Podcast
Questions and Answers
What is the primary function of Zone I in the liver?
What is the primary function of Zone I in the liver?
- Oxidative metabolism, ureagenesis, and bile acid production (correct)
- Protein synthesis and storage of glycogen
- Fatty acid synthesis and cholesterol metabolism
- Glycolysis, ketogenesis, and detoxification reactions
What is the term for the space between hepatocytes and endothelial cells?
What is the term for the space between hepatocytes and endothelial cells?
- Space of Disse (correct)
- Central vein
- Hepatic sinusoid
- Portal triad
What is the primary function of stellate cells?
What is the primary function of stellate cells?
- Regulating glucose metabolism and storing glycogen
- Producing cholesterol and regulating lipoprotein lipase
- Producing bile and regulating vitamin D
- Antigen-presenting cells and storing vitamin A (correct)
What is the term for the liver's role in regulating iron levels?
What is the term for the liver's role in regulating iron levels?
What is the term for the obstruction of the common hepatic duct?
What is the term for the obstruction of the common hepatic duct?
What is the term for the passage of bilirubin into the skin, causing yellowish discoloration?
What is the term for the passage of bilirubin into the skin, causing yellowish discoloration?
What is the term for the most common liver disease in Western countries?
What is the term for the most common liver disease in Western countries?
What is the term for the irreversible distortion of normal liver architecture?
What is the term for the irreversible distortion of normal liver architecture?
What is the term for the virus that causes hepatitis A?
What is the term for the virus that causes hepatitis A?
What is the term for the hepatitis virus that requires HBV helper function to cause infection?
What is the term for the hepatitis virus that requires HBV helper function to cause infection?
Flashcards are hidden until you start studying
Study Notes
Disorders of Upper GI
Gastric Phase
- Food triggers vagovagal reflexes, stimulating gastrin secretion
- Acidification of the gastric antrum stimulates somatostatin production
- Somatostatin inhibits gastrin release and acid secretion
- Vagal acetylcholine inhibits somatostatin production
NSAIDs and Gastric Mucosa
- NSAIDs reduce acid secretion
- Disruption of protective mechanisms leads to gastropathy/gastritis
- Inhibition of COX by NSAIDs, inhibition of gastric bicarbonate transporters by ammonium ions, reduced mucin and bicarbonate secretion, and decreased oxygen delivery
H. Pylori and Gastric Cancer
- H. pylori is implicated in almost all non-NSAID-induced GI mucosal inflammation
- H. pylori causes type B gastritis (antrum and body of the stomach)
- Almost all patients with gastric cancer have had H. pylori or gastric ulcer
Carcinoid Tumors
- Carcinoid tumors secrete serotonin
- Serotonin is secreted into the hepatic portal circulation
Bile Composition and Jaundice
- Major components of bile: bilirubin, bile salts, cholesterol, phospholipids
- Normal serum bilirubin: 0.3-1.2 mg/dL
- 2-2.5 mg/dL and above: jaundice
- Unconjugated bilirubin is insoluble and cannot be excreted in urine
- Conjugated bilirubin is water-soluble and bound to serum albumin, allowing excretion in urine
GI Tract Layers
- Mucosa: specialized epithelial cells lining the lumen
- Lamina propria: contains small blood and lymphatic vessels, immune cells, and nerve fibers
- Muscularis mucosa: used to determine if cancer of the GIT is still localized
- Submucosa: contains larger blood and lymphatic vessels
- Muscularis: responsible for motility of the GIT
- Serosa: outermost layer
Enteric Nervous System
- Enteric neurons are organized into submucosal and myenteric plexuses
- PNS efferents stimulate intestinal motility and exocrine secretion
Hormones and Paracrine Factors
- Gastrin: stimulates acid secretion and growth of gastric oxyntic gland
- CCK: stimulates gallbladder contraction, pancreatic enzyme and bicarbonate secretion, and growth of exocrine pancreas
- Secretin: stimulates pancreatic bicarbonate secretion, growth of exocrine pancreas, and pepsin secretion
- GIP: stimulates insulin release and inhibits gastric acid secretion
- Motilin: stimulates gastric and duodenal motility
- Somatostatin: inhibits release of most other peptide hormones
- Prostaglandins: promote blood flow, increase mucus and bicarbonate secretion from gastric mucosa
- Histamine: stimulates gastric acid secretion
- Serotonin: increases intestinal motility and secretion
- VIP: relaxes sphincters and gut circular muscle, stimulates intestinal and pancreatic secretion
Diseases of the Upper GI
- Zollinger-Ellison syndrome: gastrin-producing tumors
- GERD: complication of Barrett's esophagus
- Barrett's esophagus: GI metaplasia of the lower esophagus that results from chronic GERD-induced esophagitis
- Achalasia: caused by degeneration of neurons in the esophageal wall → loss of inhibitory innervation in the LES### Gastrointestinal Diseases
• Clostridioides difficile (C. diff) Infection: + Presents with watery diarrhea (≥3 loose stools in 24 hrs), lower abdominal pain, fever + Toxin released by C. diff causes ribosylation of small GTPases, leading to disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release, and apoptosis + Labs: leukocytosis, hypoalbuminemia, and lactic acidosis (in severe cases) + Diagnosis: stool studies + Risk factors: recent antibiotic use (clindamycin most common), hospitalization, age > 65
Malabsorption Disorders
• Celiac Disease: + Immune-mediated disorder triggered by ingestion of gluten-containing foods (wheat, rye, or barley) + Gliadin peptides interact with HLA-DQ2 or HLA-DQ8 on antigen-presenting cells, stimulating CD4+ T cells to produce cytokines that exacerbate tissue damage + Almost all people with celiac disease carry the class II HLA-DQ2 or HLA-DQ8 allele + Presents with diarrhea, fatigue, weight loss, and malabsorption of nutrients
Intestinal Obstruction
• Intussusception: + Occurs when a segment of the intestine telescopes into the immediately distal segment + Most common cause of intestinal obstruction in children younger than 2 years old + Etiology: idiopathic, viral infection, and rotavirus vaccines + 1% of patients with cystic fibrosis develop intussusception
β-Lipoproteinemia
• Abetalipoproteinemia: + Rare autosomal recessive disease caused by mutation in microsomal triglyceride transfer protein (MTP) + Presents in infancy with failure to thrive, diarrhea, and steatorrhea + Triglyceride accumulation in epithelial cells leads to acanthocytosis (red cells with spiky membrane protrusions)
Inflammatory Bowel Disease (IBD)
• Crohn's Disease: + Chronic inflammatory condition characterized by transmural inflammation, which can affect any area of the gastrointestinal tract + May produce transmural inflammation, leading to complications such as bowel obstruction, fistulas, and malabsorption • Ulcerative Colitis: + Limited to the colon and rectum, involving only the mucosa and submucosa + High risk for colon cancer + Associated with primary sclerosing cholangitis and pyoderma gangrenosum
Irritable Bowel Syndrome (IBS)
• Chronic Functional Disorder: + Characterized by recurrent abdominal pain, changed bowel habits (diarrhea or constipation), and bloating + Pathophysiology involves altered gut motility, visceral hypersensitivity, and psychosocial factors
Pancreatitis
• Acute Pancreatitis: + Reversible inflammatory disorder that varies in severity, from focal edema to widespread hemorrhagic necrosis + Caused by autodigestion of the pancreas by intraacinar activation of pancreatic enzymes + Elevated serum lipase and amylase levels + Common causes: gallstones, chronic excessive alcohol use, and hypertriglyceridemia
Liver Diseases
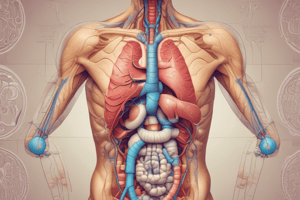
• Portal Triads: + Portal vein, hepatic artery, and bile duct + Blood from the portal vein and hepatic artery mixes in the sinusoids + Drains into the central vein, which forms the hepatic veins • Space of Disse: + Space between hepatocytes and endothelial cells + Contains interstitial fluid + Stellate (Ito) cells are located here and store vitamin A • Zone 1: + Region with the greatest delivery of oxygen and nutrients + Preferentially undertakes oxidative metabolism, ureagenesis, and bile acid production
...
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.