Podcast
Questions and Answers
What is the primary factor that influences the Glomerular Filtration Rate (GFR)?
What is the primary factor that influences the Glomerular Filtration Rate (GFR)?
Which substance is NOT typically found in glomerular filtrate?
Which substance is NOT typically found in glomerular filtrate?
In which part of the nephron does active transport of sodium occur?
In which part of the nephron does active transport of sodium occur?
Which hormone influences the reabsorption of potassium in the nephron?
Which hormone influences the reabsorption of potassium in the nephron?
Signup and view all the answers
What process primarily influences the movement of water during reabsorption?
What process primarily influences the movement of water during reabsorption?
Signup and view all the answers
What encourages chloride ions to move during reabsorption?
What encourages chloride ions to move during reabsorption?
Signup and view all the answers
Which of the following substances is not actively transported during reabsorption?
Which of the following substances is not actively transported during reabsorption?
Signup and view all the answers
Which factor enhances calcium reabsorption in the nephron?
Which factor enhances calcium reabsorption in the nephron?
Signup and view all the answers
What percentage of tubular reabsorption occurs in the proximal convoluted tubule (PCT)?
What percentage of tubular reabsorption occurs in the proximal convoluted tubule (PCT)?
Signup and view all the answers
Which substance is primarily reabsorbed at the distal convoluted tubule (DCT)?
Which substance is primarily reabsorbed at the distal convoluted tubule (DCT)?
Signup and view all the answers
What role does antidiuretic hormone (ADH) play in urine volume regulation?
What role does antidiuretic hormone (ADH) play in urine volume regulation?
Signup and view all the answers
What is the primary site of tubular secretion?
What is the primary site of tubular secretion?
Signup and view all the answers
What triggers the release of renin from juxtaglomerular cells?
What triggers the release of renin from juxtaglomerular cells?
Signup and view all the answers
What physiological effect does angiotensin II have?
What physiological effect does angiotensin II have?
Signup and view all the answers
Which hormone regulates the sodium gradient in the nephron?
Which hormone regulates the sodium gradient in the nephron?
Signup and view all the answers
What substances are primarily secreted at the distal convoluted tubule?
What substances are primarily secreted at the distal convoluted tubule?
Signup and view all the answers
What is the primary function of the nephron?
What is the primary function of the nephron?
Signup and view all the answers
Which component of the renal corpuscle is responsible for the actual filtration of blood?
Which component of the renal corpuscle is responsible for the actual filtration of blood?
Signup and view all the answers
What type of epithelial cells primarily line the proximal convoluted tubule?
What type of epithelial cells primarily line the proximal convoluted tubule?
Signup and view all the answers
What is the role of the distilled convoluted tubule in the nephron?
What is the role of the distilled convoluted tubule in the nephron?
Signup and view all the answers
Where does the loop of Henle descend from?
Where does the loop of Henle descend from?
Signup and view all the answers
Which of the following describes the peritubular capillaries?
Which of the following describes the peritubular capillaries?
Signup and view all the answers
What is unique about the blood in the efferent glomerular arterioles?
What is unique about the blood in the efferent glomerular arterioles?
Signup and view all the answers
Which action primarily occurs in the collecting ducts?
Which action primarily occurs in the collecting ducts?
Signup and view all the answers
What percentage of cardiac output is delivered to the kidneys?
What percentage of cardiac output is delivered to the kidneys?
Signup and view all the answers
What occurs during the filtration process in the renal corpuscle?
What occurs during the filtration process in the renal corpuscle?
Signup and view all the answers
The visceral layer of Bowman's capsule is primarily composed of which cell type?
The visceral layer of Bowman's capsule is primarily composed of which cell type?
Signup and view all the answers
How are the actions of the sympathetic nervous system described in relation to the kidneys?
How are the actions of the sympathetic nervous system described in relation to the kidneys?
Signup and view all the answers
What can occur during tubular secretion?
What can occur during tubular secretion?
Signup and view all the answers
What is the final product of the nephron's function?
What is the final product of the nephron's function?
Signup and view all the answers
Which of the following is the first step in performing a urinalysis?
Which of the following is the first step in performing a urinalysis?
Signup and view all the answers
What is the primary nitrogenous waste material eliminated from the body?
What is the primary nitrogenous waste material eliminated from the body?
Signup and view all the answers
Which structure collects and stores urine in the urinary system?
Which structure collects and stores urine in the urinary system?
Signup and view all the answers
Which of the following is a function of antidiuretic hormone?
Which of the following is a function of antidiuretic hormone?
Signup and view all the answers
What is the main anatomical difference between the hilus and the renal pelvis of the kidney?
What is the main anatomical difference between the hilus and the renal pelvis of the kidney?
Signup and view all the answers
Which part of the nephron is responsible for the majority of reabsorption of essential substances?
Which part of the nephron is responsible for the majority of reabsorption of essential substances?
Signup and view all the answers
What differentiates glomerular filtrate from tubular filtrate?
What differentiates glomerular filtrate from tubular filtrate?
Signup and view all the answers
What is the term for organs located outside the abdominal cavity?
What is the term for organs located outside the abdominal cavity?
Signup and view all the answers
What is the effect of antidiuretic hormone (ADH) on urine volume?
What is the effect of antidiuretic hormone (ADH) on urine volume?
Signup and view all the answers
What process occurs when blood glucose levels exceed the renal threshold?
What process occurs when blood glucose levels exceed the renal threshold?
Signup and view all the answers
How do the kidneys respond to a decrease in blood pressure?
How do the kidneys respond to a decrease in blood pressure?
Signup and view all the answers
What characterizes prerenal uremia?
What characterizes prerenal uremia?
Signup and view all the answers
How does the structure of the ureters aid in preventing urine backflow?
How does the structure of the ureters aid in preventing urine backflow?
Signup and view all the answers
What role does the muscular sphincter play in the urinary bladder?
What role does the muscular sphincter play in the urinary bladder?
Signup and view all the answers
What is the consequence of an early indicator of kidney disease, such as proteinuria?
What is the consequence of an early indicator of kidney disease, such as proteinuria?
Signup and view all the answers
What is a common resulting condition in animals predisposed to urolith production?
What is a common resulting condition in animals predisposed to urolith production?
Signup and view all the answers
What happens when urine accumulation reaches a specific trigger point in the bladder?
What happens when urine accumulation reaches a specific trigger point in the bladder?
Signup and view all the answers
What are the implications of a deficiency in ADH regarding urine output?
What are the implications of a deficiency in ADH regarding urine output?
Signup and view all the answers
What primarily leads to proteinuria in renal failure?
What primarily leads to proteinuria in renal failure?
Signup and view all the answers
What is the primary difference between tubular reabsorption and tubular secretion?
What is the primary difference between tubular reabsorption and tubular secretion?
Signup and view all the answers
What is the typical characteristic of urine produced by individuals with diabetes insipidus?
What is the typical characteristic of urine produced by individuals with diabetes insipidus?
Signup and view all the answers
What factor determines when clinical signs of renal failure become apparent?
What factor determines when clinical signs of renal failure become apparent?
Signup and view all the answers
Study Notes
Microscopic Anatomy
- The basic functional unit of the kidney is the nephron, which is involved in filtration, reabsorption, and secretion.
- The number of nephrons per kidney varies by species and animal size
- Cats: 200,000/kidney
- Dogs: 700,000/kidney
- Sheep, pigs, humans: 1,000,000/kidney
- Cows: 4,000,000/kidney
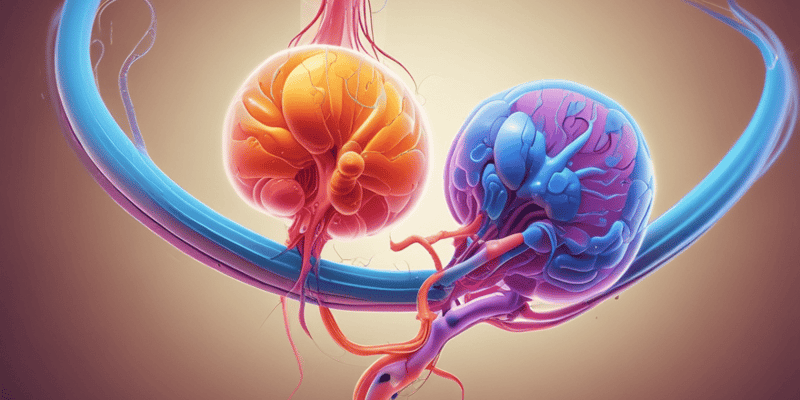
Nephron Components
-
Renal corpuscle:
- Located in the cortex
- Composed of the glomerulus (tuft of capillaries) and Bowman's capsule (double-walled capsule surrounding the glomerulus)
- The visceral layer of Bowman's capsule is made up of podocytes, which have spaces between them for filtration
- The capsular space is between the visceral and parietal layers and connects to the proximal convoluted tubule.
- It functions to filter blood and create urine.
-
Proximal convoluted tubule (PCT):
- Continuation of the capsular space
- Longest part of the tubular system
- Composed of cuboidal epithelial cells with microvilli, which aid in absorption.
-
Loop of Henle:
- Extends from the PCT, descending from the cortex to the medulla and then back to the cortex
- Descending limb: cuboidal epithelium with microvilli
- U-turn: simple squamous epithelium, no brush border
- Ascending limb: cuboidal epithelium, no microvilli
-
Distal convoluted tubule (DCT) and collecting ducts:
- The DCT continues from the ascending loop of Henle and empties into collecting ducts.
- Collecting ducts transport tubular filtrate through the medulla to the calyces, renal pelvis, and ultimately to the ureter.
- Important functions of the collecting ducts include:
- Urine volume determination (ADH action)
- Potassium regulation
- Acid-base balance
Renal Nerve Supply
- The sympathetic portion of the autonomic nervous system governs renal vasoconstriction.
- Vasoconstriction increases renal blood pressure and filtration rate
Renal Blood Supply
- The kidneys receive 25% of cardiac output
- Blood flow: renal artery -> arteries -> arterioles -> afferent glomerular arterioles -> glomerular capillaries -> efferent glomerular arterioles -> peritubular capillaries -> veins -> renal vein
- Afferent glomerular arterioles carry blood to the glomerular capillaries which filter plasma (glomerular filtrate) into Bowman's capsule.
- Efferent glomerular arterioles carry blood away from the glomerulus (still oxygenated).
- Peritubular capillaries branch from the efferent glomerular arterioles:
- Oxygen transfer occurs here
- Substances are reabsorbed back into the blood and secreted into the tubules.
Mechanisms of Renal Action
-
Filtration: Occurs in the renal corpuscle
- The glomerular capillaries have high blood pressure due to the size difference between the afferent and efferent arterioles (afferent diameter > efferent).
- Glomerular fenestrations aid in filtration.
- Glomerular filtrate is similar to plasma but lacks proteins.
-
Glomerular Filtration Rate (GFR):
- Represents the rate at which plasma is filtered through the glomerulus.
- Depends on the rate of blood flow through the kidney.
- Measured in mL/min.
- Approximately 25% of plasma is filtered each minute.
-
Reabsorption:
- Substances move from the renal tubules to the peritubular capillaries through osmosis, diffusion, and active transport.
- Path of reabsorption: tubular lumen -> tubular epithelium -> interstitial fluid -> endothelium -> peritubular capillaries.
-
Secretion:
- Eliminates substances not adequately filtered by the GFR.
- Path of secretion: peritubular capillaries -> interstitial fluid -> tubular epithelial cells -> tubular filtrate.
- DCT is the main site for tubular secretion.
Key Substances Reabsorbed and Secreted:
-
Reabsorbed Substances:
- Sodium (Na)
- Potassium (K)
- Calcium (Ca)
- Magnesium (Mg)
- Glucose
- Amino acids
- Chloride (Cl)
- Bicarbonate (HCO3)
- Water
-
Secreted Substances:
- Hydrogen (H)
- Potassium (K)
- Ammonia
- Antibiotics (penicillin, some sulfas)
Urine Volume Regulation
-
Antidiuretic hormone (ADH):
- Released from the posterior pituitary gland
- Acts on the DCT and collecting ducts to promote water reabsorption.
- Without ADH, water reabsorption is reduced, resulting in increased urine production.
-
Aldosterone:
- Released from the adrenal cortex
- Acts on the DCT and collecting ducts, regulating sodium gradients to control water reabsorption.
- Increased aldosterone promotes sodium retention and water reabsorption
Regulation of Blood Pressure
-
Renin-angiotensin-aldosterone system (RAAS):
- Activated in response to low blood pressure.
- Juxtaglomerular cells (located in the afferent glomerular arterioles) monitor blood pressure.
- Macula densa (within the ascending loop of Henle) monitors NaCl concentration of the tubular filtrate.
- If low blood pressure or low sodium is detected, the juxtaglomerular cells release renin.
-
Renin:
- Splits angiotensin I from angiotensinogen.
-
Angiotensin I:
- Converted to angiotensin II by angiotensin-converting enzyme (ACE)
-
Angiotensin II:
- Causes arterial constriction, increasing blood pressure.
- Stimulates aldosterone release from the adrenal glands.
- Aldosterone increases sodium and water reabsorption, further increasing blood pressure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the intricate structure of the nephron, the fundamental unit of kidney function. This quiz covers key components such as the renal corpuscle, glomerulus, and proximal convoluted tubule, along with variations in nephron count across species. Test your knowledge on filtration and urine formation processes.