Podcast
Questions and Answers
What is the primary reason for the interdependence of the outputs of the left and right ventricles?
What is the primary reason for the interdependence of the outputs of the left and right ventricles?
- Both ventricles pump blood into the same circulatory system. (correct)
- Right ventricle output is unaffected by left ventricle performance.
- The atria control the output of each ventricle independently.
- The left ventricle regulates blood flow to the aorta exclusively.
Which of the following factors does NOT affect vascular resistance?
Which of the following factors does NOT affect vascular resistance?
- Platelet count (correct)
- Blood viscosity
- Vessel length
- Vessel diameter
Which aspect of cardiac physiology is primarily responsible for generating the pressure needed for blood flow?
Which aspect of cardiac physiology is primarily responsible for generating the pressure needed for blood flow?
- Pacemaker cell activity
- Cardiac muscle elasticity
- Cardiac output variability
- Interventricular pressure differences (correct)
Which of the following best describes the function of hemodynamics in the cardiovascular system?
Which of the following best describes the function of hemodynamics in the cardiovascular system?
Which statement about the cardiac cycle is accurate?
Which statement about the cardiac cycle is accurate?
Where is the site of highest vascular resistance in the systemic circulation?
Where is the site of highest vascular resistance in the systemic circulation?
What happens to mean arterial pressure if both cardiac output and total peripheral resistance (TPR) increase?
What happens to mean arterial pressure if both cardiac output and total peripheral resistance (TPR) increase?
Which factor contributes to blood viscosity the most?
Which factor contributes to blood viscosity the most?
How does blood pressure change as it flows through the systemic vasculature?
How does blood pressure change as it flows through the systemic vasculature?
What effect does anemia have on blood flow?
What effect does anemia have on blood flow?
What does compliance refer to in the context of blood vessels?
What does compliance refer to in the context of blood vessels?
Which condition would likely slow down blood flow due to increased viscosity?
Which condition would likely slow down blood flow due to increased viscosity?
What primarily causes blood pressure to decline as it moves from arteries to veins?
What primarily causes blood pressure to decline as it moves from arteries to veins?
What is the primary purpose of the long refractory period in cardiac muscle tissue?
What is the primary purpose of the long refractory period in cardiac muscle tissue?
Which of the following is NOT a variable associated with the cardiac cycle?
Which of the following is NOT a variable associated with the cardiac cycle?
How does myocardial contractility affect stroke volume in the presence of increased afterload?
How does myocardial contractility affect stroke volume in the presence of increased afterload?
In what way does Starling's law help maintain cardiac output?
In what way does Starling's law help maintain cardiac output?
What effect does increased heart rate have on stroke volume, according to the reciprocal relationship in cardiac output?
What effect does increased heart rate have on stroke volume, according to the reciprocal relationship in cardiac output?
Which factor is primarily altered to affect cardiac output through ventricular filling changes?
Which factor is primarily altered to affect cardiac output through ventricular filling changes?
Which statement about preload and afterload is accurate in the context of contractility?
Which statement about preload and afterload is accurate in the context of contractility?
Which of the following statements accurately describes hemodynamic variables associated with the cardiac cycle?
Which of the following statements accurately describes hemodynamic variables associated with the cardiac cycle?
What mechanism is responsible for contraction in cardiac muscle?
What mechanism is responsible for contraction in cardiac muscle?
Which structure acts as the normal pacemaker of the heart?
Which structure acts as the normal pacemaker of the heart?
What is the typical resting heart rate of a person with enhanced parasympathetic tone, like that of an endurance athlete?
What is the typical resting heart rate of a person with enhanced parasympathetic tone, like that of an endurance athlete?
What happens if the SA node fails or transmission to the AV node fails?
What happens if the SA node fails or transmission to the AV node fails?
Which statement about cardiac action potentials is true?
Which statement about cardiac action potentials is true?
What could happen due to arrhythmias in the heart?
What could happen due to arrhythmias in the heart?
What is the intrinsic firing rate of the SA node under normal conditions?
What is the intrinsic firing rate of the SA node under normal conditions?
If the ventricular rate is excessive, what is the main consequence?
If the ventricular rate is excessive, what is the main consequence?
What does the cardiac cycle specifically refer to?
What does the cardiac cycle specifically refer to?
In terms of the cardiac cycle, what do the terms systole and diastole primarily refer to?
In terms of the cardiac cycle, what do the terms systole and diastole primarily refer to?
Which of the following statements about stroke volume (SV) is correct?
Which of the following statements about stroke volume (SV) is correct?
What is the average cardiac output (CO) for an adult?
What is the average cardiac output (CO) for an adult?
Which factor can decrease cardiac output (CO)?
Which factor can decrease cardiac output (CO)?
What determines ejection fraction?
What determines ejection fraction?
What is the relationship between the electrical events and mechanical events in the cardiac cycle?
What is the relationship between the electrical events and mechanical events in the cardiac cycle?
Which measurement can be used to assess cardiac performance?
Which measurement can be used to assess cardiac performance?
Flashcards are hidden until you start studying
Study Notes
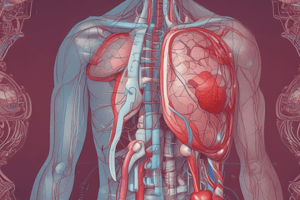
Cardiovascular System Overview
- The cardiovascular system is central to medical physiology, focusing on hemodynamics and the functional organization of blood flow.
- The outputs of the left and right ventricles are interdependent, highlighting their collaborative function in blood circulation.
Hemodynamics
- Mean arterial pressure is influenced by cardiac output and total peripheral resistance (TPR).
- Blood pressure decreases as it travels through the circulatory system, with the largest drop occurring across arterioles due to high vascular resistance.
Factors Affecting Blood Flow
- Vessel length impacts blood pressure; longer vessels result in greater pressure loss due to friction.
- Blood viscosity is affected primarily by red blood cell count and albumin concentration, influencing flow rates under various conditions (e.g., anemia vs. polycythemia).
- Compliance refers to the distensibility of blood vessels; low compliance means a minimal volume change for a given pressure change.
Cardiac Electrophysiology
- The sinoatrial (SA) node serves as the primary pacemaker, firing at about 100 beats/min, moderated to around 70 beats/min due to parasympathetic tone.
- The atrioventricular (AV) node can act as a backup pacemaker in case the SA node fails, often resulting in a slower heart rate.
Cardiac Cycle
- The cardiac cycle consists of systole (contraction) and diastole (relaxation) phases, with electrical events always preceding mechanical actions.
- Mechanical events correlate with ECG waves, illustrating the relationship between electrical signals and heart muscle contraction.
Cardiac Output and Stroke Volume
- Cardiac output (CO) is calculated as the product of heart rate (HR) and stroke volume (SV), averaging around 5 L/min in adults.
- Stroke volume is determined by the difference between end-diastolic volume (EDV) and end-systolic volume (ESV).
Ejection Fraction
- Ejection fraction measures the percentage of blood ejected from the ventricles during contraction, indicating ventricular performance.
Regulatory Mechanisms
- Calcium regulatory mechanisms in myocardial cells affect the inotropic state, influencing the strength of cardiac contractions.
- Frank-Starling principle illustrates how changes in preload and afterload impact cardiac output and overall heart function.
Refractory Periods
- Cardiac action potentials feature long refractory periods, preventing tetany and ensuring adequate filling time during diastole.
Summary of Key Factors
- Understanding the dynamics of blood flow, pressure, and heart function is essential for comprehending cardiovascular physiology.
- Knowledge of how various parameters like vessel length, viscosity, and compliance influence hemodynamics is critical for medical practice.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.