Podcast
Questions and Answers
What is a characteristic feature of COPD?
What is a characteristic feature of COPD?
Which of the following is NOT considered a common obstructive lung disorder?
Which of the following is NOT considered a common obstructive lung disorder?
What is one of the main risk factors for developing COPD?
What is one of the main risk factors for developing COPD?
Which symptom is most commonly associated with obstructive lung diseases?
Which symptom is most commonly associated with obstructive lung diseases?
Signup and view all the answers
What type of treatment is commonly used for managing COPD symptoms?
What type of treatment is commonly used for managing COPD symptoms?
Signup and view all the answers
What is a direct consequence of chronic inflammation caused by inhalation of cigarette smoke or other noxious particles?
What is a direct consequence of chronic inflammation caused by inhalation of cigarette smoke or other noxious particles?
Signup and view all the answers
What characterizes chronic bronchitis as defined in the content?
What characterizes chronic bronchitis as defined in the content?
Signup and view all the answers
Which of the following is NOT a consequence of chronic inflammatory responses in chronic bronchitis?
Which of the following is NOT a consequence of chronic inflammatory responses in chronic bronchitis?
Signup and view all the answers
What results from repeated injury and repair in the context of chronic pulmonary conditions?
What results from repeated injury and repair in the context of chronic pulmonary conditions?
Signup and view all the answers
What treatment modalities are commonly used for chronic bronchitis?
What treatment modalities are commonly used for chronic bronchitis?
Signup and view all the answers
What is a common characteristic of asthma onset?
What is a common characteristic of asthma onset?
Signup and view all the answers
Which inflammatory cells are primarily involved in asthma?
Which inflammatory cells are primarily involved in asthma?
Signup and view all the answers
What is the primary cause of COPD according to the information provided?
What is the primary cause of COPD according to the information provided?
Signup and view all the answers
How does airflow limitation differ between asthma and COPD?
How does airflow limitation differ between asthma and COPD?
Signup and view all the answers
Which type of T-regulatory cells are decreased in asthma, contributing to airway remodeling?
Which type of T-regulatory cells are decreased in asthma, contributing to airway remodeling?
Signup and view all the answers
What is a primary characteristic of emphysema?
What is a primary characteristic of emphysema?
Signup and view all the answers
Which treatment is NOT typically associated with managing asthma?
Which treatment is NOT typically associated with managing asthma?
Signup and view all the answers
What happens during the late asthmatic response?
What happens during the late asthmatic response?
Signup and view all the answers
What best describes the obstruction in emphysema?
What best describes the obstruction in emphysema?
Signup and view all the answers
Which symptom is typically associated with asthma?
Which symptom is typically associated with asthma?
Signup and view all the answers
What type of secretions are typically produced during an asthma attack?
What type of secretions are typically produced during an asthma attack?
Signup and view all the answers
In emphysema, what is a complication that may occur due to alveolar destruction?
In emphysema, what is a complication that may occur due to alveolar destruction?
Signup and view all the answers
What is the initial response that occurs in asthma during an attack?
What is the initial response that occurs in asthma during an attack?
Signup and view all the answers
What is pneumothorax primarily characterized by?
What is pneumothorax primarily characterized by?
Signup and view all the answers
Which factor is most commonly associated with spontaneous pneumothorax in healthy individuals?
Which factor is most commonly associated with spontaneous pneumothorax in healthy individuals?
Signup and view all the answers
What type of pneumothorax involves a one-way valve that accumulates pressure?
What type of pneumothorax involves a one-way valve that accumulates pressure?
Signup and view all the answers
What are the primary components of Virchow triad associated with pulmonary embolism?
What are the primary components of Virchow triad associated with pulmonary embolism?
Signup and view all the answers
What can cause secondary pneumothorax?
What can cause secondary pneumothorax?
Signup and view all the answers
Which condition describes the presence of pus within the pleural effusion?
Which condition describes the presence of pus within the pleural effusion?
Signup and view all the answers
What is a pulmonary embolus primarily caused by?
What is a pulmonary embolus primarily caused by?
Signup and view all the answers
What is pulmonary edema commonly characterized by?
What is pulmonary edema commonly characterized by?
Signup and view all the answers
Study Notes
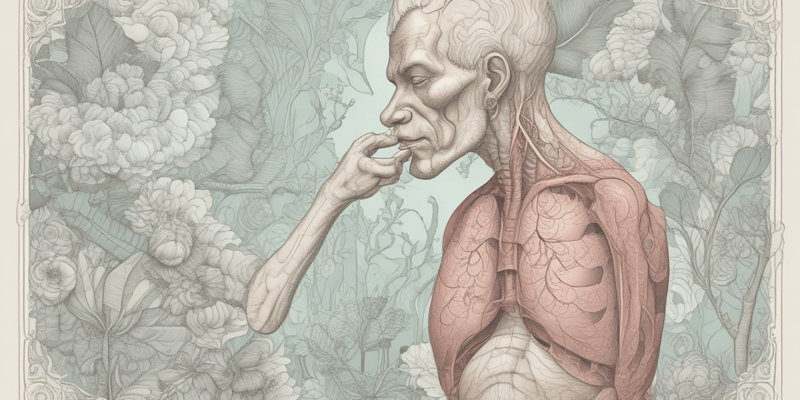
Obstructive Lung Diseases
- Airway obstruction is worse with expiration.
- Common signs and symptoms include dyspnea and wheezing.
Chronic Obstructive Pulmonary Disease (COPD)
- Characterized by persistent airflow limitation.
- It is progressive and the most common chronic lung disease globally.
- COPD is preventable and treatable.
- Enhanced chronic inflammatory response is a hallmark of the disease.
- Exacerbations and comorbidities contribute to the severity of COPD.
- Risk factors include tobacco smoke, occupational dusts and chemicals, air pollution, and factors affecting lung growth during gestation and childhood.
- Treatment includes bronchodilators, mucolytics, antioxidants, and anti-inflammatory medications.
Pathogenesis of COPD
- Inhalation of cigarette smoke or other noxious particles causes chronic inflammation.
- Chronic inflammatory response can lead to destruction of lung tissue (emphysema), disruption of airways, and impairment of lung defense mechanisms.
- Resulting structural changes contribute to airflow limitation that is not fully reversible.
Chronic Bronchitis
- Defined by hypersecretion of mucus and chronic productive cough lasting for at least 3 months a year, for 2 consecutive years.
- Inspired irritants increase mucus production and the size and number of mucous glands.
- Causes airway narrowing due to smooth muscle hypertrophy, fibrosis.
- Chronic inflammation contributes to bronchial edema.
- Mucus is thicker than normal.
- Bronchodilators, expectorants, and chest physiotherapy are used for treatment.
Emphysema
- Characterized by permanent enlargement of gas-exchange airways along with destruction of alveolar walls without obvious fibrosis.
- Obstruction occurs due to changes in lung tissues rather than mucus production and inflammation.
- Inherited deficit of α1-antitrypsin is a rare cause (1%).
- Destruction of alveoli leads to the production of large air sacs (bullae) and air spaces (blebs) that are not effective in gas exchange.
- Loss of elastic recoil makes expiration difficult and leads to air trapping.
- Treatment includes smoking cessation, inhaled anticholinergics, bronchodilators, steroids, phosphodiesterase inhibitors, and lung volume reduction surgery.
Asthma
- A chronic inflammatory disorder of the airways.
- Inflammation results in airway hyperresponsiveness.
- Can lead to airway obstruction and status asthmaticus.
- Symptoms include expiratory wheezing, dyspnea, and tachypnea.
- Peak flow meters, corticosteroids, beta-agonists, and anti-inflammatories are used for treatment.
Bronchoconstriction during Asthma Attacks
- Sudden contraction of smooth muscle causes acute dyspnea.
- Thick, viscous secretions accumulate.
- Edema is caused by engorgement of pulmonary blood vessels.
Pathophysiology of Asthma: Early vs Late Response
- Early Asthmatic Response: Vasodilation, increased capillary permeability, mucosal edema, bronchial smooth muscle contraction (bronchospasm), and tenacious mucous secretion.
- Late Asthmatic Response: Begins 4-8 hours after the early response. Chemotactic recruitment of lymphocytes, eosinophils, basophils, neutrophils, and lymphocytes occurs. Airway scarring, increased bronchial hyperresponsiveness, impaired mucociliary function, accumulation of mucous and cellular debris forming plugs in the airways, decreased Treg cells, and airway remodeling if left untreated.
Asthma vs COPD
- Asthma: Onset early in life (often childhood), symptoms vary from day to day, worse at night and early AM, caused by sensitizing agents and triggers, inflammatory cells include eosinophils and CD4+ helper T-cells, airflow limitation usually reversible.
- COPD: Onset later in life, progressive symptoms, usually associated with lengthy smoking history or α1-antitrypsin deficiency in non-smokers, inflammatory cells include neutrophils, macrophages, and CD8+ cytotoxic T-cells, airflow limitation not fully reversible.
Pneumothorax
-
Presence of air or gas in the pleural space.
-
Caused by rupture of visceral pleura or parietal pleura and chest wall.
-
Air separates pleura, leading to loss of negative pressure.
-
Lung recoils toward the hilum.
-
Spontaneous pneumothorax: Occurs in healthy men aged 20-40, often due to rupture of bullae and blebs at the apex of the lung. 80% of cases involve emphysemic changes, while 10% have no previous history.
-
Secondary pneumothorax: Caused by trauma, rib fractures, bullet wounds, stabbing, or mechanical ventilation.
-
Open pneumothorax: Air enters the pleural space freely.
-
Tension pneumothorax: One-way valve effect leads to accumulation of pressure, pushing the lung to the other side, displacing the heart and vessels, and potentially causing life-threatening conditions.
Pleural Abnormalities
-
Pleural effusion: Fluid accumulation in the pleural space.
- Transudative effusion: Caused by increased hydrostatic pressure or decreased oncotic pressure.
- Exudative effusion: Caused by inflammation or infection.
-
Hemothorax: Blood in the pleural space.
-
Empyema: Infected pleural effusion containing pus.
-
Chylothorax: Lymph fluid in the pleural space.
Pulmonary Edema
- Excess water in the lungs.
Pulmonary Embolus
- Occlusion of a portion of the pulmonary vascular bed by a thrombus, embolus, tissue fragment, lipids, or an air bubble.
- Pulmonary emboli commonly arise from the deep veins in the lower leg.
- Virchow's triad: Venous stasis, hypercoagulability, and endothelial damage to the vessels contribute to the formation of pulmonary emboli.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the key aspects of Chronic Obstructive Pulmonary Disease (COPD), including its pathogenesis, symptoms, and treatment options. Understand the risk factors and the significance of airway obstruction in lung diseases. Test your knowledge about COPD and its impact on health.