Podcast
Questions and Answers
What is the primary function of the lower oesophageal sphincter (LES) in the oesophagus?
What is the primary function of the lower oesophageal sphincter (LES) in the oesophagus?
What is the typical length of the oesophagus in humans?
What is the typical length of the oesophagus in humans?
What is the primary cause of obstruction in the oesophagus?
What is the primary cause of obstruction in the oesophagus?
What is the term for the inability to swallow due to obstruction in the oesophagus?
What is the term for the inability to swallow due to obstruction in the oesophagus?
Signup and view all the answers
What is the name of the condition characterized by the reflux of HCl into the esophagus?
What is the name of the condition characterized by the reflux of HCl into the esophagus?
Signup and view all the answers
What is the term for the inflammation of the oesophageal mucosa?
What is the term for the inflammation of the oesophageal mucosa?
Signup and view all the answers
What is the primary mechanism of damage caused by H. pylori infection in gastritis?
What is the primary mechanism of damage caused by H. pylori infection in gastritis?
Signup and view all the answers
What is the primary diagnostic test for chronic infection with H. pylori?
What is the primary diagnostic test for chronic infection with H. pylori?
Signup and view all the answers
What is the consequence of immunologic loss of parietal cell function in gastritis?
What is the consequence of immunologic loss of parietal cell function in gastritis?
Signup and view all the answers
What is the primary mechanism of damage caused by NSAIDs in gastritis?
What is the primary mechanism of damage caused by NSAIDs in gastritis?
Signup and view all the answers
What is the characteristic of chronic gastritis?
What is the characteristic of chronic gastritis?
Signup and view all the answers
What is the complication of gastritis that can lead to acute GI bleeding?
What is the complication of gastritis that can lead to acute GI bleeding?
Signup and view all the answers
What prevents backflow of bacteria from the colon into the small intestine?
What prevents backflow of bacteria from the colon into the small intestine?
Signup and view all the answers
What is the primary cause of fat malabsorption in Abetalipoproteinaemia?
What is the primary cause of fat malabsorption in Abetalipoproteinaemia?
Signup and view all the answers
Which of the following conditions is characterized by the malabsorption of bile acids?
Which of the following conditions is characterized by the malabsorption of bile acids?
Signup and view all the answers
What is the result of bacterial overgrowth in the small intestine?
What is the result of bacterial overgrowth in the small intestine?
Signup and view all the answers
What is the term for the inability to digest lactose due to a deficiency of a specific enzyme?
What is the term for the inability to digest lactose due to a deficiency of a specific enzyme?
Signup and view all the answers
What is the sensitivity of anti-gliadin antibodies IgA and tTG by blood test for diagnosing Coeliac disease?
What is the sensitivity of anti-gliadin antibodies IgA and tTG by blood test for diagnosing Coeliac disease?
Signup and view all the answers
What is the characteristic appearance of skin manifestations of Coeliac disease in 15-25 % of patients?
What is the characteristic appearance of skin manifestations of Coeliac disease in 15-25 % of patients?
Signup and view all the answers
What is the effect of a gluten-free diet on mucosal histology in Coeliac disease?
What is the effect of a gluten-free diet on mucosal histology in Coeliac disease?
Signup and view all the answers
What is the most common cause of intestinal obstruction in the small intestine?
What is the most common cause of intestinal obstruction in the small intestine?
Signup and view all the answers
What is the result of peritonitis in the context of intestinal obstruction?
What is the result of peritonitis in the context of intestinal obstruction?
Signup and view all the answers
What is the process by which a segment of intestine becomes 'telescoped' within a distal segment during peristalsis?
What is the process by which a segment of intestine becomes 'telescoped' within a distal segment during peristalsis?
Signup and view all the answers
What is the characteristic feature of the mucosal surface in ulcerative colitis?
What is the characteristic feature of the mucosal surface in ulcerative colitis?
Signup and view all the answers
What is the percentage of patients with ulcerative colitis who will require colectomy within the first three years?
What is the percentage of patients with ulcerative colitis who will require colectomy within the first three years?
Signup and view all the answers
What is the primary mechanism of diverticulitis formation?
What is the primary mechanism of diverticulitis formation?
Signup and view all the answers
What is the characteristic feature of hyperplastic polyps?
What is the characteristic feature of hyperplastic polyps?
Signup and view all the answers
What is the name of the gene mutation associated with familial adenomatous polyposis (FAP)?
What is the name of the gene mutation associated with familial adenomatous polyposis (FAP)?
Signup and view all the answers
What is the term for the blind pouch leading from the GI tract lined with mucosa?
What is the term for the blind pouch leading from the GI tract lined with mucosa?
Signup and view all the answers
Perforation of the stomach and duodenum can be diagnosed using endoscopy.
Perforation of the stomach and duodenum can be diagnosed using endoscopy.
Signup and view all the answers
Al/Mg hydroxide reduces HCL production in the stomach.
Al/Mg hydroxide reduces HCL production in the stomach.
Signup and view all the answers
The small intestine is approximately 6-7 meters long.
The small intestine is approximately 6-7 meters long.
Signup and view all the answers
The narrow lumen of the small intestine makes it prone to obstruction from scarring and swelling.
The narrow lumen of the small intestine makes it prone to obstruction from scarring and swelling.
Signup and view all the answers
Villi and microvilli in the small intestine decrease the surface area for digestion and absorption.
Villi and microvilli in the small intestine decrease the surface area for digestion and absorption.
Signup and view all the answers
Neutrophils are a marker of severe injury in the oesophagus.
Neutrophils are a marker of severe injury in the oesophagus.
Signup and view all the answers
Gastroscopy is used to detect gastroesophageal reflux disease (GORD).
Gastroscopy is used to detect gastroesophageal reflux disease (GORD).
Signup and view all the answers
Barrett's oesophagus is a complication of long-term damage in 50% of GORD patients.
Barrett's oesophagus is a complication of long-term damage in 50% of GORD patients.
Signup and view all the answers
Oesophageal varices are secondary to liver disease, such as cirrhosis.
Oesophageal varices are secondary to liver disease, such as cirrhosis.
Signup and view all the answers
The stomach produces 3 litres of HCl per day.
The stomach produces 3 litres of HCl per day.
Signup and view all the answers
The main function of the stomach is to absorb nutrients.
The main function of the stomach is to absorb nutrients.
Signup and view all the answers
Bile insufficiency can cause steatorrhea due to the lack of fat emulsification in the small intestine.
Bile insufficiency can cause steatorrhea due to the lack of fat emulsification in the small intestine.
Signup and view all the answers
Pancreatic lipase deficiency is diagnosed using the faecal elastase enzyme test (FE-1).
Pancreatic lipase deficiency is diagnosed using the faecal elastase enzyme test (FE-1).
Signup and view all the answers
Coeliac disease is primarily seen in people of Other Ethnic Groups.
Coeliac disease is primarily seen in people of Other Ethnic Groups.
Signup and view all the answers
Dermititis herpetiformis is a skin blistering lesion seen in 100% of patients with Coeliac disease.
Dermititis herpetiformis is a skin blistering lesion seen in 100% of patients with Coeliac disease.
Signup and view all the answers
Lactase is a brush border enzyme with high activity in adults.
Lactase is a brush border enzyme with high activity in adults.
Signup and view all the answers
Mucosal defects can cause fat malabsorption due to the inability to assemble chylomicrons.
Mucosal defects can cause fat malabsorption due to the inability to assemble chylomicrons.
Signup and view all the answers
The only method to diagnose Coeliac disease with 100% accuracy is by blood test.
The only method to diagnose Coeliac disease with 100% accuracy is by blood test.
Signup and view all the answers
In Coeliac disease, the overall mucosal thickness is decreased.
In Coeliac disease, the overall mucosal thickness is decreased.
Signup and view all the answers
Intussusception is a common cause of intestinal obstruction in the large intestine.
Intussusception is a common cause of intestinal obstruction in the large intestine.
Signup and view all the answers
Dermititis Herpetiformis is a skin manifestation of Coeliac disease in all patients.
Dermititis Herpetiformis is a skin manifestation of Coeliac disease in all patients.
Signup and view all the answers
Gluten-free diet can completely cure Coeliac disease.
Gluten-free diet can completely cure Coeliac disease.
Signup and view all the answers
Surgical adhesions are a common cause of intestinal obstruction in the large intestine.
Surgical adhesions are a common cause of intestinal obstruction in the large intestine.
Signup and view all the answers
Crohn's disease typically affects the terminal ileum, resulting in malabsorption of Vitamin C.
Crohn's disease typically affects the terminal ileum, resulting in malabsorption of Vitamin C.
Signup and view all the answers
Fistulas in Crohn's disease often connect with the skin, bladder, or vagina.
Fistulas in Crohn's disease often connect with the skin, bladder, or vagina.
Signup and view all the answers
Flagellin is a dominant antigen in Ulcerative Colitis (UC) but not in Crohn's disease.
Flagellin is a dominant antigen in Ulcerative Colitis (UC) but not in Crohn's disease.
Signup and view all the answers
Crohn's disease typically presents with continuous colonic involvement beginning in the rectum.
Crohn's disease typically presents with continuous colonic involvement beginning in the rectum.
Signup and view all the answers
Repeated surgery in Crohn's disease can lead to a higher risk of colon cancer.
Repeated surgery in Crohn's disease can lead to a higher risk of colon cancer.
Signup and view all the answers
Crohn's disease is characterized by a sustained viral-induced inflammatory response.
Crohn's disease is characterized by a sustained viral-induced inflammatory response.
Signup and view all the answers
Study Notes
Here is the summary of the text:
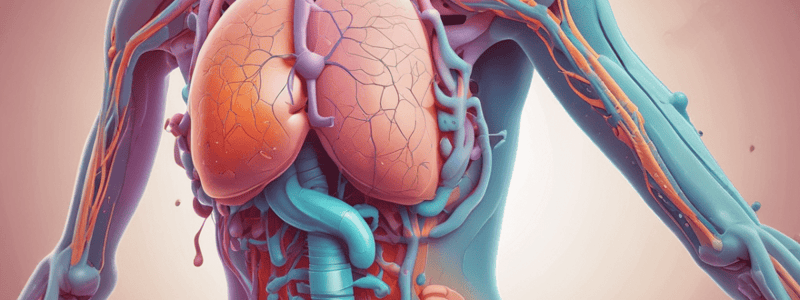
• The GI tract is divided into four functional segments: oesophagus, stomach, small intestine, and large intestine.
• The oesophagus is a four-layered structure with squamous epithelium, two sphincters (upper and lower), and an acute angle, and it moves food bolus via peristalsis coordinated by the oesophageal plexus.
• Disorders of the oesophagus include obstruction, which can cause dysphagia, and oesophagitis, which is inflammation of the oesophageal mucosa.
• Oesophagitis can be caused by central nervous system depressants, pregnancy, alcohol, and anatomical changes, leading to symptoms such as bloody diarrhea, lower abdominal pain, and systemic inflammatory complications.
• Ulcerative colitis (UC) is a clinical feature of oesophagitis, characterized by bloody diarrhea, lower abdominal pain, and similar systemic inflammatory complications to Crohn's disease.
• Differential features of Crohn's disease (CD) and UC include distribution (UC LI, CD SI&LI), wall appearance (CD thick vs UC thin), depth of inflammation (CD high vs UC low), and fistulae (CD).
• Diverticulitis is a rare condition in people under 30, but common in people over 60, and is characterized by a blind pouch leading from the GI tract lined with mucosa, causing infection and serious abdominal infection.
• Treatment for diverticulitis includes a low-fibre diet, reduced stool bulk, increased peristaltic activity, and pressure.
• Polyps are tumorous masses arising from the epithelium protruding into the gut lumen, and can be classified into hyperplastic polyp (non-neoplastic) and adenoma (neoplastic).
• Familial adenomatous polyposis (FAP) is a familial syndrome characterized by a mutation in the Adenomatous Polyposis Coli (APC) gene.
• Coeliac disease is a condition characterized by normal atrophy and loss of villi, intra-epithelial lymphocytes, and crypts elongated, and can be diagnosed by SI biopsy and treated with a gluten-free diet.
• Coeliac intestinal obstruction is a rare condition that can be caused by herniation of segment, surgical adhesions, intussusception, and tumour.
• Gastritis is inflammation of the gastric mucosa due to HCl, which can be acute or chronic, and can lead to ulceration, breach of the 4-layer structure, and stomach content leakage into the peritoneum.
• Disorders of the stomach include chronic infection with H.Pylori, chronic alcohol and tobacco use, immunologic loss of parietal cell function, and achlorydia.
• Malabsorption syndromes can be caused by defective intraluminal digestion, mucosal defects, and reduced SI surface area, leading to symptoms such as chronic diarrhea, steatorrhea, weight loss, anorexia, abdominal distension, and borborygami.
• Disaccharide deficiency is a common condition characterized by lactase deficiency, which can be treated by removing lactose from food.
• Fat malabsorption can be caused by bile insufficiency, pancreatic lipase deficiency, and mucosal defects, leading to symptoms such as greasy stools, weight loss, and abdominal distension.
• Coeliac disease is a gluten-sensitive enteropathy characterized by sensitivity to gluten, T-cell mediated inflammatory reaction, and autoimmune conditions, and can be treated with removal of gluten from the diet.
• Disorders of the oesophagus include gastroscopy to detect oesophagitis, LES reflux oesophagitis, Barrett's oesophagus, and oesophageal varices, which can be secondary to liver disease.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the pathology and medicine of the gastrointestinal tract, including the oesophagus, stomach, small intestine, and large intestine. It builds on the physiology of the GI tract and covers the pathophysiology of diseases in this area. Revision questions on the structure and function of the oesophagus are also included.