Questions and Answers
What is the main form of transport for oxygen in the blood?
Combined with hemoglobin as oxyhemoglobin
Which factor does NOT influence the shape of the oxyhemoglobin dissociation curve?
Hemoglobin structure
How is most of the carbon dioxide transported in the blood?
Mainly as bicarbonate ions
What is described by the term 'hemoglobin saturation'?
Signup and view all the answers
Which physiological effect is associated with the Bohr effect?
Signup and view all the answers
What is the main role of the protoporphyrin ring in hemoglobin?
Signup and view all the answers
Which molecule does oxygen normally combine with when transported in the blood?
Signup and view all the answers
What condition shifts the oxyhemoglobin dissociation curve to the left?
Signup and view all the answers
When the pH of blood falls, what effect leads to a decrease in the oxygen affinity of hemoglobin?
Signup and view all the answers
Which of the following is responsible for promoting oxygen release at the tissue level?
Signup and view all the answers
What is the effect of most hemoglobinopathies on the oxygen dissociation curve?
Signup and view all the answers
What causes a shift to the right in the CO2 dissociation curve by decreasing its affinity for CO2?
Signup and view all the answers
Which gas binds to hemoglobin with an affinity 210 times greater than oxygen?
Signup and view all the answers
Which effect is related to CO2 transport in the blood?
Signup and view all the answers
What is the function of myoglobin in muscle cells?
Signup and view all the answers
What happens to the oxygen dissociation curve in the presence of carbon monoxide?
Signup and view all the answers
What effect does decreased 2,3-diphosphoglycerate (2,3 DPG) have on the oxygen dissociation curve?
Signup and view all the answers
What is the impact of packed cells/banked blood having lower 2,3-DPG levels?
Signup and view all the answers
What is the main determinant of how much oxygen combines with hemoglobin?
Signup and view all the answers
What is the normal arterial oxygen content (CaO2) in mL/dL?
Signup and view all the answers
Which equation is used to calculate the oxygen content of the blood?
Signup and view all the answers
What is the component of the blood's oxygen content that is measured by the PaO2?
Signup and view all the answers
How many molecules/atoms of oxygen can one molecule of Hb combine with?
Signup and view all the answers
What causes acute intermittent porphyria (AIP)?
Signup and view all the answers
What is the solubility coefficient of O2 in blood?
Signup and view all the answers
In what state must the iron molecule be to bind oxygen in hemoglobin?
Signup and view all the answers
What factors cause a right shift in the oxygen-hemoglobin dissociation curve?
Signup and view all the answers
What is the primary effect of the Bohr effect on hemoglobin?
Signup and view all the answers
What causes a left shift in the oxygen-hemoglobin dissociation curve?
Signup and view all the answers
What is the primary role of 2,3 diphosphoglycerate (2,3 DPG) in the context of hemoglobin?
Signup and view all the answers
In which location does a left shift (reverse Bohr effect) predominantly occur?
Signup and view all the answers
Which of the following is responsible for promoting oxygen release at the tissue level?
Signup and view all the answers
What is described by the term 'hemoglobin saturation'?
Signup and view all the answers
Which condition shifts the oxyhemoglobin dissociation curve to the left?
Signup and view all the answers
The Bohr effect leads to an increase in oxygen affinity of hemoglobin at lower pH levels.
Signup and view all the answers
The Haldane effect is primarily associated with oxygen transport in the blood.
Signup and view all the answers
An increase in oxygen levels will shift the CO2 dissociation curve to the left, increasing the affinity for CO2.
Signup and view all the answers
Carbon monoxide (CO) shifts the oxyhemoglobin dissociation curve to the right.
Signup and view all the answers
Hypoventilation causes a right shift in the oxyhemoglobin dissociation curve.
Signup and view all the answers
Study Notes
Transport of Oxygen by the Blood
- Volume of oxygen delivered to the systemic vascular bed per minute = cardiac output x arterial O2 concentration
- Content or concentration of O2 (CaO2) is expressed in ml of O2/100 mL of blood
- Normally expressed as volumes percent = ml O2 per 100 mL of blood
- Oxygen content (concentration):
- 3% O2 dissolved in plasma
- 97% O2 reversibly combined with hemoglobin (Hb)
Calculating Oxygen Content of the Blood
- Oxygen content is composed of hemoglobin bound + dissolved
- Equation for calculating oxygen content of the blood is: (CaO2) = (1.34 x Hb x SaO2) + (PaO2 x 0.003)
Amount of O2 Dissolved in Plasma
- Measured by the PaO2 (partial pressure or oxygen tension)
- Insufficient to fulfill the body's oxygen requirements at rest (normal FiO2 at sea level)
- Solubility coefficient of O2 = 0.003 ml O2/100 ml blood/mmHg (or per deciliter (dL))
- Henry's Law: At a temperature of 37°C, 1 mL of plasma contains 0.00003 mL O2/mm Hg PO2
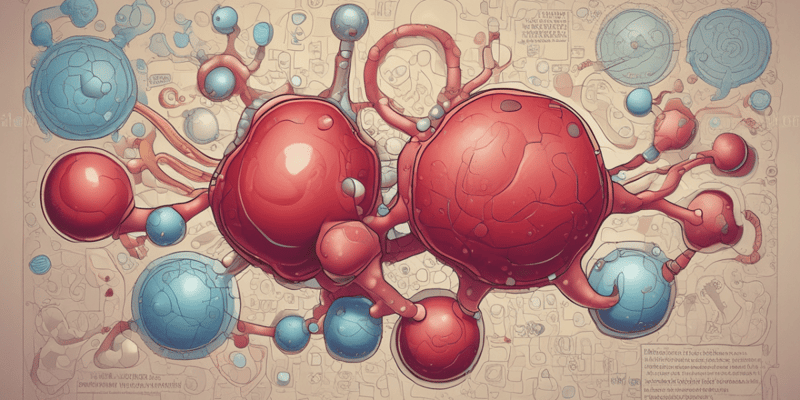
Oxygen Chemically Combined with Hemoglobin
- 97% of oxygen delivered to tissues is combined with hemoglobin (Hb)
- Adult hemoglobin, HbA is a tetramer composed of:
- 4 heme molecules + 4 globin chains
- Cells must synthesize all parts except Fe2+
- Four globin polypeptide chains: 2 α-globin subunits and 2 β-globin subunits
- A heme molecule is a protoporphyrin ring with a suspended iron molecule
- Fe in the Fe2+ state binds O2 - Not the Fe3+ state
- One molecule of Hb combines with 4 molecules/8 atoms of oxygen
Porphyrins
- The heme group is a prosthetic group consisting of a protoporphyrin ring and a central, suspended iron atom
- Acute intermittent porphyria (AIP) is caused by a gene mutation that interferes with cytoplasmic heme synthesis and causes the accumulation of toxic heme precursors
- Any drug that induces ALA synthase can accelerate this process (barbiturates, etomidate, glucocorticoids, hydralazine)
Transport of Carbon Dioxide by the Blood
- Not discussed in this text, but will be covered in the next section
Bohr and Haldane Effects
- Right shift = Bohr effect: CO2 and H+ cause Hb to release oxygen
- Factors that cause a right shift:
- Increased PCO2 from metabolism
- Decreased pH - acidosis (ketoacidosis, lactic acidosis, etc)
- Left shift is due to less [H+] interacting with Hb inside erythrocytes
- Factors that shift the curve to the left:
- Decreased CO2
- Increased pH
- Decreased Temperature
- Decreased 2,3 DPG
- Most hemoglobinopathies
Myoglobin
- Myoglobin is a single-polypeptide heme protein that stores O2 in muscle cells
- Combines with a single molecule O2
- Structurally similar to a single Hb subunit
- Hyperbolic dissociation curve
- P50 far left of HbA
- O2 remains bound for conditions with lower PO2### Transport of Oxygen by the Blood
- The volume of oxygen delivered to the systemic vascular bed per minute is calculated by multiplying cardiac output (CO) by arterial O2 concentration.
- The body has limited stores of oxygen, so limiting cardiac output or pulmonary oxygenation is fatal within minutes.
- Oxygen content (concentration) is expressed in ml of O2/100 mL of blood and is normally around 20 mL/dL.
Calculating Oxygen Content of the Blood
- Oxygen content is composed of hemoglobin-bound and dissolved O2.
- The equation for calculating oxygen content of the blood is: (CaO2) = (1.34 x Hb x SaO2) + (PaO2 x 0.003).
Oxygen Delivery to Tissues
- Oxygen delivery to tissues is approximately 5 mL O2/100 mL blood at rest.
- Cardiac output is normally 5 L/min, and normal arterial O2 content is 20 mL/dL.
- Normal venous O2 content is 15 mL/dL.
Amount of O2 Dissolved in Plasma
- The amount of O2 dissolved in plasma is measured by the PaO2 (partial pressure or oxygen tension).
- The solubility coefficient of O2 is 0.003 ml O2/100 mL blood/mmHg.
- At a temperature of 37°C, 1 mL of plasma contains 0.00003 mL O2/mmHg PO2.
Oxygen Chemically Combined with Hemoglobin
- 97% of oxygen delivered to tissues is combined with hemoglobin (Hb).
- Adult hemoglobin, HbA, is a tetramer composed of 4 heme molecules and 4 globin chains.
- One molecule of Hb combines with 4 molecules/8 atoms of oxygen.
Heme Molecule
- A heme molecule is a protoporphyrin ring with a suspended iron atom (Fe2+).
- Acute intermittent porphyria (AIP) is caused by a gene mutation that interferes with cytoplasmic heme synthesis.
Oxygen Transport and Carbon Dioxide
- Oxygen is transported in the blood as oxyhemoglobin (HbO2) and dissolved O2.
- Carbon dioxide is transported in the blood as carbamino compounds with blood proteins, bicarbonate, and dissolved CO2.
- The oxyhemoglobin dissociation curve shows the relationship between the partial pressure of oxygen and the amount of oxygen combined with hemoglobin.
Porphyrin
- A porphyrin is a heterocyclic compound containing four pyrrole rings arranged in a square with a metal atom in the central cavity.
- Porphyrin is a prosthetic group consisting of a protoporphyrin ring and a central, suspended iron atom.
Cooperative Binding of Hemoglobin (Hb)
- Hb forms a reversible bond with oxygen, allowing O2 to be released to the tissues.
- Hemoglobin occurs in two forms: T or "Tense" form (deoxyhemoglobin) and R or "Relaxed" form (oxyhemoglobin).
O2 Carrying Capacity of Hb
- The O2 carrying capacity of Hb is the maximal amount of O2 that can bind with Hb.
- One gram of Hb can combine with 1.34 ml O2.
Pulse Oximetry
- Pulse oximetry measures the oxygen saturation of Hb, which is the proportion of oxygenated hemoglobin compared to total hemoglobin.
- The calculation to find % Hb saturation is: O2 combined with Hb ÷ O2 carrying-capacity of Hb x 100% = % Hb saturation.
Bohr Effect and Haldane Effect
- The Bohr effect is the decrease in O2 affinity of Hb when the pH of blood falls, causing Hb to release oxygen.
- The Haldane effect is the increase in CO2 affinity of Hb when the pH of blood falls, causing CO2 to combine with Hb.
- The Bohr effect and Haldane effect work in synchrony for uptake and release of O2 and CO2.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.