Podcast
Questions and Answers
What is the primary function of the calf muscles during mid-stance and terminal stance?
What is the primary function of the calf muscles during mid-stance and terminal stance?
- To produce a plantar flexion moment
- To produce a dorsiflexion moment
- To oppose dorsiflexion moment and control tibial advance (correct)
- To stabilize the ankle joint
What is the result of uncontrolled tibial advancement during the weight-bearing period?
What is the result of uncontrolled tibial advancement during the weight-bearing period?
- Ankle sprain
- Tibial instability (correct)
- Hip abduction
- Knee flexion
How do the calf muscles contract during the pre-swing phase?
How do the calf muscles contract during the pre-swing phase?
- Eccentrically
- Concentrically (correct)
- Isotonically
- Isometrically
What is the effect of weakness of the calf muscles on the knee joint?
What is the effect of weakness of the calf muscles on the knee joint?
What is the characteristic of the gait pattern in a person with weakness of the dorsi flexors?
What is the characteristic of the gait pattern in a person with weakness of the dorsi flexors?
What is the long-term effect of compensating for weakness of the dorsi flexors?
What is the long-term effect of compensating for weakness of the dorsi flexors?
What is the role of the unaffected limb in contralateral vaulting?
What is the role of the unaffected limb in contralateral vaulting?
What is the effect of weakness of the calf muscles on the ankle joint?
What is the effect of weakness of the calf muscles on the ankle joint?
What is the result of delayed heel rise during the stance phase?
What is the result of delayed heel rise during the stance phase?
What is the role of the quadriceps in compensating for weakness of the calf muscles?
What is the role of the quadriceps in compensating for weakness of the calf muscles?
Study Notes
Influences on Gait
- Pain, posture, flexibility, endurance, base of support, inter-limb coordination, leg length, gender, pregnancy, obesity, age, and displacement of the center of gravity (COG) are factors that influence gait.
Causes of Pathological Gait
- Deformity (congenital or acquired), impaired motor control or spasticity, sensory loss, pain, muscle weakness, and other factors can cause pathological gait.
Deformity of Hip
- Coxa valga: increased neck shaft angle (>135°)
- Coxa vara: decreased neck shaft angle (<120°)
Deformity of Knee
- Knock knee (genu valgus)
- Bow leg (genu varum)
- Back knee (genu recurvatum)
Deformity of Ankle
- Equinus deformity: plantar flexion deformity
- Calcaneus deformity: dorsiflexion deformity
Deformity of Foot
- Club foot (talipes equino varus) or supinated foot: plantar flexion, inversion, and adduction
- Talipes calcino valgus or pronated foot: dorsiflexion, eversion, and abduction
Deformity
- Plantar flexion contracture: blocks progression of the limb over the supporting foot and inhibits floor clearance during swing
- Knee flexion contracture: blocks progression during stance and increases the activity of quadriceps
- Knee extension contracture: increases the energy cost of walking by requiring additional body maneuvers for floor clearance during swing
- Hip flexion contracture: impairs hip stability during stance and introduces strain on the back muscles and hip extensors
Impaired Motor Control (Spasticity)
- Hip flexor spasticity: restricts progression in mid and terminal stance
- Sustained quadriceps action: inhibits pre-swing preparation for limb advancement
- Plantar flexors spasticity: leads to persistent ankle plantar flexion and inability to rise on the metatarsal heads
- Hamstring spasticity: leads to persistent knee flexion and limits thigh advancement in stance and terminal swing
Sensory Loss
- Prevents the patient from knowing the position of the hip, knee, ankle, or foot
- Moderate sensory loss causes slow walking
- Greater sensory loss may obstruct walking as it causes the patient to be unable to trust the motions that occur
Pain
- Major causes of musculoskeletal pain: excessive tissue tension, joint distension related to trauma or arthritis
- Pain can cause antalgic gait (limping gait)
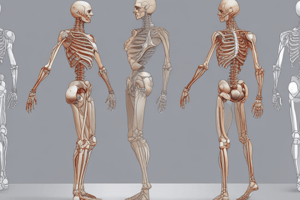
Muscle Weakness
- When the patient's muscle strength is insufficient to meet the demands of walking
- Can be caused by disuse muscular atrophy or neurological impairment
- Patients with muscle weakness can modify the timing of muscle action to avoid threatening postures, induce protective alignment during stance, and walk at a slower speed
Weakness of Hip Extensors (Gluteus Maximus)
- Normal function: counteracts flexion moment during single-limb support
- Effect of weakness on gait: inability to counteract flexion moment, excessive hip flexion, and tendency for anterior pelvic tilt
- Possible compensation: leaning the trunk backward to shift the ground reaction force vector (GRFV) behind the axis of the hip joint
- Long-term effects of compensation: excessive lumbar lordosis, shifting the lumbosacral joint anterior to the hip joint, and mechanical lower back pain
Weakness of Hip Abductors (Gluteus Medius)
- Normal function: counteracts adduction moment during single-limb support
- Effect of weakness on gait: inability to counteract adduction moment, resulting in loss of balance and a positive Trendelenberg sign
- Possible compensation: leaning the trunk laterally toward the weak limb, resulting in a gluteus medius gait or waddling gait
- Long-term effects of compensation: lateral spinal curve (functional scoliosis)
Weakness of Knee Extensors (Quadriceps)
- Normal function: counteracts flexion moment during loading response
- Effect of weakness on gait: inability to counteract flexion moment, resulting in excessive knee flexion during loading response, decreased shock absorption, and knee joint instability
- Possible compensation: leaning the trunk forward to shift the GRFV anterior to the knee joint, creating an extension moment, and placing the knee in hyperextension
Weakness of Dorsi Flexors (Anterior Tibial Group)
- Normal function: counteracts dorsiflexion moment during mid-stance and terminal stance
- Effect of weakness on gait: inability to counteract dorsiflexion moment, resulting in excessive ankle dorsiflexion and uncontrolled tibial advancement
- Possible compensation: increased demand on quadriceps to counteract tibial instability, delayed heel rise, and loss of knee extension during terminal stance
Weakness of Calf Muscles
- Normal function: counteracts dorsiflexion moment during mid-stance, terminal stance, and pre-swing
- Effect of weakness on gait: inability to counteract dorsiflexion moment, resulting in excessive ankle dorsiflexion and uncontrolled tibial advancement
- Possible compensation: increased demand on quadriceps to counteract tibial instability, delayed heel rise, and loss of knee extension during terminal stance
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the factors that affect gait, including physical characteristics and conditions, as well as the causes of abnormal gait patterns.