Podcast
Questions and Answers
What primarily replaces neutrophils during the tissue repair process?
What primarily replaces neutrophils during the tissue repair process?
Which component is not listed as part of the composition of avascular scar tissue?
Which component is not listed as part of the composition of avascular scar tissue?
What is the main contributor to wound contraction in large surface wounds?
What is the main contributor to wound contraction in large surface wounds?
What characterizes lamellar bone compared to woven bone?
What characterizes lamellar bone compared to woven bone?
Signup and view all the answers
In the process of fracture healing, which stage follows hematoma formation?
In the process of fracture healing, which stage follows hematoma formation?
Signup and view all the answers
Which process is specifically associated with the formation of granulation tissue?
Which process is specifically associated with the formation of granulation tissue?
Signup and view all the answers
What is a characteristic change during the scar formation process?
What is a characteristic change during the scar formation process?
Signup and view all the answers
What is the primary type of tissue responsible for repairing a fracture?
What is the primary type of tissue responsible for repairing a fracture?
Signup and view all the answers
What is the primary role of macrophages during the demolition stage of fracture healing?
What is the primary role of macrophages during the demolition stage of fracture healing?
Signup and view all the answers
What type of tissue formation occurs following the demolition phase in fracture healing?
What type of tissue formation occurs following the demolition phase in fracture healing?
Signup and view all the answers
During the formation of woven bone or cartilage, what is the term used to describe the material uniting the fracture ends?
During the formation of woven bone or cartilage, what is the term used to describe the material uniting the fracture ends?
Signup and view all the answers
Which cell type is primarily responsible for laying down osteoid during lamellar bone formation?
Which cell type is primarily responsible for laying down osteoid during lamellar bone formation?
Signup and view all the answers
What is the significance of Haversian systems in lamellar bone?
What is the significance of Haversian systems in lamellar bone?
Signup and view all the answers
What processes characterize the remodeling stage of fracture healing?
What processes characterize the remodeling stage of fracture healing?
Signup and view all the answers
What can happen to detached bone fragments during the demolition stage?
What can happen to detached bone fragments during the demolition stage?
Signup and view all the answers
Which layer is primarily involved in the osteogenic potential during granulation tissue formation?
Which layer is primarily involved in the osteogenic potential during granulation tissue formation?
Signup and view all the answers
What is the primary feature of wound healing by first intention?
What is the primary feature of wound healing by first intention?
Signup and view all the answers
What role do myofibroblasts play in wound healing?
What role do myofibroblasts play in wound healing?
Signup and view all the answers
Which phase occurs first in the healing by first intention process?
Which phase occurs first in the healing by first intention process?
Signup and view all the answers
By which day does granulation tissue begin to invade the incision space?
By which day does granulation tissue begin to invade the incision space?
Signup and view all the answers
What characterizes the scar formation process after one month of healing?
What characterizes the scar formation process after one month of healing?
Signup and view all the answers
Which of the following occurs during the thickening of the epidermis?
Which of the following occurs during the thickening of the epidermis?
Signup and view all the answers
What is the typical outcome of inadequate contraction during wound healing?
What is the typical outcome of inadequate contraction during wound healing?
Signup and view all the answers
What changes occur in the vascularity of a healing wound by two weeks?
What changes occur in the vascularity of a healing wound by two weeks?
Signup and view all the answers
Study Notes
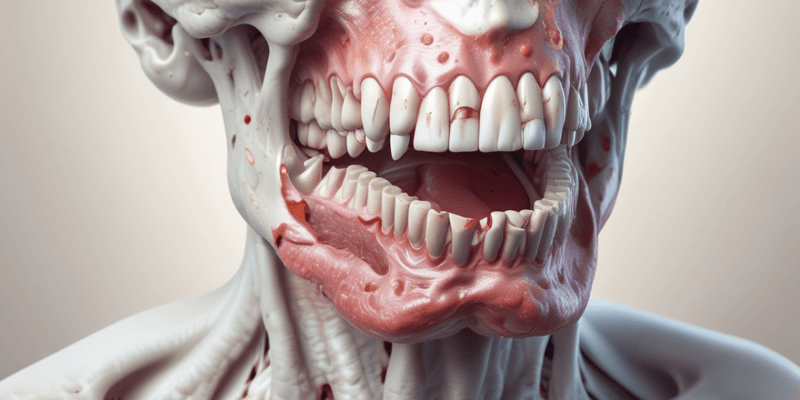
Pathology Lecture 4: Wound Healing
- Wound healing is the body's replacement of destroyed tissue by living tissue.
Phases of Wound Healing
- Inflammatory Phase (a): Initial response to injury. Involves clotting, inflammation, and removal of debris.
- Proliferative Phase (b): New tissue formation. Fibroblasts create new tissue, and blood vessels grow (angiogenesis). Epithelial cells cover the wound.
- Remodeling Phase (c): Maturation and scar formation. Collagen is remodeled, and the scar tissue matures. The wound closes completely.
Types of Tissues
- Labile cells: Rapidly divide and replace lost tissue (e.g., surface epithelium of the GI tract, urinary tract, and skin; cells of the lymphoid and hematopoietic systems)
- Stable cells: Have a lower rate of replication but maintain the capacity to divide (e.g., mesenchymal cells, smooth muscle cells, fibroblasts, osteoblasts, and endothelial cells; liver, endocrine glands, and renal tubular epithelium)
- Permanent cells: Do not divide, and lost cells are not replaced (e.g., adult neurons, striated muscle cells, and lens cells)
Wound Healing Processes
- Regeneration: Replacement of lost tissue by identical tissue cells
- Repair (scarring): Replacement of lost tissue with granulation tissue and scar tissue.
Types of Wounds
- Closed: Skin surface remains intact; underlying tissues are damaged. (e.g., contusions, hematomas, Stage 1 pressure ulcers).
- Open: Skin is broken, and underlying tissues are exposed to the environment.
Objectives of Wound Healing
- Restoration of an intact epithelial surface.
- Restoration of tensile strength of the subepithelial tissue.
Stages of Primary Union (Healing by First Intention)
- 24 hours: Neutrophils invade incision site and migrate toward the clot. Basal cells proliferate.
- 24-48 hours: Epithelial cells accumulate. Basement membranes form. A thin continuous epithelial layer forms beneath the scab.
- 3rd day: Macrophages replace neutrophils. Granulation tissue invades the incision area. Collagen fibers appear at the margins. Epithelial proliferation continues.
- 5th day: Granulation tissue fills the space. Blood vessel supply is optimal. The normal epidermal thickness is restored. Surface cells differentiate and keratinize.
- Two weeks: Continued collagen accumulation. Decreased leukocyte infiltrate. Edema resorbs. Reduced vascularity. Increased collagen deposition.
- One month: Scar tissue formation is prominent, with the epidermal layer being intact. Inflammatory infiltrate is absent.
- Consequences include loss of dermal and epidermal appendages, and healing of tensile strength may take months.
Stages of Secondary Union (Healing by Second Intention)
- Haematoma Formation (Stage 1): Variable bleeding after injury. Blood extends to surrounding muscles. If ossified, myositis ossificans results.
- Inflammation (Stage 2): Tissue damage triggers inflammatory response, causing edema and polymorphonuclear leukocyte infiltration. Blood flow is increased.
- Demolition (Stage 3): Macrophages remove the clot, inflammatory exudate, and debris. Detached pieces of bone undergo necrosis and are broken down by macrophages and osteoclasts.
- Granulation Tissue Formation (Stage 4): Newly formed capillaries, fibroblasts, and mesenchymal cells migrate from the periosteum and endosteum. This forms granulation tissue and contributes to tissue formation.
- Woven Bone/Cartilage Formation (Stage 5): Osteoblasts differentiate to form either woven bone or cartilage. This is the "callus" in fractured bone contexts. The callus begins as soft tissues to harden to bone over time.
- Lamellar Bone Formation (Stage 6): Dead cartilage or woven bone are replaced bone with orderly arrangement of collagen bundles concentrically around blood vessels resembling the Haversian systems.
- Remodeling (Stage 7): Osteoclasts remove external callus as osteoblasts form new bone. Internal callus converts to compact bone.
Factors Influencing Wound Healing
- Local factors: Type, size, location of the wound; vascular supply (e.g., wounds with impaired blood supply or presence of pressure ulcers heal more slowly); infection; movement (e.g. early motion prevents or delays healing) ; Ionizing radiation
- Systemic factors: Circulatory status; infection; metabolic status (e.g. diabetes); nutritional deficiencies; medication (e.g. aspirin, or indomethacin)
Complications of Wound Healing
- Infection: Wounds can provide a portal of entry for microorganisms, delaying or stopping healing.
- Deficient scar formation: Inadequate granulation tissue formation or ECM not being maintained can result in deficient scar. This can result in complications such as dehiscence, hernias, or ulcerations.
- Excessive scar formation (hypertrophic and keloid scars): Excessive deposition of extracellular matrix.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the essential phases of wound healing including the inflammatory, proliferative, and remodeling phases. Additionally, it explores different types of tissues involved in the healing process. Test your knowledge of these critical concepts in pathology.