Podcast
Questions and Answers
What is the primary cause of Raynaud's phenomenon?
What is the primary cause of Raynaud's phenomenon?
- Restricted blood flow (correct)
- Increased blood flow
- Nerve damage
- Blood vessel inflammation
Which of the following is a characteristic clinical manifestation of dermatomyositis?
Which of the following is a characteristic clinical manifestation of dermatomyositis?
- Decreased skin pigmentation
- Muscle weakness (correct)
- Increased appetite
- Increased joint mobility
Which of the following is a type of systemic vasculitis?
Which of the following is a type of systemic vasculitis?
- Systemic lupus erythematosus
- Giant cell arteritis (correct)
- Rheumatoid arthritis
- Sjögren's syndrome
What is the primary cause of the skin turning blue in Raynaud's phenomenon?
What is the primary cause of the skin turning blue in Raynaud's phenomenon?
Which of the following is a key feature of the pathology of systemic vasculitides?
Which of the following is a key feature of the pathology of systemic vasculitides?
What is the most common autoantibody associated with dermatomyositis?
What is the most common autoantibody associated with dermatomyositis?
Which of the following is NOT a common systemic symptom of dermatomyositis?
Which of the following is NOT a common systemic symptom of dermatomyositis?
What type of immune cells are involved in the pathogenesis of dermatomyositis?
What type of immune cells are involved in the pathogenesis of dermatomyositis?
What is the key difference between dermatomyositis and polymyositis?
What is the key difference between dermatomyositis and polymyositis?
Which of the following is a common manifestation of dermatomyositis related to the joints?
Which of the following is a common manifestation of dermatomyositis related to the joints?
What is the significance of anti-P155/P140 antibodies in dermatomyositis?
What is the significance of anti-P155/P140 antibodies in dermatomyositis?
What is the cause of polymyositis in adults according to the text?
What is the cause of polymyositis in adults according to the text?
Which type of T cells are thought to directly injure myocytes in polymyositis?
Which type of T cells are thought to directly injure myocytes in polymyositis?
In polymyositis, where are CD8+ T cells mainly located?
In polymyositis, where are CD8+ T cells mainly located?
What is a common factor leading to delayed medical advice seeking in patients with DM & PM?
What is a common factor leading to delayed medical advice seeking in patients with DM & PM?
How are systemic vasculitides classified based on according to the text?
How are systemic vasculitides classified based on according to the text?
Which type of cells are typically found in the inflammatory infiltrate of Kawasaki disease?
Which type of cells are typically found in the inflammatory infiltrate of Kawasaki disease?
Which of the following is a common complication of Kawasaki disease if left untreated?
Which of the following is a common complication of Kawasaki disease if left untreated?
What is the primary cause of Buerger's disease/thromboangiitis obliterans?
What is the primary cause of Buerger's disease/thromboangiitis obliterans?
What is the primary risk factor for developing Buerger's disease?
What is the primary risk factor for developing Buerger's disease?
Which of the following is a characteristic histological feature of the small vessel vasculitides?
Which of the following is a characteristic histological feature of the small vessel vasculitides?
Which type of ANCA is typically associated with granulomatosis with polyangiitis (Wegener's)?
Which type of ANCA is typically associated with granulomatosis with polyangiitis (Wegener's)?
Which of the following is a characteristic clinical feature of granulomatosis with polyangiitis (Wegener's)?
Which of the following is a characteristic clinical feature of granulomatosis with polyangiitis (Wegener's)?
Which of the following is a key histological feature of eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)?
Which of the following is a key histological feature of eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)?
Which of the following is a common clinical manifestation of eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)?
Which of the following is a common clinical manifestation of eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)?
Which of the following is a common treatment approach for the small vessel vasculitides?
Which of the following is a common treatment approach for the small vessel vasculitides?
Which of the following is a characteristic clinical manifestation of Granulomatosis with Polyangiitis (GPA)?
Which of the following is a characteristic clinical manifestation of Granulomatosis with Polyangiitis (GPA)?
Which of the following is a key feature of Henoch-Schönlein Purpura (HSP)?
Which of the following is a key feature of Henoch-Schönlein Purpura (HSP)?
Which of the following is a common clinical presentation of Henoch-Schönlein Purpura (HSP)?
Which of the following is a common clinical presentation of Henoch-Schönlein Purpura (HSP)?
Which of the following is a characteristic of Granulomatosis with Polyangiitis (GPA)?
Which of the following is a characteristic of Granulomatosis with Polyangiitis (GPA)?
Which of the following is a common treatment approach for Granulomatosis with Polyangiitis (GPA)?
Which of the following is a common treatment approach for Granulomatosis with Polyangiitis (GPA)?
Which of the following is a characteristic of Henoch-Schönlein Purpura (HSP)?
Which of the following is a characteristic of Henoch-Schönlein Purpura (HSP)?
Study Notes
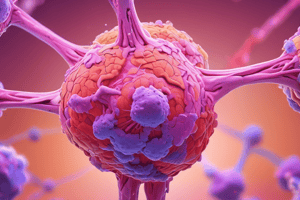
Inflammatory Myopathies
- Dermatomyositis (DM) and Polymyositis (PM) are inflammatory myopathies
- DM:
- Characterized by skin manifestations, including mechanic's hand, Gottron's papules, and heliotrope rash
- May also have systemic symptoms such as fever, malaise, weight loss, and Raynaud's phenomenon
- Can lead to malignant tumors in adults
- Autoantibodies: ANA, anti-Mi2, anti-helicase, anti-Jo1, and anti-P155/P140
- PM:
- Characterized by bilateral proximal muscle weakness, similar to DM but without a rash
- Cause is unknown, may involve viruses and autoimmune factors
- Different pathogenesis: CD8+ cytotoxic T cells probably directly injuring myocytes
- Anti-Jo1 in 20% of patients, poor prognosis with interstitial lung disease
Systemic Vasculitides
- Classification based on the size of the vessels involved
- Large vessel vasculitis:
- Takayasu arteritis
- Medium vessel vasculitis:
- Kawasaki disease
- Buerger's disease/thromboangiitis obliterans
- Small vessel vasculitis:
- ANCA-associated vasculitides:
- Microscopic polyangiitis
- Granulomatosis with polyangiitis (Wegener's granulomatosis)
- Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)
- IgA vasculitis (Henoch-Schonlein purpura)
- ANCA-associated vasculitides:
Kawasaki Disease
- Mucocutaneous lymph node syndrome
- Acute febrile illness in infants and children (< 4 years)
- Mucocutaneous symptoms and cervical lymph node enlargement
- Treatment: IVIG
Buerger's Disease/Thromboangiitis Obliterans
- Affects medium and small vessels
- Heavy smokers, males, 20-40 years
- Pathogenesis: Clots in vessels supplying fingers and toes
- Patients develop ulcers on fingers and toes, often co-exists with Raynaud's phenomenon
- Treatment: Smoking cessation
Small Vessel Vasculitides
- Microscopic polyangiitis:
- Leukocytoclastic or hypersensitivity vasculitis
- Transmural, necrotizing vasculitis
- Organs involved: skin, mucous membranes, lungs, GI, kidneys, heart, and brain
- Treatment: glucocorticoids, cyclophosphamide
- Granulomatosis with polyangiitis/Wegener's granulomatosis:
- Classical clinical triad: kidney, nasopharynx, and lungs
- Biopsy: focal necrotizing vasculitis, granulomatous change, and PR3-ANCA positive
- Rapidly fatal if left untreated
- Treatment: glucocorticoids, cyclophosphamide
- Eosinophilic granulomatosis with polyangiitis/Churg-Strauss syndrome:
- Necrotizing vasculitis, granulomatous vasculitis
- Strongly associated with asthma, eosinophilia, and pulmonary infiltrates
- Supportive therapy and glucocorticoids
- Henoch-Schonlein purpura:
- IgA antibodies directly target endothelial cells
- Small vessel IgA and immune complex-mediated vasculitis
- Presentation: skin lesions on buttocks and leg, progressing from blanching macules to petechiae to palpable purpura
- Diagnosis: clinical, as lab results often normal
- Treatment: supportive therapy, +/- corticosteroids for GI symptoms
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on inflammatory myopathies, systemic vasculitides, and Raynaud's phenomenon. Learn about the changes in skin color due to restricted blood flow and vascular reactions.