Podcast
Questions and Answers
What is the primary active process involved in renal cellular transport?
What is the primary active process involved in renal cellular transport?
In the proximal tubule, sodium reabsorption primarily occurs through which mechanism?
In the proximal tubule, sodium reabsorption primarily occurs through which mechanism?
What additional process is required for the effective reabsorption of bicarbonate (HCO3-) in the proximal tubule?
What additional process is required for the effective reabsorption of bicarbonate (HCO3-) in the proximal tubule?
What is the outcome of the sodium-potassium exchange mediated by the sodium-potassium ATPase?
What is the outcome of the sodium-potassium exchange mediated by the sodium-potassium ATPase?
Signup and view all the answers
What mechanism is primarily responsible for sodium reabsorption across the proximal tubule epithelial cells?
What mechanism is primarily responsible for sodium reabsorption across the proximal tubule epithelial cells?
Signup and view all the answers
Which of the following factors is not involved in the regulation of tubular transport processes?
Which of the following factors is not involved in the regulation of tubular transport processes?
Signup and view all the answers
What type of epithelium lines the female urethra?
What type of epithelium lines the female urethra?
Signup and view all the answers
What are umbrella cells and where are they found?
What are umbrella cells and where are they found?
Signup and view all the answers
Which key renal function is primarily associated with the reabsorption of sodium?
Which key renal function is primarily associated with the reabsorption of sodium?
Signup and view all the answers
What occurs when the sodium-potassium pump operates in renal epithelial cells?
What occurs when the sodium-potassium pump operates in renal epithelial cells?
Signup and view all the answers
What unique feature allows the transitional epithelium to accommodate a full bladder?
What unique feature allows the transitional epithelium to accommodate a full bladder?
Signup and view all the answers
What structure is formed at the urethra in the urinary bladder?
What structure is formed at the urethra in the urinary bladder?
Signup and view all the answers
Which of the following describes the arrangement of muscle layers in the urinary bladder?
Which of the following describes the arrangement of muscle layers in the urinary bladder?
Signup and view all the answers
In terms of histology, how does the male urethra differ from the female urethra?
In terms of histology, how does the male urethra differ from the female urethra?
Signup and view all the answers
What role do sensory fibers play in the micturition reflex?
What role do sensory fibers play in the micturition reflex?
Signup and view all the answers
How long is the male urethra on average?
How long is the male urethra on average?
Signup and view all the answers
What is the primary mechanism by which water moves from the interstitial space into blood vessels?
What is the primary mechanism by which water moves from the interstitial space into blood vessels?
Signup and view all the answers
What is the net force moving filtrate into capillaries?
What is the net force moving filtrate into capillaries?
Signup and view all the answers
In which part of the loop of Henle does the reabsorption of sodium mainly occur?
In which part of the loop of Henle does the reabsorption of sodium mainly occur?
Signup and view all the answers
Which mechanism is primarily responsible for sodium reabsorption in the thick ascending limb?
Which mechanism is primarily responsible for sodium reabsorption in the thick ascending limb?
Signup and view all the answers
What occurs in the thin ascending limb of the loop of Henle?
What occurs in the thin ascending limb of the loop of Henle?
Signup and view all the answers
Which of the following ions is primarily reabsorbed across the paracellular pathway in the thick ascending limb due to a positive tubular fluid charge?
Which of the following ions is primarily reabsorbed across the paracellular pathway in the thick ascending limb due to a positive tubular fluid charge?
Signup and view all the answers
What role does Na,K-ATPase play in the thicken ascending limb of the loop of Henle?
What role does Na,K-ATPase play in the thicken ascending limb of the loop of Henle?
Signup and view all the answers
Why is the thick ascending limb of the loop of Henle impermeable to water?
Why is the thick ascending limb of the loop of Henle impermeable to water?
Signup and view all the answers
What percentage of the filtered NaCl is reabsorbed by the proximal tubule?
What percentage of the filtered NaCl is reabsorbed by the proximal tubule?
Signup and view all the answers
How does sodium primarily enter the renal tubule cells at the luminal membrane?
How does sodium primarily enter the renal tubule cells at the luminal membrane?
Signup and view all the answers
What effect does the high concentration of Cl- in tubular fluid have on Na+ movement?
What effect does the high concentration of Cl- in tubular fluid have on Na+ movement?
Signup and view all the answers
What is the primary driving force for water reabsorption in the proximal tubule?
What is the primary driving force for water reabsorption in the proximal tubule?
Signup and view all the answers
In what manner is water primarily reabsorbed in the proximal tubule?
In what manner is water primarily reabsorbed in the proximal tubule?
Signup and view all the answers
What occurs to the osmolality of the tubular fluid during the reabsorption of solutes?
What occurs to the osmolality of the tubular fluid during the reabsorption of solutes?
Signup and view all the answers
Which mechanism allows for NaCl reabsorption via a paracellular route?
Which mechanism allows for NaCl reabsorption via a paracellular route?
Signup and view all the answers
What type of transporter is involved in sodium leaving the cell at the basolateral membrane?
What type of transporter is involved in sodium leaving the cell at the basolateral membrane?
Signup and view all the answers
What stimulates aldosterone secretion?
What stimulates aldosterone secretion?
Signup and view all the answers
What is the primary mechanism for bicarbonate reabsorption in the proximal tubules?
What is the primary mechanism for bicarbonate reabsorption in the proximal tubules?
Signup and view all the answers
Where is most of the filtered bicarbonate reabsorbed?
Where is most of the filtered bicarbonate reabsorbed?
Signup and view all the answers
What is NOT a condition that inhibits aldosterone secretion?
What is NOT a condition that inhibits aldosterone secretion?
Signup and view all the answers
What process is primarily responsible for producing new bicarbonate in the body?
What process is primarily responsible for producing new bicarbonate in the body?
Signup and view all the answers
How is bicarbonate reabsorbed across the basolateral membrane of the proximal tubule?
How is bicarbonate reabsorbed across the basolateral membrane of the proximal tubule?
Signup and view all the answers
What percentage of filtered HCO3- is typically excreted?
What percentage of filtered HCO3- is typically excreted?
Signup and view all the answers
Where does the majority of H+ secreted in the collecting duct combine with urinary buffer?
Where does the majority of H+ secreted in the collecting duct combine with urinary buffer?
Signup and view all the answers
Study Notes
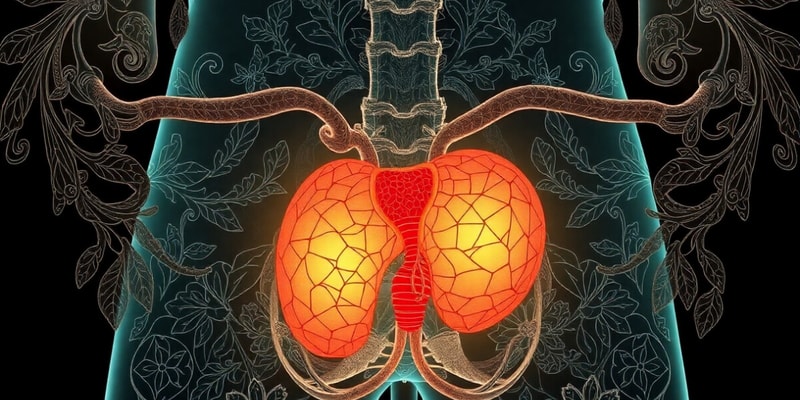
### Bladder
- Epithelium is stratified and variable in thickness
- 2-3 layers in minor calyces, 5-6 layers in bladder
- Cells can stretch and shift over each other, accommodating a full bladder
- Full bladder appears to have only 2-3 layers of flat cells
- Empty bladder:
- Cuboidal basal layer
- Polygonal middle layer
- Convex, often binucleate tall upper layer
- Surface has plaques: modified plasma membrane areas that unfold allowing stretching
- Umbrella cells of the surface layer can be binucleate and have a refractile border
Ureters
- Transitional epithelium with a lamina propria consisting of fibroblasts and connective tissue
- Two spirally arranged muscle layers
- Third layer towards the urinary bladder
- Adventitia and serosa
### Urinary Bladder
- Transitional epithelium with 3 spiraled muscle layers: longitudinal, circular, longitudinal
- Internal sphincter is formed at the urethra
- Sympathetic fibres in the adventitia
- Parasympathetic fibres in the adventitia and muscle
- These fibres form the efferent fibres of the micturation reflex
- Sensory fibres from the bladder muscle to the sacral portion of the spinal cord form the afferent fibres of the micturation reflex
### Female Urethra
- Stratified squamous epithelium
- Lamina propria: vascular and contains mucous secreting glands
- External sphincter of striated muscle from the mid portion of urethra, passes through the striated muscles of the pelvic floor
### Male Urethra
- 20-25 cm long
- Two functions: void urine and final conduit of male reproductive system
- Three segments:
- Prostatic: from the neck of the bladder through the prostate
- Receives the openings of the ejaculatory ducts
- Many periurethral glands open into it
- Very thin here
- Membranous: 1 cm long, runs through the pelvic floor
- External sphincter of striated muscle
- Penile
- Small mucous glands open into it
- Prostatic: from the neck of the bladder through the prostate
- Lined with:
- Transitional epithelium
- Stratified columnar epithelium
- Stratified cuboidal epithelium
- Stratified squamous epithelium progressively
### Renal Transport Processes
#### Main Renal Functions
- Sodium and water reabsorption
- Electrolyte balance
- Acid-base balance
#### Basic Elements of the Renal Transport Process
- Key element and primary active process is mediated by sodium/potassium ATPase situated at the basolateral membrane
- 3 Na+ exchanged for 2K+ within the cell, some K+ filters back into the interstitial space, resulting in a net negative charge (-70mv) inside the cell
- Sodium/potassium pump maintains decreased cellular sodium concentration, resulting in a favourable gradient for the movement of sodium from the tubular fluid into the cell
### Proximal Tubule
#### First Half
- Sodium reabsorption coupled with H+ (antiport mechanism) or organic solutes mainly glucose and amino acids (symport mechanism)
- Accompanying filtered anion HCO3- requires a different process involving carbonic anhydrase (CA) for effective reabsorption
- Coupled process for Na reabsorption is associated with specific transport proteins (facilitated transport) along concentration and electrochemical gradients (secondary active process)
- Transport proteins operate secondarily to Na/K- ATPase situated at the basolateral membrane of the cell, which is the primary source of energy for renal transport processes
#### Second Half
- Sodium enters the cell luminal membrane via a parallel operation involving a Na+-H+ antiporter and a Cl—Anion antiporter
- Secreted H+ and anion combine in the tubular fluid and re-enter the cell by diffusion, resulting in uptake of NaCl
- Sodium leaves the cell via Na/K- ATPase at the basolateral membrane, chloride leaves via a K/Cl- symporter
- NaCl is also reabsorbed via a paracellular route
- High concentration of Cl- in the tubular fluid in the second half results in a concentration gradient with Cl- in the interstitial space, facilitating movement of Cl- out of the tubular fluid
- Loss of Cl- makes the tubular fluid positively charged, facilitating movement of Na+ out of the tubular fluid
#### Overall
- 67% of filtered NaCl is reabsorbed by the proximal tubule
- Two-thirds reabsorbed via a transcellular route and one-third via the paracellular route
#### Water Reabsorption
- 67% of the water in the filtrate is reabsorbed in the proximal tubule
- Driving force is the transtubular osmotic gradient established by solute reabsorption (NaCl, glucose, HCO 3-)
- Water moves along the osmotic gradient into the interstitial space mostly via the paracellular route
- Reabsorption of water is isosmotic, so the osmolality of the tubular fluid remains the same as plasma in the proximal tubule
- Once water has accumulated in the interstitial space by osmosis, it moves by filtration into the blood vessels, dependant on filtration forces
### Loop of Henle
#### Descending Limb
- Reabsorption of water but not sodium
- Increasing sodium concentration within the tubule
#### Ascending Limb
##### Thin Ascending Limb
- Sodium diffuses out along a concentration gradient, impermeable to water
- Decreasing osmolality of the tubular fluid
##### Thick Ascending Limb (TAL)
- Na/K- ATPase plays the same role in the reabsorption of sodium as it does in the proximal tubule
- Sodium reabsorption at the luminal membrane is mediated by the Na+- 2Cl- - K+ symporter, which is the carrier protein inhibited by loop diuretics
- Na+- H+ antiporter situated at the apical membrane facilitates the reabsorption of sodium and the secretion of H+ by a secondary active transport process
- Reabsorption of HCO3-
- Potassium and chloride leave the cell at the basolateral membrane by facilitated diffusion
- Tubular fluid in TAL is positively charged due to increased Cl- transport in the second half of the proximal tubule and also within TAL
- Positive charge in the tubular fluid causes the reabsorption of cations, mainly Na+, but also Ca++, K+ and Mg++ across the paracellular pathway
- TAL is also not permeable to water
### Distal Tubule
- Responsible for fine-tuning the reabsorption of sodium, potassium, and calcium
- Reabsorption of water is regulated by antidiuretic hormone (ADH)
- Na+ reabsorption is stimulated by aldosterone
- Reabsorption of water is isosmotic
### Collecting Duct
- Reabsorption of sodium and water under the influence of aldosterone and ADH
- Reabsorption of potassium is regulated by aldosterone
- Reabsorption of water is regulated by ADH
#### Aldosterone Effects
- Aldosterone secretion is stimulated by angiotensin II and hyperkalemia
- Inhibited by hypervolemia, hypokalemia and natriuretic peptide
- Stimulates sodium reabsorption, increasing water reabsorption, plays a critical role in maintaining fluid balance
- Reabsorption of water is isosmotic
### Reabsorption of Bicarbonate
- Reabsorption of HCO3- requires secretion of H+
- H+ secretion is dependent on the actions of a Na+- H+ antiporter and a H+- ATPase at the apical membrane of the proximal tubular cells and on the Na+- H+ antiporter at the apical membrane of TAL tubular cells
- H+, K+- antiporter and H+- ATPase at the apical membrane of the Intercalated cell found in the late distal tubules and the collecting ducts
- CO2 is produced in the tubular cell as part of normal metabolic processes or diffuses into the tubular cell from the tubular fluid or the interstitium
- CO2 combines with H2O catalysed by carbonic anhydrase (CA) to produce carbonic acid
- Carbonic acid dissociates into H+ and HCO3-
- Bicarbonate exits the cell across the basolateral membrane and returns to the peritubular blood
- Exit is mediated by a Na+- 3HCO3- symporter and a Cl- - HCO3- antiporter
- Both mechanisms are active in the proximal tubules (85% of filtered HCO 3-) and TAL (10% of filtered HCO3-)
- Cl- - HCO3- antiporter is active at the basolateral membrane of the Intercalated cell located in the late distal tubules and collecting ducts (4.9% of filtered HCO 3-)
- About 0.1% of filtered HCO3- is excreted
### Urinary Buffering
- HCO3- reabsorption does not replenish HCO3- lost during buffering processes in body fluids accompanying metabolism
- New HCO3- needs to be produced to maintain acid-base balance
- Tubular fluid contains little HCO3- because most of it is reabsorbed in upstream segments of the nephron
- H+ secreted into the tubular fluid of the collecting ducts combines with urinary buffer as a consequence
- HCO3- produced from endogenous CO2 involving the activity of carbonic anhydrase does not form part of the filtered HCO 3- and represents newly produced HCO3-
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the structure and function of the urinary bladder and ureters in this detailed quiz. Learn about the transitional epithelium, muscle layers, and unique characteristics that allow these organs to accommodate varying volumes. Test your knowledge on how these features contribute to the urinary system as a whole.