clinical manifestation typically present in myxedema coma?
Signup and view all the answers
Which treatment method is an alternative to intravenous levothyroxine in myxedema coma management?
Which treatment method is an alternative to intravenous levothyroxine in myxedema coma management?
Signup and view all the answers
What is the most common cause of thyrotoxicosis?
What is the most common cause of thyrotoxicosis?
Signup and view all the answers
Which symptom is NOT commonly associated with thyrotoxicosis?
Which symptom is NOT commonly associated with thyrotoxicosis?
Signup and view all the answers
Which investigation is part of the first-line tests for diagnosing thyrotoxicosis?
Which investigation is part of the first-line tests for diagnosing thyrotoxicosis?
Signup and view all the answers
What percentage of cases of thyrotoxicosis is accounted for by solitary thyroid adenoma?
What percentage of cases of thyrotoxicosis is accounted for by solitary thyroid adenoma?
Signup and view all the answers
Which sign is commonly seen in a patient with thyrotoxicosis?
Which sign is commonly seen in a patient with thyrotoxicosis?
Signup and view all the answers
Which of the following is least likely to cause thyrotoxicosis?
Which of the following is least likely to cause thyrotoxicosis?
Signup and view all the answers
What percentage of thyrotoxicosis cases is attributed to drugs like amiodarone?
What percentage of thyrotoxicosis cases is attributed to drugs like amiodarone?
Signup and view all the answers
Which of the following symptoms reflects the neuromuscular effects of thyrotoxicosis?
Which of the following symptoms reflects the neuromuscular effects of thyrotoxicosis?
Signup and view all the answers
Which of the following is a reproductive symptom of thyrotoxicosis?
Which of the following is a reproductive symptom of thyrotoxicosis?
Signup and view all the answers
Which of the following is a less common cause of thyrotoxicosis?
Which of the following is a less common cause of thyrotoxicosis?
Signup and view all the answers
Study Notes
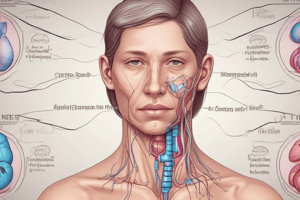
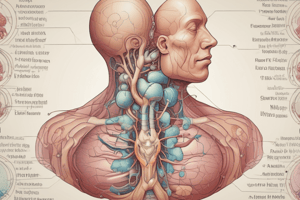
Thyroid Anatomy and Physiology
- The thyroid gland consists of two lobes connected by a midline isthmus
- Each lobe usually measures up to 5cm in length, 2cm in width, and 2cm in depth
- The entire gland weighs 10-20 grams
- Histologically, the gland contains two cell types: parafollicular C cells and follicular epithelial cells
- Parafollicular C cells secrete calcitonin, not significant in humans
- Follicular epithelial cells synthesize thyroid hormones by incorporating iodine into the amino acid tyrosine on the surface of thyroglobulin (Tg)
- Iodine is crucial for thyroid hormone production, requiring a daily intake exceeding 100µg for adults
- The thyroid primarily produces thyroxine (T4) and a smaller amount of triiodothyronine (T3)
- Around 85% of circulating T3 comes from the conversion of T4 in tissues
- T4 has a longer half-life than T3 (approximately 1 week vs. 18 hours)
- T3 and T4 circulate mostly bound to carrier proteins (TBG), with free hormones diffusing into tissues
- Thyroid hormone production is stimulated by thyrotropin (TSH), a glycoprotein from the anterior pituitary
- TSH release is regulated by thyrotropin-releasing hormone (TRH) from the hypothalamus
- Thyroid hormones negatively feedback on the hypothalamus and pituitary, suppressing TSH secretion in thyrotoxicosis
- TSH is the most helpful indicator of thyroid function
Disorders of the Thyroid Gland
- Thyrotoxicosis: excess thyroid hormone from various causes, often referred to as hyperthyroidism when caused by gland overactivity
- Graves' disease: a common cause of hyperthyroidism, characterized by an autoimmune attack on the thyroid
- Multinodular goiter: multiple nodules within the gland contributing to overactive hormone production
- Solitary thyroid adenoma: a single overactive nodule
- Thyroiditis: inflammation of the thyroid gland, potentially leading to hormone imbalance
- Post-partum thyroiditis: thyroiditis occurring after childbirth, involving a transient thyrotoxic phase
- Subacute (De Quervain's) thyroiditis: inflammation of the thyroid gland, often associated with pain and fever
- lodine-induced: excessive iodine intake can affect thyroid function
- Drug-induced: certain medications can trigger thyroid issues
- Factitious thyrotoxicosis: deliberate intake of thyroid hormone
- Toxic adenoma/multinodular goiter: nodules producing excess thyroid hormone
- Subclinical hyperthyroidism: suppressed TSH level but normal T3 and T4 levels, often asymptomatic
Investigations in Thyroid Diseases
- Thyroid function tests (T3, T4, TSH): assessing thyroid hormone levels for evaluating thyroid conditions.
- Thyroid autoantibodies (Anti-TPO and Anti-TSH): checking for autoimmune thyroid disease, typically used for detecting potential issues.
- Imaging (US, CT, PET): visual evaluation of the gland for size, structure, and presence of nodules, used in investigating thyroid conditions.
- Radioactive iodine uptake (RAIU): a test measuring iodine uptake by the thyroid over time, evaluating the cause of hyperthyroidism.
- Tissue biopsy (histopathological): examining tissue samples for determining the underlying cause of a problem
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the anatomy and physiology of the thyroid gland. This quiz covers the structure, function, and hormonal production details, including the significance of iodine and the types of cells involved. Challenge yourself with key concepts related to thyroid health.