Podcast
Questions and Answers
Which of the following is NOT one of the main clinical signs of acute inflammation?
Which of the following is NOT one of the main clinical signs of acute inflammation?
- HYPERPLASIA (correct)
- DOLOR
- RUBOR
- CALOR
What does an exudate imply about the vascular permeability?
What does an exudate imply about the vascular permeability?
- Variable vascular permeability
- Decreased vascular permeability
- Increased vascular permeability (correct)
- Normal vascular permeability
Which of the following best describes the role of neutrophil margination during acute inflammation?
Which of the following best describes the role of neutrophil margination during acute inflammation?
- Destruction of pathogens
- Formation of new blood vessels
- Direction movement towards the injury site (correct)
- Secretion of histamine
What is the primary role of histamine in the immediate early response of acute inflammation?
What is the primary role of histamine in the immediate early response of acute inflammation?
What is the role of increased lymphatic drainage during inflammation?
What is the role of increased lymphatic drainage during inflammation?
Which statement about the immediate sustained response is true?
Which statement about the immediate sustained response is true?
How does the body initially combat injury during acute inflammation?
How does the body initially combat injury during acute inflammation?
Which mechanism is NOT involved in the function of acute inflammation?
Which mechanism is NOT involved in the function of acute inflammation?
What is the role of endogenous pyrogens such as IL1 in the body during acute inflammation?
What is the role of endogenous pyrogens such as IL1 in the body during acute inflammation?
Which of the following is NOT a consequence of systemic effects during acute inflammation?
Which of the following is NOT a consequence of systemic effects during acute inflammation?
Which protein is known for its bactericidal properties and is involved in the acute inflammatory response?
Which protein is known for its bactericidal properties and is involved in the acute inflammatory response?
What may occur after the development of acute inflammation?
What may occur after the development of acute inflammation?
What is the primary function of C-reactive protein (CRP) in the acute phase response?
What is the primary function of C-reactive protein (CRP) in the acute phase response?
Which of the following mechanisms is primarily responsible for the resolution of acute inflammation?
Which of the following mechanisms is primarily responsible for the resolution of acute inflammation?
During acute inflammation, which type of white blood cells typically increases during bacterial infections?
During acute inflammation, which type of white blood cells typically increases during bacterial infections?
In what situation is complete resolution of acute inflammation NOT possible?
In what situation is complete resolution of acute inflammation NOT possible?
What initiates the margination process in neutrophils?
What initiates the margination process in neutrophils?
Which mediator is primarily responsible for the conversion of superoxide ions during microbial killing?
Which mediator is primarily responsible for the conversion of superoxide ions during microbial killing?
What is the main role of prostaglandins and leukotrienes in inflammation?
What is the main role of prostaglandins and leukotrienes in inflammation?
What is a significant effect of oxygen-derived free radicals in the inflammatory process?
What is a significant effect of oxygen-derived free radicals in the inflammatory process?
Which of the following substances is an example of a product from activation of platelets during inflammation?
Which of the following substances is an example of a product from activation of platelets during inflammation?
What mechanism allows neutrophils to detect and respond to foreign substances during their movement?
What mechanism allows neutrophils to detect and respond to foreign substances during their movement?
Which cytokines are specifically mentioned as activating E selectin on the endothelium?
Which cytokines are specifically mentioned as activating E selectin on the endothelium?
How do neutrophils primarily kill microbes once they have internalized them?
How do neutrophils primarily kill microbes once they have internalized them?
What is the primary causative organism of lobar pneumonia?
What is the primary causative organism of lobar pneumonia?
What happens to the alveoli in lobar pneumonia?
What happens to the alveoli in lobar pneumonia?
What typically characterizes a skin blister?
What typically characterizes a skin blister?
Which mechanism signifies 'resolution by crisis' in lobar pneumonia?
Which mechanism signifies 'resolution by crisis' in lobar pneumonia?
In the context of inflammation in serous cavities, what condition may respiratory impairment lead to?
In the context of inflammation in serous cavities, what condition may respiratory impairment lead to?
What type of necrosis is commonly associated with an abscess?
What type of necrosis is commonly associated with an abscess?
Which of the following is a feature not typical of acute inflammation in serous cavities?
Which of the following is a feature not typical of acute inflammation in serous cavities?
What is a common disorder of acute inflammation that results from inherited deficiencies?
What is a common disorder of acute inflammation that results from inherited deficiencies?
Study Notes
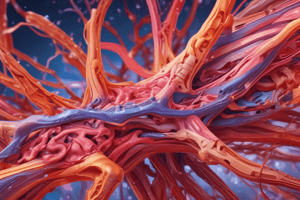
Features of Acute Inflammation
- Main clinical signs include: rubor (redness), tumor (swelling), calor (heat), dolor (pain), and functio laesa (loss of function).
- Described through the ‘triple response’ consisting of brief blanching, followed by reddening, flare, and wheal.
- Microscopic changes involve vascular dilation, increased red blood cell sludging, and fluid leakage into interstitium due to increased vascular permeability.
Definitions of Fluid Types in Inflammation
- Transudate: Low protein content, indicating hydrostatic or oncotic pressure alterations.
- Exudate: High protein content, suggesting an inflammatory process and increased vascular permeability.
Mechanisms of Inflammation
- Vasodilation enhances blood delivery, raises temperature, and aids toxin removal.
- Exudate carries immunoglobulins, dilutes toxins, and facilitates lymphatic drainage.
- Increased lymphatic drainage aids in delivering pathogens to phagocytes and transporting antigens.
Chemical Mediators of Acute Inflammation
- Three phases of response:
- Immediate early response: Histamine release from mast cells, basophils, and platelets causes vascular effects.
- Immediate sustained response: May occur due to direct endothelial cell damage.
- Delayed response: Peaks around 3 hours with numerous chemical mediators involved.
Key Chemical Mediators
- Includes proteases, kinins (e.g., Bradykinin), cytokines (e.g., TNF alpha, IL-1), and arachidonic acid metabolites (e.g., prostaglandins, leukotrienes).
- NSAIDs like aspirin block these mediators.
- Platelets and neutrophils release additional inflammatory substances and mediators.
Neutrophil Role in Inflammation
- Neutrophils marginate and emigrate towards the injury site by binding to the endothelium and moving through vessel walls.
- Diapedesis involves relaxation of endothelial junctions and digestion of the vascular basement membrane.
- They perform phagocytosis and microbial killing through oxygen-dependent and independent mechanisms.
Systemic Effects of Acute Inflammation
- Fever and leukocytosis result from endogenous pyrogens (e.g., IL-1, TNF alpha).
- Acute-phase response is characterized by decreased appetite, altered sleep patterns, and changes in plasma levels of acute-phase proteins (e.g., C-reactive protein).
Problems Caused by Acute Inflammation
- Local complications include swelling, pain, and potential for autoimmunity.
- Systemic issues may involve the spread of microbes or toxins, leading to shock.
Resolution of Acute Inflammation
- Possible outcomes include complete resolution, progression to chronic inflammation, or fibrous repair.
- Morphological changes reverse as neutrophils die, vessel permeability normalizes, and exudate drains.
Clinical Examples
- Lobar Pneumonia: Caused by Streptococcus pneumoniae; affects young adults and alcoholics; characterized by worsening symptoms with resolution upon antibody appearance.
- Skin Blister: Resulting in pain, exudate, and potential tissue damage, particularly if bacterial infection occurs.
- Abscess: Solid tissues separate due to inflammatory exudate leading to liquefactive necrosis and pain.
Disorders of Acute Inflammation
- Rare diseases, such as hereditary angioedema or alpha-1 antitrypsin deficiency, highlight the significance of complex inflammatory mechanisms.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the mechanisms and features of acute inflammation in this quiz. Understand the clinical signs and microscopic changes associated with this pathological condition. Key topics include the triple response of inflammation and vascular dynamics.