Podcast
Questions and Answers
What is NOT a known cause or contributing factor of the condition discussed?
What is NOT a known cause or contributing factor of the condition discussed?
Which symptom is always present in cases of this condition?
Which symptom is always present in cases of this condition?
In which timeframe is a patient typically expected to become wheelchair dependent?
In which timeframe is a patient typically expected to become wheelchair dependent?
Which variant of ALS is characterized by initial symptoms affecting muscles innervated by cranial nerves?
Which variant of ALS is characterized by initial symptoms affecting muscles innervated by cranial nerves?
Signup and view all the answers
What is the prognosis for patients diagnosed with this condition?
What is the prognosis for patients diagnosed with this condition?
Signup and view all the answers
What is a characteristic of Wallerian degeneration in peripheral nerves?
What is a characteristic of Wallerian degeneration in peripheral nerves?
Signup and view all the answers
What factor reduces the likelihood of a functional connection during nerve regeneration?
What factor reduces the likelihood of a functional connection during nerve regeneration?
Signup and view all the answers
Which statement is true regarding the regeneration of nerves in the peripheral nervous system (PNS)?
Which statement is true regarding the regeneration of nerves in the peripheral nervous system (PNS)?
Signup and view all the answers
What is a significant difference between the central nervous system (CNS) and peripheral nervous system (PNS) regarding regeneration?
What is a significant difference between the central nervous system (CNS) and peripheral nervous system (PNS) regarding regeneration?
Signup and view all the answers
Which of the following factors does NOT influence regeneration of peripheral nerves?
Which of the following factors does NOT influence regeneration of peripheral nerves?
Signup and view all the answers
What is a symptom associated with cauda equina syndrome?
What is a symptom associated with cauda equina syndrome?
Signup and view all the answers
What type of sensory loss is seen below the level of impairment in posterior spinal artery syndrome?
What type of sensory loss is seen below the level of impairment in posterior spinal artery syndrome?
Signup and view all the answers
Which of the following conditions is associated with subacute combined degeneration of the spinal cord?
Which of the following conditions is associated with subacute combined degeneration of the spinal cord?
Signup and view all the answers
In Friedreich’s ataxia, which tract is primarily responsible for unconscious proprioception?
In Friedreich’s ataxia, which tract is primarily responsible for unconscious proprioception?
Signup and view all the answers
What is a characteristic symptom of Tabes Dorsalis?
What is a characteristic symptom of Tabes Dorsalis?
Signup and view all the answers
Which of the following is NOT a symptom of systemic problems affecting the spinal cord?
Which of the following is NOT a symptom of systemic problems affecting the spinal cord?
Signup and view all the answers
Which symptom indicates a lower motor neuron (LMN) problem?
Which symptom indicates a lower motor neuron (LMN) problem?
Signup and view all the answers
What type of atrophy is observed in Friedreich’s ataxia?
What type of atrophy is observed in Friedreich’s ataxia?
Signup and view all the answers
What condition is characterized by the defect of the neural arch allowing for extension of the meninges and cerebrospinal fluid?
What condition is characterized by the defect of the neural arch allowing for extension of the meninges and cerebrospinal fluid?
Signup and view all the answers
Which type of spina bifida does not involve the spinal cord and typically presents with no functional deficits?
Which type of spina bifida does not involve the spinal cord and typically presents with no functional deficits?
Signup and view all the answers
What is the primary symptom of autonomic dysreflexia in individuals with complete lesions above T6?
What is the primary symptom of autonomic dysreflexia in individuals with complete lesions above T6?
Signup and view all the answers
Which structure is affected by polio, leading to muscle weakness without sensory changes?
Which structure is affected by polio, leading to muscle weakness without sensory changes?
Signup and view all the answers
If a patient experiences flaccidity followed by spasticity after a complete transection of the spinal cord, what is the condition likely causing this progression?
If a patient experiences flaccidity followed by spasticity after a complete transection of the spinal cord, what is the condition likely causing this progression?
Signup and view all the answers
What is the primary defect in myelomeningocele compared to other types of spina bifida?
What is the primary defect in myelomeningocele compared to other types of spina bifida?
Signup and view all the answers
What type of spina bifida is characterized as having incidental findings on X-ray, generally presenting with no functional deficits?
What type of spina bifida is characterized as having incidental findings on X-ray, generally presenting with no functional deficits?
Signup and view all the answers
In cases of complete spinal cord transection, which symptoms may NOT be experienced?
In cases of complete spinal cord transection, which symptoms may NOT be experienced?
Signup and view all the answers
Which of the following is a common treatment for autonomic dysreflexia?
Which of the following is a common treatment for autonomic dysreflexia?
Signup and view all the answers
What is the condition characterized by chronic headaches and high blood pressure due to autonomic dysregulation?
What is the condition characterized by chronic headaches and high blood pressure due to autonomic dysregulation?
Signup and view all the answers
When might a surgical repair for myelomeningocele occur?
When might a surgical repair for myelomeningocele occur?
Signup and view all the answers
What is a typical characteristic of post-polio syndrome?
What is a typical characteristic of post-polio syndrome?
Signup and view all the answers
What indicates that Lou Gehrig may have suffered from chronic traumatic encephalopathy?
What indicates that Lou Gehrig may have suffered from chronic traumatic encephalopathy?
Signup and view all the answers
What is NOT a characteristic of complete transection of the spinal cord?
What is NOT a characteristic of complete transection of the spinal cord?
Signup and view all the answers
Which site is primarily affected in diseases such as muscular dystrophy?
Which site is primarily affected in diseases such as muscular dystrophy?
Signup and view all the answers
What characterizes myasthenia gravis at the neuromuscular junction?
What characterizes myasthenia gravis at the neuromuscular junction?
Signup and view all the answers
In myasthenia gravis, which of the following symptoms is commonly observed?
In myasthenia gravis, which of the following symptoms is commonly observed?
Signup and view all the answers
What is the role of acetylcholinesterase in relation to myasthenia gravis?
What is the role of acetylcholinesterase in relation to myasthenia gravis?
Signup and view all the answers
Which statement accurately describes the nerve conduction studies in myasthenia gravis?
Which statement accurately describes the nerve conduction studies in myasthenia gravis?
Signup and view all the answers
What is a major characteristic of lower motor neurons?
What is a major characteristic of lower motor neurons?
Signup and view all the answers
How does muscle weakness from myasthenia gravis vary?
How does muscle weakness from myasthenia gravis vary?
Signup and view all the answers
Which of the following is considered a major site of problems in the context of neuromuscular diseases?
Which of the following is considered a major site of problems in the context of neuromuscular diseases?
Signup and view all the answers
Study Notes
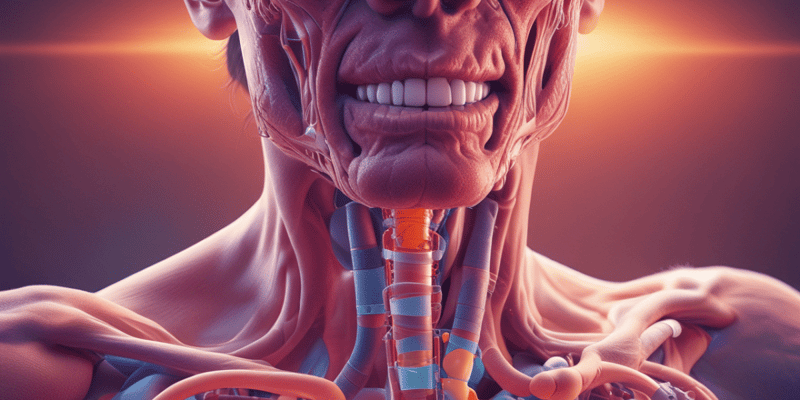
Major Sites of Neurological Issues
- Muscle disorders such as Muscular Dystrophy can occur at various sites including:
- Neuromuscular junction
- Peripheral nerves
- Nerve roots
- Motor neurons
- Spinal cord, with complications including extra-axial and intra-axial lesions, tracts issues, and trauma
- Vascular problems
Motor Unit and Lower Motor Neuron
- Definition of a motor unit includes cell body, axon, neuromuscular junction, and all skeletal muscle fibers it innervates.
- Lower motor neurons consist of the cell body and axon, crucial in muscle activation.
Myasthenia Gravis
- An autoimmune disorder affecting postsynaptic transmission at the NM junction, caused by antibodies against nicotinic acetylcholine receptors.
- Symptoms include fluctuating muscle weakness, particularly in cranial and limb muscles, typically not affecting muscle stretch reflexes (MSRs).
- Nerve conduction studies often remain normal.
Wallerian Degeneration
- Limited regeneration in the PNS compared to the CNS, marked by distal axon atrophy and proximal segment swelling.
- Regeneration mechanisms include regenerative (same axon regrows) and collateral sprouting (nearby axon regrows).
- Regrowth rates are approximately 1 mm per day, depending on factors such as cell body integrity and lesion location.
CNS vs PNS Regeneration
- CNS regeneration is less likely due to factors currently not definitively identified.
- Common risk factors include heavy metal toxicity, smoking, military service, and brain trauma.
- Typical onset of conditions is in males aged 40 to mid-60s.
Symptoms and Prognosis of ALS
- Early symptoms include painless extremity weakness and difficulties with fine motor skills; wasting of hand and foot muscles follows.
- Progression leads to rapid weakness spread, hyperreflexia, and atypical sensory conditions.
- Life expectancy post-diagnosis generally ranges between 3 to 5 years due to respiratory failure or choking from dysphagia.
Variants of ALS
- Progressive Bulbar Palsy: affects muscles innervated by cranial nerves, involving dysarthria and dysphagia.
- Spinal Muscular Atrophy: characterized by lower motor neuron involvement leading to muscle weakness and atrophy.
Role of Physical Therapy (PT)
- Education and support for patients and families are essential; training in maintaining functionality and transfers.
- Use of adaptive devices and wheelchair assistance is advocated; heavy strengthening is not recommended.
Polio and Its Aftereffects
- Affects anterior horn cells with no sensory changes but causes muscle weakness.
- Post-polio syndrome can arise, with considerations for patient safety and recovery strategies.
Disorders of the Spinal Cord
- Conditions include Spina Bifida, complete cord transection, anterior and posterior spinal artery syndromes, and Brown-Sequard syndrome, each having distinct impacts and required treatments.
Types of Spina Bifida
- Spina Bifida Occulta: vertebral defect without nerve involvement, generally asymptomatic.
- Meningocele: involves a bulge of meninges without cord involvement, typically repaired at birth.
- Myelomeningocele: significant involvement of the spinal cord, resulting in severe neurological deficits including paraplegia.
Complete Transection of the Cord
- Initial spinal shock presents as flaccid paralysis, later developing UMN signs like spasticity and hyperreflexia.
- Results in total loss of sensory modalities below the injury level, impacting respiratory function if occurring above the C3 level.
Autonomic Dysreflexia
- A potentially life-threatening condition arising from complete lesions above T6, characterized by exaggerated autonomic responses to noxious stimuli.
- Symptoms include severe headache, high blood pressure, flushing above the lesion, and bradycardia; treatment requires removing the stimulus and positioning the patient correctly.
Cauda Equina Syndrome
- Symptoms include saddle sensory loss and LMN signs like bowel and bladder difficulties, alongside low back pain.
Systemic Problems Affecting the Spinal Cord
- Includes subacute combined degeneration of the spinal cord due to vitamin B12 deficiency, leading to proprioceptive loss, spastic paresis, and urinary incontinence.
Friedreich’s Ataxia
- Genetic condition resulting in motor and proprioceptive dysfunction due to affected CNS tracts.
- Characterized by gait and coordination impairments, upper motor neuron signs, and preservation of some reflexes.
Questions and Discussion Points
- Consideration of case studies or specific patient presentations to further understand the clinical correlates within peripheral and spinal cord contexts.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Explore the various clinical correlates from the periphery to the spinal cord in this quiz designed for Neuroscience PHT 5200. Understand the major sites where problems occur, including muscular conditions, neuromuscular junctions, and spinal cord issues. Test your knowledge on definitions and key concepts related to motor units and clinical pathologies.