Podcast
Questions and Answers
What is the primary mechanism of tissue damage in celiac disease?
What is the primary mechanism of tissue damage in celiac disease?
- Stimulation of CD4+ T cells by gliadin peptides to produce cytokines (correct)
- Release of pro-inflammatory cytokines by macrophages and neutrophils
- Activation of CD8+ intraepithelial T-cells by IL-15
- Autoantibody production against intestinal epithelial cells
Which of the following is a risk factor for Clostridioides difficile infection?
Which of the following is a risk factor for Clostridioides difficile infection?
- Family history of inflammatory bowel disease
- Recent travel to a tropical country
- History of liver transplantation
- Previous antibiotic use (correct)
What is the most common cause of intestinal obstruction in children younger than 2 years old?
What is the most common cause of intestinal obstruction in children younger than 2 years old?
- Intussusception (correct)
- Hernias
- Adhesions
- Volvulus
What is the characteristic laboratory finding in abetalipoproteinemia?
What is the characteristic laboratory finding in abetalipoproteinemia?
What is the primary mechanism of paralytic ileus?
What is the primary mechanism of paralytic ileus?
Which of the following is a complication of diverticulitis?
Which of the following is a complication of diverticulitis?
What is the primary difference between Crohn's disease and ulcerative colitis?
What is the primary difference between Crohn's disease and ulcerative colitis?
What is the primary mechanism of inflammation in inflammatory bowel disease?
What is the primary mechanism of inflammation in inflammatory bowel disease?
What is the primary symptom of acute pancreatitis?
What is the primary symptom of acute pancreatitis?
What is the most common cause of acute pancreatitis?
What is the most common cause of acute pancreatitis?
Flashcards are hidden until you start studying
Study Notes
Disorders of Upper GI
Gastric Phase
- Food triggers vagovagal reflexes, stimulating gastrin secretion
- Acidification of the gastric antrum stimulates somatostatin production
- Somatostatin inhibits gastrin release and acid secretion
- Vagal acetylcholine inhibits somatostatin production
NSAIDs and Gastric Mucosa
- NSAIDs reduce acid secretion
- Disruption of protective mechanisms leads to gastropathy/gastritis
- Inhibition of COX by NSAIDs, inhibition of gastric bicarbonate transporters by ammonium ions, reduced mucin and bicarbonate secretion, and decreased oxygen delivery
H. Pylori and Gastric Cancer
- H. pylori is implicated in almost all non-NSAID-induced GI mucosal inflammation
- H. pylori causes type B gastritis (antrum and body of the stomach)
- Almost all patients with gastric cancer have had H. pylori or gastric ulcer
Carcinoid Tumors
- Carcinoid tumors secrete serotonin
- Serotonin is secreted into the hepatic portal circulation
Bile Composition and Jaundice
- Major components of bile: bilirubin, bile salts, cholesterol, phospholipids
- Normal serum bilirubin: 0.3-1.2 mg/dL
- 2-2.5 mg/dL and above: jaundice
- Unconjugated bilirubin is insoluble and cannot be excreted in urine
- Conjugated bilirubin is water-soluble and bound to serum albumin, allowing excretion in urine
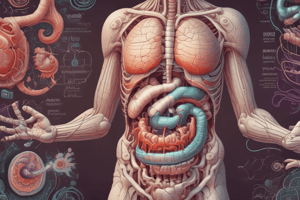
GI Tract Layers
- Mucosa: specialized epithelial cells lining the lumen
- Lamina propria: contains small blood and lymphatic vessels, immune cells, and nerve fibers
- Muscularis mucosa: used to determine if cancer of the GIT is still localized
- Submucosa: contains larger blood and lymphatic vessels
- Muscularis: responsible for motility of the GIT
- Serosa: outermost layer
Enteric Nervous System
- Enteric neurons are organized into submucosal and myenteric plexuses
- PNS efferents stimulate intestinal motility and exocrine secretion
Hormones and Paracrine Factors
- Gastrin: stimulates acid secretion and growth of gastric oxyntic gland
- CCK: stimulates gallbladder contraction, pancreatic enzyme and bicarbonate secretion, and growth of exocrine pancreas
- Secretin: stimulates pancreatic bicarbonate secretion, growth of exocrine pancreas, and pepsin secretion
- GIP: stimulates insulin release and inhibits gastric acid secretion
- Motilin: stimulates gastric and duodenal motility
- Somatostatin: inhibits release of most other peptide hormones
- Prostaglandins: promote blood flow, increase mucus and bicarbonate secretion from gastric mucosa
- Histamine: stimulates gastric acid secretion
- Serotonin: increases intestinal motility and secretion
- VIP: relaxes sphincters and gut circular muscle, stimulates intestinal and pancreatic secretion
Diseases of the Upper GI
- Zollinger-Ellison syndrome: gastrin-producing tumors
- GERD: complication of Barrett's esophagus
- Barrett's esophagus: GI metaplasia of the lower esophagus that results from chronic GERD-induced esophagitis
- Achalasia: caused by degeneration of neurons in the esophageal wall → loss of inhibitory innervation in the LES### Abdominal Distention after Milk Ingestion
- Congenital lactase deficiency: mutations in the lactase gene, leading to explosive diarrhea, watery, frothy stool, and abdominal distention after milk ingestion
- Acquired lactase deficiency: loss of lactase gene expression early in childhood, manifesting after weaning from breast milk
- Transient lactase deficiency: reversible, caused by small bowel injury, infectious or inflammatory insults
Diarrhea
- Time-dependent water absorption responsible for normal stool consistency
- Acute diarrhea: < 2 weeks, usually due to infectious causes
- Chronic diarrhea: > 4 weeks, often due to medication side effects, infectious, toxic, or dietary causes
- Osmotic diarrhea/malabsorption: caused by glucose-galactose or fructose malabsorption, lactulose therapy, bacterial overgrowth, and defective fat solubilization
Pseudomembranous Colitis
- Purulent inflammation of the bowel inner lining, suggestive of C. diff infection
- Presents with watery diarrhea, lower abdominal pain, and fever
- Toxin released by C. diff leads to ribosylation of small GTPases, disrupting epithelial cytoskeleton, tight junction barrier, and causing cytokine release and apoptosis
- Lab findings: leukocytosis, hypoalbuminemia, and lactic acidosis (severe)
- Diagnosis: stool studies, abdominal imaging to rule out toxic megacolon, bowel perforation, and other surgical interventions
- Risk factors: history of recent antibiotic use, hospitalization, age > 65
Celiac Disease
- Immune-mediated disorder triggered by gluten ingestion
- Gluten is digested into amino acids and peptides, including α-gliadin peptide, which is resistant to degradation
- Immune mechanisms: innate (CD8+ intraepithelial T-cells, activated by IL-15) and adaptive (CD4+ T cells and B-cells sensitization to gliadin)
- Gliadin peptides interact with HLA-DQ2 or HLA-DQ8, stimulating CD4+ T cells to produce cytokines that exacerbate tissue damage
- Almost all people with celiac disease carry the HLA-DQ2 or HLA-DQ8 allele
Intestinal Obstruction
- Most common: small intestine (narrow lumen)
- Hernias, intestinal adhesions, intussusception, and volvulus account for 80% of mechanical obstructions
Intussusception
- Occurs when a segment of intestine telescopes into the distal segment
- Most common cause of intestinal obstruction in children under 2 years old
- Etiology: idiopathic, viral infection, and rotavirus vaccines
Betalipoproteinemia
- Autosomal recessive disease, characterized by inability to assemble triglyceride-rich lipoproteins
- Caused by mutation in microsomal triglyceride transfer protein (MTP)
- Presents in infancy with failure to thrive, diarrhea, and steatorrhea
- Failure to absorb essential fatty acids, leading to deficiencies of fat-soluble vitamins and lipid membrane defects
Paralytic Ileus
- Spasms or ileus, which is a failure of normal intestinal motility
- Often occurs after intestinal or abdominal surgery, acute pancreatitis, intestinal infection, cardiac dysfunction, or hypokalemia
- Strangulated obstruction can lead to blood flow compromise, intestinal ischemia, necrosis, or perforation if left untreated
Diverticular Disease
- Herniation of mucosa and submucosa through the muscular layer, often at the site of arterial insertion
- Predisposed by chronic constipation and connective tissue disease
Diverticulitis
- Irritation or obstruction of diverticular entrance, leading to closure and infection
- May cause perforation, abscess, or fistula with surrounding structures
Inflammatory Bowel Disease (IBD)
- Chronic inflammatory condition triggered by the host immune response to intestinal microbes in genetically predisposed individuals
- Encompasses two entities: Crohn disease and ulcerative colitis
- Pathogenesis: involves the presentation of microbial antigens to CD4+ helper T cells, which are induced to differentiate into Th1 and Th17 cells
Exocrine Pancreas
- Normal pancreas: main pancreatic duct (duct of Wirsung) joins the common bile duct, and the accessory pancreatic duct (duct of Santorini) drains into the duodenum
- Pancreatic divisum: failure of fusion of the fetal duct systems, leading to the bulk of the pancreas draining into the duodenum through the minor papilla
Pancreatitis
- Acute pancreatitis: reversible inflammatory disorder, medical emergency, caused by autodigestion of the pancreas by intraacinar activation of pancreatic enzymes
- Marker: serum lipase
- Causes: gallstone, chronic excessive alcohol use, non-gallstone-related obstruction, metabolic disorders, medications, and infections
- Chronic pancreatitis: long-standing inflammation, leading to irreversible destruction of the exocrine pancreas, followed by loss of the islets of Langerhans
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.