Podcast
Questions and Answers
What effect does vasodilation have on vascular resistance and pressure?
What effect does vasodilation have on vascular resistance and pressure?
- Decreases resistance and lowers pressure (correct)
- Increases resistance and lowers pressure
- Increases resistance and pressure
- Does not affect resistance or pressure
Which of the following is a direct vasodilator?
Which of the following is a direct vasodilator?
- Alpha1 agonists
- Nitrates (correct)
- Beta blockers
- Calcium channel blockers
Which determinant decreases stroke volume (SV)?
Which determinant decreases stroke volume (SV)?
- Contractility
- Preload
- Heart Rate (HR)
- Afterload (correct)
What is the relationship between mean arterial pressure (MAP) and cardiac output (CO)?
What is the relationship between mean arterial pressure (MAP) and cardiac output (CO)?
What is the role of calcium ions (Ca++) in smooth muscle contraction?
What is the role of calcium ions (Ca++) in smooth muscle contraction?
What is the primary action of nitric oxide (NO) in promoting vasodilation?
What is the primary action of nitric oxide (NO) in promoting vasodilation?
Which condition is NOT associated with reduced bioavailability of nitric oxide?
Which condition is NOT associated with reduced bioavailability of nitric oxide?
What effect do nitrates primarily have on the heart?
What effect do nitrates primarily have on the heart?
What can cause nitrate tolerance?
What can cause nitrate tolerance?
Which of the following statements about calcium channel blockers is true?
Which of the following statements about calcium channel blockers is true?
What is a significant limitation of nitrates compared to other vasodilators?
What is a significant limitation of nitrates compared to other vasodilators?
What consequence might elevated levels of reactive oxygen species (ROS) have in relation to nitric oxide?
What consequence might elevated levels of reactive oxygen species (ROS) have in relation to nitric oxide?
What effect do b-blockers have on heart rate (HR)?
What effect do b-blockers have on heart rate (HR)?
Which of the following best describes the mechanism through which SNS activity increases blood volume?
Which of the following best describes the mechanism through which SNS activity increases blood volume?
What is the primary role of pure b-blockers in the context of blood pressure regulation?
What is the primary role of pure b-blockers in the context of blood pressure regulation?
In which situation might a1 and b1 mixed antagonists, such as carvedilol, be preferred?
In which situation might a1 and b1 mixed antagonists, such as carvedilol, be preferred?
What can happen if reflex tachycardia due to vasodilators is too extreme?
What can happen if reflex tachycardia due to vasodilators is too extreme?
What is one major effect of NO donors on the cardiovascular system?
What is one major effect of NO donors on the cardiovascular system?
Which nitrate is dependent on cysteine (GSH) and ALDH2 for NO liberation?
Which nitrate is dependent on cysteine (GSH) and ALDH2 for NO liberation?
How does nitric oxide (NO) primarily exert its vasodilatory effect in smooth muscle cells?
How does nitric oxide (NO) primarily exert its vasodilatory effect in smooth muscle cells?
Which compound is primarily used for acute angina treatment due to its rapid onset?
Which compound is primarily used for acute angina treatment due to its rapid onset?
What is the role of Protein Kinase G (PKG) in the mechanism of NO-induced vasodilation?
What is the role of Protein Kinase G (PKG) in the mechanism of NO-induced vasodilation?
What effect does PKG have on vessel contraction in smooth muscle cells?
What effect does PKG have on vessel contraction in smooth muscle cells?
Which signaling cascade primarily leads to the activation of eNOS in endothelial cells?
Which signaling cascade primarily leads to the activation of eNOS in endothelial cells?
What is the primary role of nitric oxide (NO) in vascular smooth muscle cells (VSMC)?
What is the primary role of nitric oxide (NO) in vascular smooth muscle cells (VSMC)?
What is the end product of the activation of adenylate cyclase in smooth muscle?
What is the end product of the activation of adenylate cyclase in smooth muscle?
How do nitrates function in vascular dilation?
How do nitrates function in vascular dilation?
Which of the following is NOT a part of the signaling pathway for vessel contraction?
Which of the following is NOT a part of the signaling pathway for vessel contraction?
What is the effect of cGMP in vascular smooth muscle cells?
What is the effect of cGMP in vascular smooth muscle cells?
What happens as a result of increased K+ efflux in smooth muscle cells?
What happens as a result of increased K+ efflux in smooth muscle cells?
What is the primary action of b1 adrenergic receptors in the heart when activated?
What is the primary action of b1 adrenergic receptors in the heart when activated?
How do beta-blockers affect heart rate?
How do beta-blockers affect heart rate?
Which type of beta-blocker is designed to avoid affecting b2 mediated vasodilation?
Which type of beta-blocker is designed to avoid affecting b2 mediated vasodilation?
What effect do beta-blockers have on contractility?
What effect do beta-blockers have on contractility?
What is a common use of beta-blockers in blood pressure management?
What is a common use of beta-blockers in blood pressure management?
How do beta-blockers reduce blood pressure?
How do beta-blockers reduce blood pressure?
Which of the following describes a characteristic of mixed antagonists among beta-blockers?
Which of the following describes a characteristic of mixed antagonists among beta-blockers?
What role does PKA play in the action of b1 adrenergic receptors?
What role does PKA play in the action of b1 adrenergic receptors?
Flashcards
What is contractility?
What is contractility?
The force of the heart contracting.
What is afterload?
What is afterload?
This reflects the pressure the heart must generate to open the aortic valve.
What is preload?
What is preload?
This is the amount of blood returning to the heart from the veins.
What is stroke volume?
What is stroke volume?
Signup and view all the flashcards
What is vasoconstriction?
What is vasoconstriction?
Signup and view all the flashcards
How do NO donors reduce preload?
How do NO donors reduce preload?
Signup and view all the flashcards
How do NO donors help with partially blocked vessels?
How do NO donors help with partially blocked vessels?
Signup and view all the flashcards
Explain how nitroglycerin (GTN) works.
Explain how nitroglycerin (GTN) works.
Signup and view all the flashcards
Describe the signaling pathway leading to NO-induced vasodilation.
Describe the signaling pathway leading to NO-induced vasodilation.
Signup and view all the flashcards
What happens when the endothelium is damaged?
What happens when the endothelium is damaged?
Signup and view all the flashcards
Rho Kinase
Rho Kinase
Signup and view all the flashcards
MLC Dephosphorylation
MLC Dephosphorylation
Signup and view all the flashcards
MLC Phosphorylation
MLC Phosphorylation
Signup and view all the flashcards
eNOS Activation
eNOS Activation
Signup and view all the flashcards
Soluble Guanylate Cyclase
Soluble Guanylate Cyclase
Signup and view all the flashcards
PKG Activation
PKG Activation
Signup and view all the flashcards
PKA Activation in VSMCs
PKA Activation in VSMCs
Signup and view all the flashcards
Vasodilators and cAMP Signaling
Vasodilators and cAMP Signaling
Signup and view all the flashcards
Baroreceptor Reflex
Baroreceptor Reflex
Signup and view all the flashcards
Beta-blockers and Baroreceptor Reflex
Beta-blockers and Baroreceptor Reflex
Signup and view all the flashcards
Reflex Tachycardia
Reflex Tachycardia
Signup and view all the flashcards
Beta-1 Selective Blockers
Beta-1 Selective Blockers
Signup and view all the flashcards
Alpha-1 and Beta-1 Mixed Antagonists
Alpha-1 and Beta-1 Mixed Antagonists
Signup and view all the flashcards
What are beta-blockers?
What are beta-blockers?
Signup and view all the flashcards
What are beta-1 receptors?
What are beta-1 receptors?
Signup and view all the flashcards
What are beta-2 receptors?
What are beta-2 receptors?
Signup and view all the flashcards
How specific are beta-blockers?
How specific are beta-blockers?
Signup and view all the flashcards
How do beta-blockers affect heart rate?
How do beta-blockers affect heart rate?
Signup and view all the flashcards
How do beta-blockers affect contractility?
How do beta-blockers affect contractility?
Signup and view all the flashcards
How do beta-blockers lower blood pressure?
How do beta-blockers lower blood pressure?
Signup and view all the flashcards
Why are beta-blockers used in combination therapy to lower blood pressure?
Why are beta-blockers used in combination therapy to lower blood pressure?
Signup and view all the flashcards
What is the primary mechanism of action for Nitric Oxide?
What is the primary mechanism of action for Nitric Oxide?
Signup and view all the flashcards
How does NO availability become reduced in certain diseases?
How does NO availability become reduced in certain diseases?
Signup and view all the flashcards
How do nitrates affect blood vessels and what is their primary clinical effect?
How do nitrates affect blood vessels and what is their primary clinical effect?
Signup and view all the flashcards
What is nitrate tolerance and what are its potential mechanisms?
What is nitrate tolerance and what are its potential mechanisms?
Signup and view all the flashcards
What is the primary mechanism of action for dihydropyridine Ca++ channel blockers?
What is the primary mechanism of action for dihydropyridine Ca++ channel blockers?
Signup and view all the flashcards
What is the primary mechanism of action for non-dihydropyridine Ca++ channel blockers?
What is the primary mechanism of action for non-dihydropyridine Ca++ channel blockers?
Signup and view all the flashcards
What is a common side effect of Ca++ channel blockers and what mechanism underlies it?
What is a common side effect of Ca++ channel blockers and what mechanism underlies it?
Signup and view all the flashcards
Study Notes
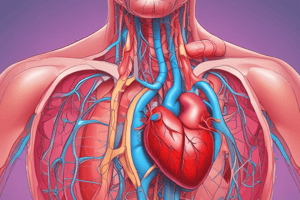
Vasodilators and Adrenergic Antagonists
- Vasodilators and adrenergic antagonists are used in blood pressure management
- Blood pressure is controlled by vasodilation and contraction
- Drugs that induce vasodilation are used to lower blood pressure
- Direct vasodilators include nitrates, hydralazine, and PDE5i
- Other direct vasodilators include K+ channel agonists and calcium channel blockers
- Alpha2 agonists and Alpha1 antagonists are also used
- Beta blockers are another group of drugs used in blood pressure management
Blood Pressure Basics
- Blood pressure is calculated as cardiac output (CO) divided by systemic vascular resistance (SVR)
- CO is calculated as Stroke volume (SV) multiplied by Heart rate (HR)
- Stroke volume is determined by preload (venous return), afterload (blood pressure and cardiac wall stress) and contractility
- Blood pressure is dependent on SVR and CO
- CO depends on HR, preload, afterload, and contractility
Vasoconstriction and Vasodilation
- Vasoconstriction decreases blood vessel radius, thus cross-sectional area, increasing resistance and blood pressure
- Vasodilation increases blood vessel radius, thus cross-sectional area, decreasing resistance and lowering blood pressure
- Resistance (R) is calculated as Mean Arterial Pressure (MAP) divided by Cardiac Output (CO)
- Remember P= R*Q
Molecular Basis of Smooth Muscle Contraction
- Agonists activate receptors, turning on plasma membrane calcium channels
- Depolarization and signaling in smooth muscle releases intracellular calcium stores via IP3 Receptors
- Intracellular calcium activates MLCK
- MLCK phosphorylates MLC, activating myosin and causing vessel contraction
Molecular Basis of VSMC Dilation
- Receptor-activated signaling cascades activate nitric oxide synthase (eNOS)
- NO diffuses to vascular smooth muscle cells (VSMCs)
- NO activate soluble guanylate cyclase (SGC)
- SGC converts GTP to cyclic GMP
- cGMP activates protein kinase G (PKG)
- PKG limit VSMC contraction
- Decrease Ca++ influx/release
- Increase K+ efflux
PKA and Smooth Muscle Dilation
- Vasodilators can activate adenylate cyclase, making cAMP
- cAMP activates PKA
- PKA opposes MLCK effects and activates MLCP to reduce contraction
- This action is the opposite of PKA in the heart
Summary of VSMC Signaling
- Vessel dilation and contraction lead to flow changes
- Signaling mechanisms include receptor signaling, intracellular calcium release, MLCK activation, and MLC phosphorylation in contraction and in dilation; Receptor signaling, NO generation, cGMP production, and PKG activation
Nitrates
- Nitrates are potent vasodilators by releasing nitric oxide (NO)
- NO mainly causes venous dilation, decreasing venous return and preload
- Nitrates can also dilate large blood vessels, and increase coronary flow, with minimal effect on resistance vessels
Nitrates: Compounds
- GTN, isoglyceryl trinitrate, is dependent on cysteine and ALDH2 for NO release
- Rapid onset and short half-life (1-3 min)
- ISDN is a slow-onset, long half-life nitrate
- ISMN is another slow-onset, long half-life nitrate
- Sodium Nitroprusside (SNP) is a fast-acting IV NO donor
- Nitrates rapidly inactivated for systemic effects
NO in smooth muscle
- NO promotes vasodilation produced by eNOS in the endothelium
- NO diffuses to the smooth muscle
- NO stimulates guanylate cyclase, creating cGMP
- cGMP activates PKG which induces a coordinated response to promote vasodilation
Reduced NO and Endothelial Dysfunction
- NO availability may be reduced in diseases such as diabetes, hyperlipidemia, and others with inflammatory conditions
- Conditions like endothelial dysfunction due to disruption in eNOS or increases in inflammatory ROS
- ROS can transform NO into ONOO(peroxynitrite) which is a potent antioxidant.
Nitrates and Areas of Action
- Nitrates increase vein dilation and decrease preload
- They dilate larger conduit vessels but have less effect on resistance vessels
- Nitrates lower afterload but have a milder effect compared to other agents
Nitrate Tolerance
- Prolonged/frequent nitrate use can cause tolerance and ineffectiveness
- Tolerance may involve changes in processing enzymes or damage to relaxation signaling via nitroso radicals
- Limiting high doses and intermitten therapy can prevent tolerance
Hydralazine
- Hydralazine is a potent arteriolar vasodilator acting directly on smooth muscle
- Multiple/ complex mechanism of action, including K+ channel activation and reduced calcium release
- It limits reactive oxygen species and may promote vasodilator production.
Hydralazine Treatment
- Onset within 1-2 hours (oral) and longer half-life depending on patient metabolism potentially reaching 100 hours
- Often used with NO donors such as ISDN for chronic treatment
- Risk of acute/extreme drop in BP and hypoperfusion
- Patients should receive beta-blocker before Hydralazine, to prevent baroreceptor reflex
Hydralazine Summary
- Potent arteriolar vasodilator
- Less effect on veins and preload compared to NO donors
- Blocks contraction pathways via reduced ROS and reduced IP3R activation (Ca++ release)
- Likely increases K+ channel activation for vasodilation
- High risk of reflex tachycardia
PDE5 Inhibitors
- Phosphodiesterases cleave cyclic nucleotides including cGMP
- PDE5 is specific to cGMP degradation
- NO dependent vasodilation involves activation of guanylyl cyclase and conversion of GTP to cGMP
- PDE5i increases VSD and keeps cGMP level elevated
- More pronounced effects in pulmonary vasculature
- Associated with anti-fibroproliferative responses; Sildenafil and tadalafil are examples.
PDE5 in smooth muscle cells
- NO promotes vasodilation
- NO activates guanylyl cyclase in smooth muscle cells to convert GTP to cGMP
- PDE5 inhibitors prevent cGMP degradation
- This leads to increased cGMP, activating PKG to induce vascular smooth muscle contraction
- PKG promotes a coordinated response to promote vasodilation
- Inhibit Ca2+ channels and Ca2+ release
- Activates myosin phosphatase to reduce myosin phosphorylation
PDE5i
- Sildenafil, tadalafil, vardenafil, and avanafil are examples
- More effective for pulmonary vasodilation and lower pressures in pulmonary hypertension
- Increased risks of headaches, flushing, epistaxis, and dyspepsia
- Contraindicated with other vasodilators due to risk of hypotension.
- Patients might need lower starting dose if on alpha blockers
Nitrates and PDE5 Inhibitors
- Nitrates and PDE5i can have combining negative feedback mechanisms leading to dangerous blood pressure drops
- Avoid using nitrates within 12-24 hours post administration of PDE5 inhibitors
PDE5 Summary; Things to Know
- PDE5 breaks down cGMP, antagonizing NO-cGMP-PKG dependent vasodilation
- PDE5 inhibitors promotes cGMP accumulation
- Used mainly for pulmonary circulation relaxation
- Major concern for hypotension and contraindicated with nitrates and sGC stimulators
Ca Channels and Ca channel blockers
- Voltage gated calcium channels (L-type channels) have five subunits
- Calcium channel blockers (CCBs) work on the a1 subunit of the L-type channels allowing calcium movement in.
Ca+ channel blockers
- Dihydropyridines reduce peripheral and coronary vascular resistance, affecting the L-type calcium channel a1 subunit
- Also blocks cardiac contractility, including amlodipine, clevidipine, felodipine
Ca++ channels and vasoconstriction
- Many stimuli result in increased calcium influx through L-type voltage-gated calcium channels
- Cytosolic calcium increases initiating signaling cascades
- Activation of MLCK and other MLC phosphorylation cascades increases contraction
- Calcium channel blockers (CCBs) do not effectively promote venous dilation
Main effects of Ca+ channel blockers
- Dihydropyridines (DHP) and non-DHPs increase systemic vasodilation, decrease resistance, and decrease afterload
- DHPs reduce cardiac contractility (inotropy) more than non-DHPs
- Non-DHPs decrease heart rate and conduction
- Both types lower blood pressure by decreasing stroke volume and cardiac output
Types of Ca+ channel blockers
- Dihydropyridines (e.g., amlodipine, nifedipine) primarily affect vascular smooth muscle
- Non-dihydropyridines (e.g., verapamil, diltiazem) primarily affect cardiac muscle and nodal tissue
Ca channel blockers: side effects
- DHPs can cause reflex tachycardia due to a drop in blood pressure
- Vasodilation initiates a baroreceptor reflex to increase HR to normalize blood pressure
- Formulations with delayed release drugs help mitigate this to some extent.
- DHPs can lower heart rate and conduction, but this doesn't always overcome an initial tachycardia.
Summary: CCB
- Ca++ channel blockers reduce Ca++ entry into vascular smooth muscle and cardiomyocytes
- Block vasoconstriction by limiting MLC phosphorylation
- Decrease cardiac afterload and cardiomyocyte contraction
- Decrease vascular contractility and heart rate
- Diltiazem and Verapamil are non-DHPs
- These drugs affect and reduce the heart rate via blocking SA and AV nodal recovery of Ca+ channels.
- DHPs have more affects on vessels than non-DHPs
K+ channels and vasodilation
- K+ channels on vascular smooth muscle plasma membranes promote vasodilation
- Activated Ca++ channel activation increases cytosolic Ca++ which in turn increase positive charges in the cell.
- Opening of K+ channels cause K+ efflux and cause a negative charge in the cell, known as "hyper-polarization"
- This hyperpolarization promotes vasodilation
K+ channels in vasomotor regulation
The diagram illustrates the cellular processes involved in vasomotor regulation, showing the interplay between nitric oxide (NO) signaling, calcium channels, and potassium channels, which ultimately leads to vasodilation or vasoconstriction.
- Diagram displays the roles of NO, calcium ions, and potassium ion channels in smooth muscle cells.
K+ channel openers
- Minoxidil and diazoxide are K+ channel openers, used in severe hypertension resistant to other treatments
- Minoxidil has a major risk of hypotension and adverse myocardial effects.
- Diazoxide is also associated with hyperinsulinemic hypoglycemia
α2-AR agonists
- α2-agonists decrease blood pressure by stimulating α2 receptors in the brain.
- This reduces SNS outflow and increases vagal tone.
- Decreasing vascular constriction, lowering heart rate, and reducing systemic vascular resistance lowers blood pressure
- Drugs such as clonidine and methyldopa are examples
α2-AR agonists
- Clonidine and methyldopa are the two primary drugs in this category.
- Clonidine is not a first-line agent, whereas methyldopa is usually a preferred option in pregnancy-induced hypertension.
- Common side effects include sodium and water retention (more pronounced with methyldopa), orthostatic hypotension, and a risk of rebound hypertension
α1-AR antagonists
- α1-receptor antagonists such as doxazosin and prazosin can be used to treat hypertension
- In particular, these drugs help reduce peripheral resistance and lower blood pressure
- These may require additional diuretics to prevent edema due to water/sodium retention.
α-AR agents and BP summary
- α2 agonists are used to decrease blood pressure as an alternative to first-line agents
- They act centrally, reducing SNS signal
- α1-antagonists effectively lower SVR and thus blood pressure
- Not a preferred first-line medication due to adverse events versus other agents but useful as an alternative
- They work by blocking NE/EPI activation of a1-AR and the subsequent MLC phosphorylation cascades
Beta-blockers
- β1 receptors are found in the heart and cause increased HR and contractility when activated
- β2 receptors are found in the vasculature and cause vasodilation
- Beta blockers can be nonspecific or Beta 1 specific
Sympathetic stimulation of heart rate
- Activation of β1 receptors increases Na+ current through "funny" channels, leading to increased cytosolic Ca++, which in turn opens Ca++ channels and increases HR
β-blocker effect on heart rate
- β-blockers cause slower Na+ influx through "funny" channels and limiting PKA-dependent increases in channel opening due to affecting the channel response time to reach threshold of Ca+ to be released. This ultimately decreases heart rate and reduces CO
B1-AR PKA activation promotes Ca++ release
- PKA increases Ca+ release through direct modulation of Ca++ release through RyR and external Ca++ channels
- PKA phosphorylates and inhibits PLB, which allows Ca++ stores to increase
- β-blockers inhibit this process, reducing contractility and CO
Adrenergic Antagonists
A branching diagram showing different categories of adrenergic receptor antagonists:
- α-receptor antagonists including nonselective, α1-selective, and α2-selective
- β-receptor antagonists including nonselective, β1-selective, and β2-selective
β-blockers
- Beta blockers can reduce blood pressure by decreasing HR and contractility
- Beta1 selective are preferred to leave beta2 intact
- Mixed antagonists (e.g., carvedilol) have both α and β effects
- Newer drugs like nebivolol also has NO-donor moiety which promotes vasodilation.
Reflex Tachycardia
- Beta-blockers in combination therapy with vasodilators help limit reflex tachycardia
- When vasodilators cause a drop in blood pressure, the baroreceptors activate SNS and increase HR and CO to restore pressure;
- β-blockers decrease SNS response preventing reflex tachycardia from occurring.
Summary β-blockers and BP
- Pure β-blockers do not directly cause vasodilation or decrease SVR
- Decrease SNS which ultimately decrease CO
- Decrease HR, and contractility, subsequently decreases CO
- Decrease reflex actions (to raise BP)
- β1 selective are preferred
Preferred Combinations for Hypertension
Different drug combinations for managing hypertension, grouped as preferred, acceptable, and less effective.
A note about the upcoming test
- Always read the question thoroughly
- Answer choices may be accurate but incorrect in context
- Students often miss when an accurate answer is inappropriate for the question
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the effects of vasodilation, the role of nitric oxide, and the mechanisms affecting cardiac output. This quiz covers various topics related to vascular resistance, cardiovascular pharmacology, and smooth muscle contraction. Dive into the nuances of calcium ions, heart rate, and the implications of reactive oxygen species in circulation.