Questions and Answers
What is the primary function of keratocytes in the corneal stroma?
To maintain stromal collagen and ECM
Which of the following proteoglycans is more abundant in the posterior stroma?
Lumican
What is the approximate length of keratan sulfate in the cornea?
45nm
What is the primary function of Dermatan sulfate in the cornea?
Signup and view all the answers
What is the thickness of Descemet's membrane at birth?
Signup and view all the answers
What is the function of the anterior lamina of Descemet's membrane?
Signup and view all the answers
What is the shape of the majority of endothelial cells?
Signup and view all the answers
What is the minimum cell density required for normal endothelial function?
Signup and view all the answers
What is the primary function of the endothelial pump?
Signup and view all the answers
Why is the cornea clear?
Signup and view all the answers
What is the approximate horizontal diameter of the cornea?
Signup and view all the answers
Which of the following layers of the cornea is nonkeratinized?
Signup and view all the answers
What is the main function of the peripheral zone of the cornea?
Signup and view all the answers
What is the average radius of curvature of the posterior cornea?
Signup and view all the answers
How many layers of cells are present in the central corneal epithelium?
Signup and view all the answers
What is the thickness of the cornea in the periphery?
Signup and view all the answers
What is the transition zone between the cornea and the sclera/conjunctiva?
Signup and view all the answers
What is the function of the central optical zone of the cornea?
Signup and view all the answers
What is the approximate vertical diameter of the cornea?
Signup and view all the answers
What is the type of epithelial cells present in the cornea?
Signup and view all the answers
What is the primary function of microvilli and microplicae on the surface of corneal epithelial cells?
Signup and view all the answers
What is the average thickness of the corneal epithelium in terms of the number of cell layers?
Signup and view all the answers
What is the main function of tight, lateral, intercellular junctions and multiple gap junctions in wing cells?
Signup and view all the answers
What is the average time it takes for the complete turnover of the corneal epithelium?
Signup and view all the answers
What is the primary component of the basement membrane?
Signup and view all the answers
What is the thickness of the Bowman's layer?
Signup and view all the answers
What is the primary component of the corneal stroma?
Signup and view all the answers
What is the approximate number of lamellae in the corneal stroma?
Signup and view all the answers
What is the characteristic of the anterior 1/3 of the corneal stroma?
Signup and view all the answers
What is the role of the X, Y, Z hypothesis in corneal epithelial maintenance?
Signup and view all the answers
What is responsible for the majority of the refractive power in the globe?
Signup and view all the answers
Which of the following maintains corneal clarity?
Signup and view all the answers
How does the cornea receive its nutrient supply?
Signup and view all the answers
What is the main source of oxygen for the cornea?
Signup and view all the answers
What is the density of nerve terminals in the cornea?
Signup and view all the answers
What is the origin of the sensory nerves that supply the cornea?
Signup and view all the answers
What is the location of the nerve terminals in the cornea?
Signup and view all the answers
What is the result of the regular arrangement of collagen fibrils in the cornea?
Signup and view all the answers
What is the function of the endothelial fluid pump in the cornea?
Signup and view all the answers
How many layers does the cornea consist of?
Signup and view all the answers
What is the approximate diameter of the iris?
Signup and view all the answers
What is the function of the iris?
Signup and view all the answers
What is the thickest portion of the iris?
Signup and view all the answers
What is the function of the dilator muscle in the iris?
Signup and view all the answers
What is the approximate thickness of the iris at the iris root?
Signup and view all the answers
What is the shape of the pupil?
Signup and view all the answers
What happens to the pupil in low lighting conditions?
Signup and view all the answers
What is the junction between the iris and the ciliary body called?
Signup and view all the answers
What is the function of the sphincter muscle in the iris?
Signup and view all the answers
What is the approximate thickness of the peripheral ciliary zone?
Signup and view all the answers
What is the primary function of the iris in the eye?
Signup and view all the answers
What is the name of the heavily pigmented region at the pupil margin?
Signup and view all the answers
What is the function of the iris sphincter muscle?
Signup and view all the answers
What is the name of the single layer of lightly pigmented cells that forms the anterior epithelium of the iris?
Signup and view all the answers
What is the function of the iris dilator muscle?
Signup and view all the answers
What is the name of the layer of the iris that is highly vascularized?
Signup and view all the answers
What is the function of the melanocytes in the iris?
Signup and view all the answers
What is the name of the muscle that is stronger than the iris dilator muscle?
Signup and view all the answers
What is the characteristic of the pupil in bright conditions?
Signup and view all the answers
What is the relationship between the concentration of melanin in the iris and the iris color?
Signup and view all the answers
What is the primary function of melanocytes in the posterior iris surface?
Signup and view all the answers
What type of inheritance pattern is seen in iris pigmentation?
Signup and view all the answers
What is the characteristic of the vessels in the iris stroma?
Signup and view all the answers
What is the origin of the arterial supply to the iris?
Signup and view all the answers
What is the pattern of convergence of the radial vessels in the iris stroma?
Signup and view all the answers
What is the characteristic of the contraction folds in the periphery of the ciliary zone?
Signup and view all the answers
What is the function of the crypts in the anterior iris surface?
Signup and view all the answers
What is the relationship between melanin content and eye color?
Signup and view all the answers
What is the pathway of the pupillary light reflex?
Signup and view all the answers
What is the arrangement of the radial trabeculae in the anterior iris surface?
Signup and view all the answers
What is the anatomical structure that divides the anterior chamber from the posterior chamber and has a highly vascularized, muscular diaphragm with a central opening?
Signup and view all the answers
What is the term for the meeting point between the peripheral ciliary zone and the central pupillary zone of the iris?
Signup and view all the answers
What is the shape of the opening between the irises, which dilates in low lighting conditions and constricts in high lighting conditions?
Signup and view all the answers
What is the approximate diameter of the iris?
Signup and view all the answers
What is the junction between the iris and the ciliary body called?
Signup and view all the answers
What is the function of the pupillary ruff, and what is its histological composition?
Signup and view all the answers
Describe the structure and function of the anterior epithelium in the iris.
Signup and view all the answers
What is the difference in melanin concentration between the anterior and posterior epithelial layers of the iris?
Signup and view all the answers
Describe the structure and function of the iris sphincter muscle.
Signup and view all the answers
What is the relationship between the iris dilator muscle and the iris sphincter muscle?
Signup and view all the answers
What is the characteristic of the radial trabeculae seen in the anterior iris surface of light-colored irises?
Signup and view all the answers
What is the function of the melanocytes in the posterior iris surface?
Signup and view all the answers
How does the polygenic inheritance of iris pigmentation affect the amount of melanin in the iris?
Signup and view all the answers
What is the significance of the non-fenestrated vessels with tight junctions between endothelial cells in the iris vasculature?
Signup and view all the answers
What is the function of the two smooth muscles with opposing action in the iris?
Signup and view all the answers
What is the primary function of the ciliary muscle in accommodation?
Signup and view all the answers
What is the purpose of the ora serrata?
Signup and view all the answers
What is the main function of the pars plana?
Signup and view all the answers
What is the purpose of the supracilliaris in the ciliary body?
Signup and view all the answers
What is the function of the longitudinal/meridional muscle in the ciliary body?
Signup and view all the answers
What is the main function of the radial muscle in the ciliary body?
Signup and view all the answers
What is the purpose of the circular/Muller's muscle in the ciliary body?
Signup and view all the answers
What is the primary function of the zonules in the eye?
Signup and view all the answers
What is the main function of the pars plicata in the ciliary body?
Signup and view all the answers
What is the function of the dentate process in the ciliary body?
Signup and view all the answers
What is the primary function of the ciliary muscle?
Signup and view all the answers
What type of receptors dominate the ciliary muscle?
Signup and view all the answers
What is the primary mechanism of aqueous humor production?
Signup and view all the answers
What is the function of the non-pigmented epithelial cells in the ciliary epithelium?
Signup and view all the answers
What is the direction of NaCl transport in the ciliary epithelium?
Signup and view all the answers
What is the function of gap junctions in the ciliary epithelium?
Signup and view all the answers
What is the purpose of the fenestrated capillaries in the ciliary stroma?
Signup and view all the answers
What is the site of aqueous humor production?
Signup and view all the answers
What is the purpose of the Na+/K+ ATPase in the ciliary epithelium?
Signup and view all the answers
What is the purpose of the Cl- channels in the ciliary epithelium?
Signup and view all the answers
What is the purpose of the trabecular meshwork?
Signup and view all the answers
What is the location of Schwalbe's line?
Signup and view all the answers
What is the function of the endothelial cells in the trabecular meshwork?
Signup and view all the answers
What is the purpose of the ciliary sulcus?
Signup and view all the answers
What is the function of the scleral spur?
Signup and view all the answers
What is the purpose of the juxtacanalicular meshwork?
Signup and view all the answers
What is the function of the trabecular cells?
Signup and view all the answers
What is the location of the Schlemm's canal?
Signup and view all the answers
What is the function of the inner wall of Schlemm's canal?
Signup and view all the answers
What is the function of the endothelial cells in Schlemm's canal?
Signup and view all the answers
What is the percentage of aqueous drainage through the uveoscleral route?
Signup and view all the answers
Which of the following is NOT a part of the trabecular meshwork outflow route?
Signup and view all the answers
What is the effect of ciliary muscle contraction on trabecular outflow?
Signup and view all the answers
What is the route of aqueous drainage from the collector channel to the episcleral plexus?
Signup and view all the answers
What is the effect of ciliary muscle relaxation on uveoscleral outflow?
Signup and view all the answers
What is the final destination of aqueous humour drained through the vortex system?
Signup and view all the answers
What is the route of aqueous humour drainage through the uveoscleral pathway?
Signup and view all the answers
What is the effect of accommodation on uveoscleral outflow?
Signup and view all the answers
What is the proportion of aqueous humour drainage through the trabecular meshwork outflow route?
Signup and view all the answers
What is the role of the ciliary muscle in regulating aqueous humour outflow?
Signup and view all the answers
What is the location of Schwalbe’s Line?
Signup and view all the answers
What is the function of trabecular cells?
Signup and view all the answers
What is the function of the scleral spur?
Signup and view all the answers
What is the region of the trabecular meshwork closest to the anterior chamber?
Signup and view all the answers
What is the main source of resistance to aqueous flow?
Signup and view all the answers
What is the function of the endothelial cells in Schlemm's canal?
Signup and view all the answers
What is the region of the iris where it inserts into the ciliary body?
Signup and view all the answers
What percentage of drainage occurs through the uveoscleral route?
Signup and view all the answers
What is the effect of a contracted ciliary muscle on trabecular outflow?
Signup and view all the answers
What is the destination of aqueous humour that drains through the uveoscleral route?
Signup and view all the answers
What is the effect of a relaxed ciliary muscle on uveoscleral outflow?
Signup and view all the answers
What is the route of aqueous humour drainage that involves the episcleral plexus?
Signup and view all the answers
What is the relationship between the ciliary muscle and trabecular outflow?
Signup and view all the answers
What is the percentage of aqueous humour drainage that occurs through the trabecular route?
Signup and view all the answers
What is the destination of aqueous humour that drains through the trabecular route?
Signup and view all the answers
What is the approximate composition of the crystalline lens in terms of water and protein?
Signup and view all the answers
What is the significance of the equator in the anatomy of the crystalline lens?
Signup and view all the answers
What is the sequence of events during the 4th to 8th week of gestation in the development of the crystalline lens?
Signup and view all the answers
What is the significance of the lens bow in the development of the crystalline lens?
Signup and view all the answers
What is the importance of the lens capsule in the anatomy of the crystalline lens?
Signup and view all the answers
What is the reason why the lens is transparent despite the presence of protein that would normally scatter light?
Signup and view all the answers
What is the role of α-crystallin in the lens?
Signup and view all the answers
What is the role of the 'pump-leak' mechanism in the lens?
Signup and view all the answers
What is the characteristic of β-crystallin in the lens?
Signup and view all the answers
What is the approximate percentage of α-crystallin in the lens?
Signup and view all the answers
What is the refractive power of the lens in diopters, and how does the refractive index of the lens vary from the anterior pole to the posterior pole?
Signup and view all the answers
Describe the structure and function of the lens epithelium, including its regional variations and the role of gap junctions in maintaining lens transparency.
Signup and view all the answers
What is the structure and function of the lens fibers, including their formation, growth, and organization, and how do they contribute to the lens's refractive power?
Signup and view all the answers
Describe the structure and function of the lens zonules, including their composition, origin, and role in maintaining lens position and facilitating accommodation.
Signup and view all the answers
What is the 'pump-leak' system of lens hydration, and how does it maintain the lens's transparency and refractive index?
Signup and view all the answers
What is the percentage of water in the crystalline lens?
Signup and view all the answers
What is the name of the centre of the anterior lens surface?
Signup and view all the answers
During which week of gestation does the optic pit deepen to form the optic vesicle?
Signup and view all the answers
What is the function of the zonules?
Signup and view all the answers
During which week of gestation does the posterior cells begin to elongate anteriorly?
Signup and view all the answers
What is the name of the layer that surrounds the lens vesicle?
Signup and view all the answers
What is the name of the area midway between the two poles of the lens?
Signup and view all the answers
During which week of gestation does the primary lens fibres fill the lens vesicle?
Signup and view all the answers
What is the function of the crystalline lens?
Signup and view all the answers
What is the characteristic of the lens cells?
Signup and view all the answers
What is the approximate refractive power of the lens?
Signup and view all the answers
What is the shape of lens fibers in cross-section?
Signup and view all the answers
What is the function of the lens epithelium?
Signup and view all the answers
What is the main component of the lens?
Signup and view all the answers
What is the function of the lens zonules?
Signup and view all the answers
What is the shape of the lens suture at the anterior pole?
Signup and view all the answers
What is the function of the 'pump-leak' system in the lens?
Signup and view all the answers
What is the approximate thickness of the lens at birth?
Signup and view all the answers
What is the shape of the lens fibers?
Signup and view all the answers
What is the function of the lens capsule?
Signup and view all the answers
What is the main reason for the transparency of the lens?
Signup and view all the answers
What is the function of αA-crystallin in the lens?
Signup and view all the answers
What is the most abundant crystallin protein in the lens?
Signup and view all the answers
What is the function of the 'pump-leak' mechanism in the lens?
Signup and view all the answers
What is the function of αB-crystallin in the lens?
Signup and view all the answers
What is the least abundant crystallin protein in the lens?
Signup and view all the answers
What is the function of crystallin proteins in the lens?
Signup and view all the answers
What is the function of the lens epithelial cells?
Signup and view all the answers
What is the function of the surrounding capsule of the lens?
Signup and view all the answers
What is the characteristic of the lens that allows it to be transparent?
Signup and view all the answers
What is the role of the ciliary muscle in accommodation, and how does it affect the zonules and the lens?
Signup and view all the answers
How does the lens capsule influence the shape of the lens during accommodation?
Signup and view all the answers
Describe the changes in the lens shape and displacement during accommodation.
Signup and view all the answers
What is the significance of the zonules in accommodation, and how do they relate to the ciliary muscle?
Signup and view all the answers
What is the current understanding of the mechanism of accommodation, and what are the ongoing debates in this area?
Signup and view all the answers
What is the primary pathway involved in the neural control of accommodation, and what are the two signals sent from the Edinger-Westphal nucleus?
Signup and view all the answers
What are the main contributors to the development of presbyopia, and how do they affect the accommodative apparatus?
Signup and view all the answers
What is the role of sympathetic nerve activity in the neural control of accommodation, and where do these fibers originate and synapse?
Signup and view all the answers
What are the anatomical components that make up the accommodative apparatus, and how do they work together to facilitate accommodation?
Signup and view all the answers
What is the sequence of events involved in the accommodation reflex, and what are the resulting effects on the pupil and medial rectus?
Signup and view all the answers
What is the main driver of presbyopia?
Signup and view all the answers
What is the role of the Edinger Westphal nucleus in accommodation?
Signup and view all the answers
What type of mediated contraction occurs in the ciliary muscle?
Signup and view all the answers
What is the origin of the sympathetic nerve activity that affects the ciliary muscle?
Signup and view all the answers
What is the result of the accommodation reflex?
Signup and view all the answers
What is the anatomical basis underpinning accommodation?
Signup and view all the answers
What is the function of the parasympathetic nerves in the ciliary muscle?
Signup and view all the answers
Where do the post-ganglionic fibres from the superior cervical ganglion travel to?
Signup and view all the answers
What is the approximate age of onset for presbyopia?
Signup and view all the answers
What is the name of the nucleus that receives the blur signal from the primary visual cortex?
Signup and view all the answers
What is the primary function of the ciliary muscle in the accommodation process?
Signup and view all the answers
What is the result of the contraction of the outer longitudinal fibers of the ciliary muscle during accommodation?
Signup and view all the answers
What is the primary function of the zonules in the accommodation process?
Signup and view all the answers
What is the result of the forward displacement of the lens during accommodation?
Signup and view all the answers
What is the role of the lens capsule in the accommodation process?
Signup and view all the answers
What is the result of decapsulation of the lens?
Signup and view all the answers
What is the primary function of the lens capsule in young eyes?
Signup and view all the answers
What is the result of the increase in nucleus thickness during accommodation?
Signup and view all the answers
What is the result of the posterior pole of the lens remaining unchanged during accommodation?
Signup and view all the answers
What is the arrangement of the ciliary muscle fibers?
Signup and view all the answers
The vitreous humor is composed of 99% water and 1% structural proteins.
Signup and view all the answers
The posterior hyaloid membrane is a typical membrane that separates the vitreous from the retina.
Signup and view all the answers
The vitreous base is the strongest site of attachment to the retina.
Signup and view all the answers
Hyalocytes are responsible for producing collagen in the vitreous.
Signup and view all the answers
The refractive index of the vitreous is approximately 1.337.
Signup and view all the answers
Vitamin C promotes intraocular wound healing via its antioxidant properties.
Signup and view all the answers
The vitreous humor functions as a blood-ocular barrier, preventing the movement of macromolecules and cells between the anterior and posterior segments.
Signup and view all the answers
Liquefaction of the vitreous humor starts from the peripheral region.
Signup and view all the answers
The collagen fibril network in the vitreous humor becomes more compact with age.
Signup and view all the answers
Hyaluronic acid maintains the vitreous humor's gel consistency, collagen fibril spacing, and optical clarity.
Signup and view all the answers
What is the approximate percentage of water in the vitreous?
Signup and view all the answers
Which of the following is NOT a function of the vitreous?
Signup and view all the answers
What is the main component of the vitreous collagen fibril network?
Signup and view all the answers
What is the approximate thickness of the cortex in the vitreous?
Signup and view all the answers
What is the purpose of the patellar fossa?
Signup and view all the answers
What is the approximate percentage of structural proteins in the vitreous?
Signup and view all the answers
What is the primary function of hyaluronic acid in the vitreous?
Signup and view all the answers
What is the location of the highest hyalocyte density in the vitreous?
Signup and view all the answers
What is the primary function of type IX collagen in the vitreous?
Signup and view all the answers
What is responsible for the vitreous being firmer than egg white?
Signup and view all the answers
What is the primary function of vitamin C in the vitreous?
Signup and view all the answers
What is the primary component of the vitreous humor?
Signup and view all the answers
What is the result of the aging changes in the vitreous humor?
Signup and view all the answers
What is the function of the blood-ocular barrier in the vitreous?
Signup and view all the answers
What is the result of the collagen fibril network becoming free-floating bundles?
Signup and view all the answers
What is the primary function of hyaluronic acid in the vitreous?
Signup and view all the answers
What is the primary component responsible for the mechanical strength of the vitreous?
Signup and view all the answers
What is the result of the vitreous maintaining optical clarity?
Signup and view all the answers
What is the primary function of the vitreous humor?
Signup and view all the answers
What is the result of the change in hyaluronic acid conformation with aging?
Signup and view all the answers
What is the primary function of Müller cells in the retina?
Signup and view all the answers
What is the significance of the blood-retina barrier in the retina?
Signup and view all the answers
What is the function of the retinal pigment epithelium (RPE) in the retina?
Signup and view all the answers
What is the role of astrocytes in the retina?
Signup and view all the answers
What is the significance of the tight junctions between the retinal pigment epithelium and the photoreceptors?
Signup and view all the answers
What is the function of the optic fiber in the retina?
Signup and view all the answers
What is the significance of the basolateral membrane of the retinal pigment epithelium?
Signup and view all the answers
What is the role of the retinal pigment epithelium in the recycling of photopigments?
Signup and view all the answers
What is the significance of the peak distribution of astrocytes on the optic nerve head?
Signup and view all the answers
What is the function of the Müller cells in maintaining the ionic balance of the retina?
Signup and view all the answers
What is the approximate diameter of the central retina?
Signup and view all the answers
Which layer of the retina is the outermost layer?
Signup and view all the answers
What is the function of macular pigment?
Signup and view all the answers
What is the center of the fovea?
Signup and view all the answers
Which layer of the retina is thicker in the central retina than in the peripheral retina?
Signup and view all the answers
What is the total diameter of the retina?
Signup and view all the answers
What is the shape of the optic nerve head?
Signup and view all the answers
What is the region of the retina that stretches to the ora serrata?
Signup and view all the answers
What is the diameter of the macula?
Signup and view all the answers
What is the region of the retina that has no rod photoreceptors?
Signup and view all the answers
What is the primary function of the Outer Nuclear Layer (ONL) in the retina?
Signup and view all the answers
What is the primary pathway of visual information transmission in the retina?
Signup and view all the answers
What is the type of glial cell that functions as a macrophage in response to retinal trauma?
Signup and view all the answers
What is the approximate convergence ratio of rods to ganglion cells in the retina?
Signup and view all the answers
What is the location of the optic cup in the retina?
Signup and view all the answers
What is the function of the Inner Plexiform Layer (IPL) in the retina?
Signup and view all the answers
What is the primary function of the Retinal Pigment Epithelium (RPE) in the retina?
Signup and view all the answers
What is the type of synapse formed between photoreceptors and bipolar cells in the retina?
Signup and view all the answers
What is the approximate number of photoreceptors that converge onto one ganglion cell in the fovea?
Signup and view all the answers
What is the layer of the retina where the ganglion cell axons travel towards the optic disc?
Signup and view all the answers
What is the primary function of Müller cells in the retina?
Signup and view all the answers
Where are the cell bodies and processes of astrocytes typically found in the retina?
Signup and view all the answers
What is the primary function of the retinal pigment epithelium (RPE)?
Signup and view all the answers
What is the function of the tight junctions between the retinal pigment epithelium (RPE) and the choriocapillaris?
Signup and view all the answers
What is the location of the basolateral membrane of the retinal pigment epithelium (RPE)?
Signup and view all the answers
What is the function of the astrocytes in the retina?
Signup and view all the answers
What is the function of the Müller cells in terms of photopigment recycling?
Signup and view all the answers
What is the approximate location of the astrocytes in the retina?
Signup and view all the answers
What is the function of the retinal pigment epithelium (RPE) in terms of the blood-retina barrier?
Signup and view all the answers
What is the structure that separates the retinal pigment epithelium (RPE) from the choroid?
Signup and view all the answers
What is the primary function of Müller cells in the retina?
Signup and view all the answers
Which of the following is a characteristic of astrocytes in the retina?
Signup and view all the answers
What is the function of the retinal pigment epithelium (RPE) in relation to the choriocapillaris?
Signup and view all the answers
Which of the following is NOT a function of Müller cells?
Signup and view all the answers
What is the location of the basolateral membrane of the retinal pigment epithelium (RPE)?
Signup and view all the answers
Which of the following glial cells is responsible for maintaining the blood-retina barrier in the inner retina?
Signup and view all the answers
What is the function of the tight junctions between the retinal pigment epithelium (RPE) and the choriocapillaris?
Signup and view all the answers
Which of the following is a characteristic of the retinal pigment epithelium (RPE)?
Signup and view all the answers
What is the function of the optic fiber in the retina?
Signup and view all the answers
Which of the following is a function of the Müller cells in relation to photopigments?
Signup and view all the answers
What is the function of the lamina cribrosa in the optic nerve head?
Signup and view all the answers
What is the main function of oligodendrocytes in the optic nerve?
Signup and view all the answers
What are the fine fibrous septa in the optic nerve responsible for?
Signup and view all the answers
What is the function of the circle of Zinn-Haller in the optic nerve?
Signup and view all the answers
Why is the blood-retina barrier crucial for the retina?
Signup and view all the answers
What is the primary function of the pia mater in the optic nerve?
Signup and view all the answers
How does the optic nerve increase in thickness posteriorly?
Signup and view all the answers
What is the role of astrocytes in the optic nerve?
Signup and view all the answers
What is the main function of the optic nerve?
Signup and view all the answers
What are the four layers of the optic nerve?
Signup and view all the answers
What is the shape of the optic disc?
Signup and view all the answers
What is the range of the area of the optic disc?
Signup and view all the answers
What is the thickness of the RNFL that feeds into the optic nerve?
Signup and view all the answers
What is the location of the ganglion cell axons?
Signup and view all the answers
What is the normal vertical cup to disc ratio?
Signup and view all the answers
What is the range of the horizontal diameter of the optic disc?
Signup and view all the answers
What is the innermost layer of the retina?
Signup and view all the answers
What is the outermost layer of the retina?
Signup and view all the answers
What is the section of the optic nerve that is within the eye?
Signup and view all the answers
What is the thickest portion of the neural retinal rim?
Signup and view all the answers
What is the function of astrocytes in the optic nerve head?
Signup and view all the answers
What is the structure that separates the inner surface of the optic nerve head from the vitreous?
Signup and view all the answers
What is the approximate number of retinal ganglion cells per optic nerve?
Signup and view all the answers
What is the region of the optic nerve head where the nerve fibres become increasingly myelinated?
Signup and view all the answers
What is the purpose of the astrocytes in the glial lamina cribrosa?
Signup and view all the answers
What is the term for the pattern of nerve fibres in the superficial nerve fibre layer?
Signup and view all the answers
What is the structure that is formed by the convergence of nerve fibres towards the disc?
Signup and view all the answers
What is the term for the region of the optic nerve head where the astrocytes increase in number posteriorly?
Signup and view all the answers
What is the purpose of the limiting membrane of Elschnig?
Signup and view all the answers
What is the term for the astrocytes that line the periphery of the optic nerve?
Signup and view all the answers
What is the primary function of the lamina cribrosa?
Signup and view all the answers
What is the location of the circle of Zinn-Haller?
Signup and view all the answers
What is the function of the pial septa in the optic nerve?
Signup and view all the answers
What is the main function of the blood-retina barrier?
Signup and view all the answers
What is the main function of the myelination of nerve axons in the retrolaminar region?
Signup and view all the answers
What is the function of the meningeal sheath in the optic nerve?
Signup and view all the answers
What is the main function of the astrocytes in the optic nerve?
Signup and view all the answers
What is the primary function of the optic nerve?
Signup and view all the answers
How many layers does the optic nerve consist of?
Signup and view all the answers
What is the main blood supply to the optic disc surface?
Signup and view all the answers
What is the primary function of the choroid in the eye?
Signup and view all the answers
What is the typical thickness of the choroid at birth, and how does it change with age?
Signup and view all the answers
What are the two main histologically defined layers of the choroid, and what are their characteristic features?
Signup and view all the answers
What is the role of Bruch's membrane in the eye, and what changes occur in it with aging?
Signup and view all the answers
What is the approximate thickness of the choriocapillaris, and how does it vary across the retina?
Signup and view all the answers
What is the suprachoroid, and what is its significance in pharmacological targeting of the choroid?
Signup and view all the answers
What is the role of indocyanine green angiography (ICG) in clinical assessment of the choroid?
Signup and view all the answers
What is the role of optical coherence tomography angiography (OCTa) in clinical assessment of the choroid?
Signup and view all the answers
What is the significance of the choroid in Vogt-Koyanagi-Harada's disease and age-related macular degeneration (AMD)?
Signup and view all the answers
What is the approximate percentage of aqueous humour drainage that occurs via the uveoscleral pathway?
Signup and view all the answers
What is the primary function of the choroid in the eye?
Signup and view all the answers
What is the approximate thickness of the choroid at birth?
Signup and view all the answers
What is the function of Bruch's membrane?
Signup and view all the answers
What is the thickness of the choriocapillaris?
Signup and view all the answers
What is the layer of the choroid that contains medium to small sized vessels?
Signup and view all the answers
What is the purpose of indocyanine green (ICG) angiography in clinical assessment of the choroid?
Signup and view all the answers
What is the percentage of aqueous humour drainage that occurs via the uveoscleral pathway?
Signup and view all the answers
What is the disease that is characterized by choroidal granulomas?
Signup and view all the answers
What is the layer of the choroid that is of pharmacological interest as a drug delivery target?
Signup and view all the answers
What is the technique used to produce enface imaging of the retina and choroid vessels?
Signup and view all the answers
What is the mechanism by which the signalling protein TGF-β2 'disarms' inflammatory cells that cross from the blood stream into the eye?
Signup and view all the answers
What is the significance of the 'stitched' together vessel endothelial cells in the iris, as observed under electron microscopy?
Signup and view all the answers
What is the consequence of the breakdown of tight junctions in the blood ocular barrier during inflammation?
Signup and view all the answers
What is the primary purpose of inflammation in the body, and how does it achieve this purpose?
Signup and view all the answers
What is the function of the choroidal vessels in the retina, and how do they differ from retinal vessels?
Signup and view all the answers
What are the clinical signs of acute inflammation, and how do they impact the body?
Signup and view all the answers
What is the role of the retinal pigment epithelium (RPE) in maintaining the blood ocular barrier in the retina?
Signup and view all the answers
What is ocular immune privilege, and how does it relate to inflammation in the eye?
Signup and view all the answers
What are the key differences between anterior chamber reaction and chorioretinal inflammation in the eye?
Signup and view all the answers
How does inflammation in the eye impact the blood-ocular barrier, and what are the consequences of this impact?
Signup and view all the answers
What is the primary purpose of inflammation in the body?
Signup and view all the answers
Which of the following is a characteristic of chronic inflammation?
Signup and view all the answers
What is the purpose of the ocular immune privilege?
Signup and view all the answers
What is the site of blood-ocular barrier?
Signup and view all the answers
What is the result of uncontrolled inflammation in the eye?
Signup and view all the answers
What is the purpose of anti-inflammatory drugs?
Signup and view all the answers
What is the clinical sign of inflammation characterized by redness?
Signup and view all the answers
What is the type of cells involved in anterior chamber reaction?
Signup and view all the answers
What is the site of inflammation in ocular surface allergy?
Signup and view all the answers
What is the protein involved in anterior chamber reaction?
Signup and view all the answers
What is the primary function of ocular immune privilege?
Signup and view all the answers
What is the main source of TGF-β2 in the eye?
Signup and view all the answers
What is the function of tight junctions in the blood-ocular barrier?
Signup and view all the answers
What happens to the blood-aqueous barrier during inflammation?
Signup and view all the answers
What is the function of the blood-retina barrier?
Signup and view all the answers
What is the function of the RPE in the blood-ocular barrier?
Signup and view all the answers
Where are fenestrated blood vessels found in the eye?
Signup and view all the answers
What is the result of the breakdown of the blood-aqueous barrier?
Signup and view all the answers
What is the function of the choroid?
Signup and view all the answers
What is the result of the breakdown of the blood-retina barrier?
Signup and view all the answers
Study Notes
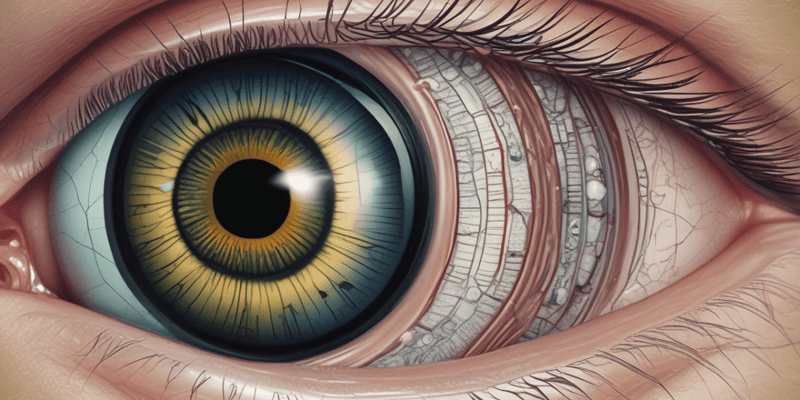
Anatomy of the Cornea
- The cornea is the anterior 1/6 of the globe, consisting of 5 layers: epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium.
- The cornea merges with the sclera and conjunctiva in a transitional region called the limbus.
- Dimensions:
- Anteriorly: oval appearance, 11.7mm horizontally and 10.6mm vertically.
- Posteriorly: circular, 11.7mm in diameter.
- Thinnest centrally: 550 μm, increasing to 700 μm in the periphery.
- Radius of curvature: 7.7mm anteriorly and 6.9mm posteriorly.
Optical Zones
- Only the central optical zone (central 3-4mm) is responsible for image formation.
- The remainder of the cornea is for mechanical support and peripheral vision with a dilated pupil.
- Central zone: mostly spherical.
- Paracentral zone: generally spherical, but flatter than the central zone.
- Peripheral zone: flattens significantly.
- Limbal zone: transitions into the sclera and conjunctiva.
Corneal Epithelium
- Thickness: 50-60 μm.
- Composed of 5 layers of cells centrally.
- Non-keratinized, stratified squamous epithelial cells.
- Cell layers:
- Superficial cells: 2-3 layers thick, attached to each other by desmosomes.
- Wing cells: 2-3 layers, named for their wing-shaped processes, with tight, lateral, intercellular junctions and multiple gap junctions.
- Basal cells: single layer of tall columnar cells, adherent to the basement membrane.
- Turnover: complete every 10 days, with the X, Y, Z hypothesis of corneal epithelial maintenance.
Basement Membrane
- Thickness: 40-100 nm.
- Composed of type IV collagen, laminin, heparin sulfate proteoglycans (HSPGs), and nidogens.
- Aids in binding of the epithelium to the underlying Bowman's layer.
Bowman's Layer
- Thickness: 12 μm.
- Acellular collagen fibril matrix, mainly composed of type I collagen.
- Collagen is finer and more randomly arranged than in the stroma.
Corneal Stroma
- Thickness: 90% of the corneal thickness.
- Composed of water, collagen arranged into lamellae, keratocytes, proteoglycans, and GAGs.
- Mainly type I collagen, with small amounts of type III, V, and VI.
- Lamellae: 200-300, with all fibrils in the same lamellae running in the same direction.
- Anterior 1/3: lamellae are narrow, branching, and interweaving.
- Posterior 2/3: lamellae are wider and more regular.
Stromal Cells
- Keratocytes (corneal fibroblasts): flattened cells that lie between the lamellae.
- Maintain stromal collagen and ECM.
- Large nuclei with minimal cytoplasm, communicate with each other via numerous long processes and gap junctions.
Descemet's Membrane
- Thickness: 5 μm at birth, increasing to 15 μm over a lifetime.
- Composed of type IV collagen.
- Divided into two laminae: anterior (banded, 3 μm thick) and posterior (non-banded, homogenous).
- Terminates abruptly at the limbus as a thickened area of collagen called Schwalbe's line.
Corneal Endothelium
- Innermost corneal layer, adjacent to the aqueous humour and anterior chamber.
- Continuous with the cells lining the trabecular meshwork and the anterior iris.
- Single layer of flattened polygonal cells.
- 70-80% of cells are hexagonal in shape.
- Around 20 μm in diameter and 4-6 μm thick.
- Gap junctions provide communication between cells.
Why is the Cornea Clear?
- Corneal clarity is maintained by:
- Regular collagen size, spacing, and lattice pattern.
- Lattice fibril arrangement, allowing light to pass through without disruption.
- Even keratocyte spacing.
- Endothelial fluid pump.
Nutrient Supply to the Cornea
- The cornea is avascular, receiving nutrients by diffusion from the aqueous humour and limbal vessels.
- Limbal vessels are supplied by anterior ciliary arteries.
- Oxygen is mainly obtained from atmospheric oxygen dissolved in the tear film.
- With eyes closed, palpebral capillaries supply the bulk of oxygen.
Corneal Nerves
- The cornea is the most richly innervated body tissue, with approximately 160,000 nerve terminals/mm2.
- Sensory nerves are supplied by long ciliary nerves (ophthalmic branch of CN V).
- Form a unmyelinated plexus, whose branches are mostly within the middle 1/3 of the stroma to Bowman's layer.
- Can become desensitized over time (e.g., contact lens wear).
Anatomy of the Iris
- The iris is the most anterior component of the uvea, dividing the anterior chamber from the posterior chamber.
- It is a highly vascularized, muscular diaphragm with a central opening (pupil), approximately 12 mm in diameter.
- The iris has two zones: the peripheral ciliary zone (3-4 mm) containing the dilator muscle, and the central pupillary zone (1-2 mm) containing the sphincter muscle.
Iris Structure
- The iris has three layers: the anterior border layer, stroma, and pigmented epithelial layer (anterior and posterior).
- The anterior border layer consists of a modified stroma with melanocytes, collagen, and fibroblasts, determining iris color.
- The stroma is a loose collagenous matrix with fibroblasts, melanocytes, and a high degree of vascularization.
Iris Muscles
- There are two muscles in the iris: the sphincter and dilator muscles, which have opposing actions to govern pupil size.
- The sphincter muscle is a flat annulus of smooth muscle at the pupil margin, approximately 0.75-1 mm wide.
- The dilator muscle is composed of radially oriented basal processes of anterior epithelial cells, extending into the stroma.
Pupil
- The pupil is a circular opening between the irises, approximately 3-4 mm in diameter.
- Pupil size is regulated by the opposing actions of the sphincter and dilator muscles, responding to light stimuli.
- Pupil size affects retinal illuminance, depth of focus, and aberrations.
Iris Function
- The iris controls pupil size, modulating retinal illuminance and minimizing aberrations.
- It blocks stray light and plays a role in social signaling, constricting when asleep and dilating when excited.
Iris Histology
- The anterior epithelium is a single layer of lightly pigmented cells divided into apical and basal processes.
- The posterior epithelium is a single layer of heavily pigmented epithelial cells, with a concentration of melanin similar between individuals, regardless of iris color.
Anatomy of the Iris
- The iris is the most anterior component of the uvea, dividing the anterior chamber from the posterior chamber.
- It is a highly vascularized, muscular diaphragm with a central opening (pupil), approximately 12 mm in diameter.
- The iris has two zones: the peripheral ciliary zone (3-4 mm) containing the dilator muscle, and the central pupillary zone (1-2 mm) containing the sphincter muscle.
Iris Structure
- The iris has three layers: the anterior border layer, stroma, and pigmented epithelial layer (anterior and posterior).
- The anterior border layer consists of a modified stroma with melanocytes, collagen, and fibroblasts, determining iris color.
- The stroma is a loose collagenous matrix with fibroblasts, melanocytes, and a high degree of vascularization.
Iris Muscles
- There are two muscles in the iris: the sphincter and dilator muscles, which have opposing actions to govern pupil size.
- The sphincter muscle is a flat annulus of smooth muscle at the pupil margin, approximately 0.75-1 mm wide.
- The dilator muscle is composed of radially oriented basal processes of anterior epithelial cells, extending into the stroma.
Pupil
- The pupil is a circular opening between the irises, approximately 3-4 mm in diameter.
- Pupil size is regulated by the opposing actions of the sphincter and dilator muscles, responding to light stimuli.
- Pupil size affects retinal illuminance, depth of focus, and aberrations.
Iris Function
- The iris controls pupil size, modulating retinal illuminance and minimizing aberrations.
- It blocks stray light and plays a role in social signaling, constricting when asleep and dilating when excited.
Iris Histology
- The anterior epithelium is a single layer of lightly pigmented cells divided into apical and basal processes.
- The posterior epithelium is a single layer of heavily pigmented epithelial cells, with a concentration of melanin similar between individuals, regardless of iris color.
Ciliary Body Anatomy
- The ciliary body is part of the uvea, located at the corneoscleral junction and attached to the iris.
- It consists of 5 layers: supracillaris, ciliary muscle, ciliary stroma, pigmented epithelium, and non-pigmented epithelium.
- The ciliary body is divided into two parts: pars plicata and pars plana.
Pars Plicata
- The anterior ciliary body, containing around 70 ciliary processes.
- Each ciliary process is approximately 2 mm long, 0.5 mm wide, and 1 mm deep.
- Pars plicata is responsible for producing aqueous humor.
Pars Plana
- The posterior ciliary body, extending from the pars plicata to the ora serrata.
- The retinal extension into the pars plana is called the dentate process.
- Ora serrata is the serrated junction between the retina and the ciliary body, located approximately 5 mm anterior to the equator.
Ciliary Body - Supraciliaris
- The junction between the ciliary body and the sclera, composed of ribbons of connective tissue.
- It also contains fibroblasts and melanocytes, allowing the ciliary muscle to contract without detaching from the sclera.
Ciliary Body - Ciliary Muscle
- The ciliary muscle has three muscle groups: longitudinal/meridional/Brucke's muscle, radial, and circular/Muller's muscle.
- The longitudinal muscle is closest to the sclera, attaching to the scleral spur.
- The radial muscle is located in the middle, and the circular muscle is closest to the lens, functioning as a sphincter.
- In accommodation, the parasympathetic innervation is dominant over the sympathetic innervation.
- The ciliary muscles move anterior to the lens, reducing zonular fiber contraction, and the lens bulges to accommodate.
Accommodation
- The lens zonules (or zonule of Zinn) connect the ciliary body to the lens, originating from the pars plana.
- The neural control of accommodation involves a blur signal sent to the primary visual cortex, then to the pretectal area, and finally to the Edinger Westphal nucleus.
- Two signals are then sent: one via the parasympathetic pathway to the ciliary ganglion and the ciliary muscle, and the other via CNIII to the medial rectus.
- The accommodation/near reflex involves accommodation, pupil constriction, and convergence.
Ciliary Stroma
- The ciliary stroma lies over the ciliary muscle, being heavily pigmented, vascularized, and innervated.
- It is continuous with the choroid posteriorly and the iris anteriorly.
- The ciliary beds within the stroma are fenestrated, allowing exchange between the blood and the stroma.
Ciliary Epithelium
- The ciliary epithelium is the site of aqueous production and facilitates immune privilege of the eye.
- There are two types of ciliary epithelium: pigmented (inner, cuboidal) and non-pigmented (outer, columnar/cuboidal).
- The non-pigmented cells contain tight junctions (zonula occludens) to prevent leakage and maintain the ocular blood-aqueous barrier.
Aqueous Production
- The production rate of aqueous humor is approximately 2.5 µL/min, with a turnover of around 2.4 µL/min.
- Aqueous humor is produced through a combination of active secretion (80-90%) and passive diffusion (10-20%).
- There are three mechanisms of aqueous production: passive diffusion, passive ultrafiltration, and active secretion.
Aqueous Production Mechanisms
- Passive diffusion: transportation of substances down their concentration gradient across the lipid portion of the membrane.
- Passive ultrafiltration: flow of water and water-soluble substances through fenestrated capillaries, driven by osmotic gradient or hydrostatic pressure.
- Active secretion: energy-dependent transport of selected substances against a concentration gradient through specific transporters.
Aqueous Production Steps
- Step 1: NaCl is transferred from the stroma by two sets of electroneutral transporters.
- Step 2: Passage of NaCl from the pigmented epithelium to the non-pigmented epithelium through gap junctions.
- Step 3: Secondary active transport of Cl- and HCO3-, and primary active transport of Na+ and K+.
Aqueous Drainage
- Aqueous humor is drained through two sites: the posterior trabecular meshwork into Schlemm's canal, and the uveoscleral route (~10% outflow).
- Intraocular pressure (IOP) is determined by the balance between aqueous production and clearance.
Anterior Chamber Angle
- Forms the junction between the cornea and iris
- Responsible for the drainage of aqueous humour
Trabecular Meshwork
- Located between Schwalbe's Line and the scleral spur
- Consists of three regions: uveal, corneoscleral, and juxtacanalicular/cribriform meshwork
- Uveal meshwork: closest to the anterior chamber, collagen and elastic lamellae network, and large openings between lamellae
- Corneoscleral meshwork: middle layer, perforated collagen and elastin plates covered by TM cells, and connects the scleral spur to the anterior wall of the scleral sulcus
- Juxtacanalicular/cribriform meshwork: loose connective tissue, sieve-like plates, and main source of resistance to aqueous flow
Trabecular Cells
- Endothelial: maintain passageway patency, neutralize reactive oxygen species
- Macrophage: biological filter/phagocytosis, immune mediation
- Fibroblastic: ECM turnover/tissue repair
- Smooth muscle: contractile tone, mechanotrasduction
Schlemm's Canal
- Outer wall: closest to sclera, monolayer of endothelial cells, well-developed basement membrane, and no transcellular microchannels
- Inner wall: closest to TM, monolayer of endothelial cells, incomplete sub-endothelial layer, no basement membrane, and tight junctions between cells
Scleral Spur
- Posterior wall of Schlemm's canal
- Site of anterior ciliary muscle attachment
- Prevents Schlemm's canal from collapsing under ciliary muscle contraction
Outflow Routes of Aqueous Humor
- Trabecular outflow: TM → Schlemm's canal → collector channel → episcleral plexus
- Uveoscleral drainage: fluid passes between the uveal trabeculae and ciliary muscle bundles → drain to the episclera
- Uveoscleral drainage affected by drugs and state of accommodation (ciliary muscle)
Ciliary Muscle on Aqueous Flow
- Ciliary muscle relaxed: decreases trabecular outflow, increases uveoscleral outflow
- Ciliary muscle contracted: increases trabecular outflow, decreases uveoscleral outflow
Anterior Chamber Angle
- Forms the junction between the cornea and iris
- Responsible for the drainage of aqueous humour
Trabecular Meshwork
- Located between Schwalbe's Line and the scleral spur
- Consists of three regions: uveal, corneoscleral, and juxtacanalicular/cribriform meshwork
- Uveal meshwork: closest to the anterior chamber, collagen and elastic lamellae network, and large openings between lamellae
- Corneoscleral meshwork: middle layer, perforated collagen and elastin plates covered by TM cells, and connects the scleral spur to the anterior wall of the scleral sulcus
- Juxtacanalicular/cribriform meshwork: loose connective tissue, sieve-like plates, and main source of resistance to aqueous flow
Trabecular Cells
- Endothelial: maintain passageway patency, neutralize reactive oxygen species
- Macrophage: biological filter/phagocytosis, immune mediation
- Fibroblastic: ECM turnover/tissue repair
- Smooth muscle: contractile tone, mechanotrasduction
Schlemm's Canal
- Outer wall: closest to sclera, monolayer of endothelial cells, well-developed basement membrane, and no transcellular microchannels
- Inner wall: closest to TM, monolayer of endothelial cells, incomplete sub-endothelial layer, no basement membrane, and tight junctions between cells
Scleral Spur
- Posterior wall of Schlemm's canal
- Site of anterior ciliary muscle attachment
- Prevents Schlemm's canal from collapsing under ciliary muscle contraction
Outflow Routes of Aqueous Humor
- Trabecular outflow: TM → Schlemm's canal → collector channel → episcleral plexus
- Uveoscleral drainage: fluid passes between the uveal trabeculae and ciliary muscle bundles → drain to the episclera
- Uveoscleral drainage affected by drugs and state of accommodation (ciliary muscle)
Ciliary Muscle on Aqueous Flow
- Ciliary muscle relaxed: decreases trabecular outflow, increases uveoscleral outflow
- Ciliary muscle contracted: increases trabecular outflow, decreases uveoscleral outflow
Lens Anatomy
- The lens is a transparent, biconvex, ellipsoid structure with a refractive power of +20D.
- It is composed of 66% water and 33% protein.
- The lens is avascular, meaning it has no blood vessels, and it has no nerves.
- Lens cells divide, but they do not shed, and the lens increases in size and weight with age.
Lens Development
- The lens develops from the optic pit, which forms during the 4th week of gestation.
- The lens placode invaginates to form the lens pit during the 5th week.
- The lens vesicle forms during the 6th week, and it is surrounded by an intact basement membrane.
- The posterior cells begin to elongate anteriorly during the 6th week, and they reach the anterior wall during the 7th week.
- The primary lens fibers fill the lens vesicle during the 8th week, and the intracellular organelles disappear.
Lens Parameters
- The lens thickness increases by about 0.02mm/year.
- At birth, the lens thickness is 3.5-4.0mm, and it increases to 4.75-5.0mm by 90 years.
- The equatorial diameter of the lens is 6.0-6.5mm at birth and 9.0-10.0mm in adults.
- The anterior radius of curvature is 8.0-14.0mm, and the posterior radius of curvature is 4.5-7.5mm.
Lens Capsule
- The lens capsule is a basement membrane with elastic properties.
- It is the point of attachment for the lens zonules.
- The capsule envelops the lens and has regional variations in thickness.
Lens Epithelium
- The lens epithelium is responsible for the growth and development of the entire lens.
- It is composed of simple cuboidal cells that become columnar near the equator.
- The epithelium is restricted to the anterior surface of the lens.
- The basal aspect of the epithelium is in contact with the capsule.
- The epithelium contains a nucleus and organelles.
- Gap junctions between cells maintain lens transparency.
Lens Fibers
- Lens fibers are the main component of the lens.
- They arise from the epithelium in the germinative zone.
- The cells elongate and then turn meridionally.
- The nucleus is displaced anteriorly, forming the lens bow.
- The fibers are hexagonal in cross-section and form rows.
- The fibers are thinner posteriorly, and their tips meet at a suture.
Lens Fiber Nucleus
- As lens fibers migrate to deeper layers, the cell organelles and nucleus degenerate.
- The cytoplasm becomes homogenous.
- The basal attachment of the fiber to the posterior capsule terminates.
Lens Sutures
- Lens sutures are formed by the overlap of the ends of secondary fibers.
- Primary fibers do not form sutures.
- Fetal secondary fibers form Y-shaped sutures, which become more complex in adolescence and adulthood.
Lens Zonules/Zonule of Zinn
- The lens zonules are fibers that pass from the ciliary body to the lens.
- They hold the lens in place and allow the ciliary muscle to act on the lens during accommodation.
- The zonules are composed of non-collagenous glycoprotein.
Lens Hydration
- Lens hydration is essential for transparency.
- The lens maintains hydration through a 'pump-leak' system.
- The posterior part of the lens has no epithelial barrier, allowing for free diffusion of ions, solutes, and water between the lens and vitreous.
- The anterior part of the lens actively transports K+ and amino acids into the lens.
Crystallin Proteins
- Crystallin proteins make up ~40% of the wet weight of the lens fiber cells.
- They have a higher refractive index than the surrounding fluid.
- They maintain hydration during lens deformation due to accommodation.
- The high concentration and dense packing of crystallin proteins mean that the majority of light scatter is cancelled out.
- There are three types of crystallin proteins: α-crystallin, β-crystallin, and γ-crystallin.
Lens Anatomy
- The lens is a transparent, biconvex, ellipsoid structure with a refractive power of +20D.
- It is composed of 66% water and 33% protein.
- The lens is avascular, meaning it has no blood vessels, and it has no nerves.
- Lens cells divide, but they do not shed, and the lens increases in size and weight with age.
Lens Development
- The lens develops from the optic pit, which forms during the 4th week of gestation.
- The lens placode invaginates to form the lens pit during the 5th week.
- The lens vesicle forms during the 6th week, and it is surrounded by an intact basement membrane.
- The posterior cells begin to elongate anteriorly during the 6th week, and they reach the anterior wall during the 7th week.
- The primary lens fibers fill the lens vesicle during the 8th week, and the intracellular organelles disappear.
Lens Parameters
- The lens thickness increases by about 0.02mm/year.
- At birth, the lens thickness is 3.5-4.0mm, and it increases to 4.75-5.0mm by 90 years.
- The equatorial diameter of the lens is 6.0-6.5mm at birth and 9.0-10.0mm in adults.
- The anterior radius of curvature is 8.0-14.0mm, and the posterior radius of curvature is 4.5-7.5mm.
Lens Capsule
- The lens capsule is a basement membrane with elastic properties.
- It is the point of attachment for the lens zonules.
- The capsule envelops the lens and has regional variations in thickness.
Lens Epithelium
- The lens epithelium is responsible for the growth and development of the entire lens.
- It is composed of simple cuboidal cells that become columnar near the equator.
- The epithelium is restricted to the anterior surface of the lens.
- The basal aspect of the epithelium is in contact with the capsule.
- The epithelium contains a nucleus and organelles.
- Gap junctions between cells maintain lens transparency.
Lens Fibers
- Lens fibers are the main component of the lens.
- They arise from the epithelium in the germinative zone.
- The cells elongate and then turn meridionally.
- The nucleus is displaced anteriorly, forming the lens bow.
- The fibers are hexagonal in cross-section and form rows.
- The fibers are thinner posteriorly, and their tips meet at a suture.
Lens Fiber Nucleus
- As lens fibers migrate to deeper layers, the cell organelles and nucleus degenerate.
- The cytoplasm becomes homogenous.
- The basal attachment of the fiber to the posterior capsule terminates.
Lens Sutures
- Lens sutures are formed by the overlap of the ends of secondary fibers.
- Primary fibers do not form sutures.
- Fetal secondary fibers form Y-shaped sutures, which become more complex in adolescence and adulthood.
Lens Zonules/Zonule of Zinn
- The lens zonules are fibers that pass from the ciliary body to the lens.
- They hold the lens in place and allow the ciliary muscle to act on the lens during accommodation.
- The zonules are composed of non-collagenous glycoprotein.
Lens Hydration
- Lens hydration is essential for transparency.
- The lens maintains hydration through a 'pump-leak' system.
- The posterior part of the lens has no epithelial barrier, allowing for free diffusion of ions, solutes, and water between the lens and vitreous.
- The anterior part of the lens actively transports K+ and amino acids into the lens.
Crystallin Proteins
- Crystallin proteins make up ~40% of the wet weight of the lens fiber cells.
- They have a higher refractive index than the surrounding fluid.
- They maintain hydration during lens deformation due to accommodation.
- The high concentration and dense packing of crystallin proteins mean that the majority of light scatter is cancelled out.
- There are three types of crystallin proteins: α-crystallin, β-crystallin, and γ-crystallin.
Anatomy Underpinning Accommodation
- Accommodation involves a dioptre change in the optical power of the eye, with an increase in curvature of the lens to focus on objects up close.
Accommodative Apparatus
- The ciliary muscle is arranged in three bundles: outer longitudinal, middle radial, and inner circular fibers.
- It attaches anteriorly to the scleral spur and trabecular meshwork, and posteriorly to the elastic network of Bruch's membrane and the choroid.
- The ciliary muscle has a primary function of stabilizing the lens and facilitating accommodation.
Zonules
- Zonules arise from the pars plana and are composed of non-collagenous glycoprotein secreted by the ciliary epithelium.
- They have three groups of fibers: anterior, equatorial, and posterior zonules.
- Zonules serve to stabilize the lens and facilitate accommodation.
Lens
- The lens is surrounded by a continuous basement membrane, known as the lens capsule, which has elastic properties and envelops the lens.
- The lens capsule has regional variations in thickness and serves as the point of attachment for the lens zonules.
Accommodation – Ciliary Muscle
- During accommodation, the outer longitudinal fibers of the ciliary muscle contract, causing the main mass of the muscle to move forward along the curved inner wall of the sclera.
- This forces the inner radial fibers and overlying ciliary processes to bulge inwards towards the posterior chamber.
Accommodation – Theories
- The mechanism of accommodation is still debated, with various studies and theories proposed.
Accommodation – Capsule
- The lens capsule plays a crucial role in accommodation, drawing the lens into a more accommodated form.
- Decapsulation results in flattening and an increase in focal length.
Lens Shape and Displacement
- During accommodation, the anterior pole of the lens is displaced, with the most displacement occurring in the nucleus rather than the cortex.
- This leads to increased nucleus thickness, shallowing of the anterior chamber, increased lens convexity, and closer proximity of the cornea to the anterior lens.
Neural Control of Accommodation
- The neural control of accommodation involves a blur signal sent to the primary visual cortex, then to the pretectal area, and finally to the Edinger-Westphal nucleus.
- Two signals are then sent: one via the parasympathetic pathway to the ciliary ganglion and ciliary muscle, and another via the CNIII to the medial rectus (convergence).
Accommodation and Convergence Reflex
- The accommodation/near reflex involves accommodation, pupil constriction, and convergence.
Presbyopia
- Presbyopia is a common presentation in clinic, typically occurring around 40 years old, characterized by a gradual inability to accommodate.
- It is caused by various contributors, including increased stiffness of the crystalline lens and changes in zonule insertion with age.
Anatomy Underpinning Accommodation
- Accommodation involves a dioptre change in the optical power of the eye, with an increase in curvature of the lens to focus on objects up close.
Accommodative Apparatus
- The ciliary muscle is arranged in three bundles: outer longitudinal, middle radial, and inner circular fibers.
- It attaches anteriorly to the scleral spur and trabecular meshwork, and posteriorly to the elastic network of Bruch's membrane and the choroid.
- The ciliary muscle has a primary function of stabilizing the lens and facilitating accommodation.
Zonules
- Zonules arise from the pars plana and are composed of non-collagenous glycoprotein secreted by the ciliary epithelium.
- They have three groups of fibers: anterior, equatorial, and posterior zonules.
- Zonules serve to stabilize the lens and facilitate accommodation.
Lens
- The lens is surrounded by a continuous basement membrane, known as the lens capsule, which has elastic properties and envelops the lens.
- The lens capsule has regional variations in thickness and serves as the point of attachment for the lens zonules.
Accommodation – Ciliary Muscle
- During accommodation, the outer longitudinal fibers of the ciliary muscle contract, causing the main mass of the muscle to move forward along the curved inner wall of the sclera.
- This forces the inner radial fibers and overlying ciliary processes to bulge inwards towards the posterior chamber.
Accommodation – Theories
- The mechanism of accommodation is still debated, with various studies and theories proposed.
Accommodation – Capsule
- The lens capsule plays a crucial role in accommodation, drawing the lens into a more accommodated form.
- Decapsulation results in flattening and an increase in focal length.
Lens Shape and Displacement
- During accommodation, the anterior pole of the lens is displaced, with the most displacement occurring in the nucleus rather than the cortex.
- This leads to increased nucleus thickness, shallowing of the anterior chamber, increased lens convexity, and closer proximity of the cornea to the anterior lens.
Neural Control of Accommodation
- The neural control of accommodation involves a blur signal sent to the primary visual cortex, then to the pretectal area, and finally to the Edinger-Westphal nucleus.
- Two signals are then sent: one via the parasympathetic pathway to the ciliary ganglion and ciliary muscle, and another via the CNIII to the medial rectus (convergence).
Accommodation and Convergence Reflex
- The accommodation/near reflex involves accommodation, pupil constriction, and convergence.
Presbyopia
- Presbyopia is a common presentation in clinic, typically occurring around 40 years old, characterized by a gradual inability to accommodate.
- It is caused by various contributors, including increased stiffness of the crystalline lens and changes in zonule insertion with age.
Vitreous Anatomy
- The vitreous is a flattened sphere that takes up approximately 80% of the globe's volume.
- It is a gel surrounded by a thin collagenous membrane.
- The anterior indentation, also known as the hyaloid/patellar fossa, surrounds the lens.
- The vitreous has a firm attachment to the retina.
Vitreous Composition
- The vitreous is composed of 99% water, 1% structural proteins, and few hyalocytes in the periphery.
- 15-20% of the water is bound to structural proteins.
- The structural proteins include:
- 75% type II collagen
- 15% type IX collagen
- Rest: V, VI, XI collagen, and hyaluronic acid (major GAG)
Vitreous Functions
- The vitreous maintains optical clarity due to its biochemical structure.
- It provides structural support to the globe, making up approximately 80% of the globe's volume.
- The vitreous supports the lens anteriorly and keeps the retinal adherence to the choroid/sclera.
- It absorbs external forces and reduces mechanical deformation of the globe.
- The vitreous acts as a molecule repository, receiving metabolites from the ciliary body and retina, and containing ions and organic molecules.
- It promotes intraocular wound healing via vitamin C reservoir and serves as an antioxidant.
Anatomical Zones
- The central/medullary zone is cell-free, contains collagen fibrils and hyaluronic acid, and is in a gel state.
- The cortex is approximately 100 µm thick, has a higher collagen concentration, and is 2% of the vitreous volume.
- The basal zone is located at the ora serrata, has dense, thickened collagen fibers, and is the site of strongest adherent to the retina.
Vitreous Biochemistry
- Type II collagen forms fibrils, while type IX collagen provides structural support to the fibrils.
- Type V/XI collagen co-assembles fibrils with type II collagen, and type VI collagen links fibrils to hyaluronan.
- Hyaluronic acid is a large glycosaminoglycan arranged in a network of long chains, interconnected to collagen fibrils, and ensures proper vitreous hydration and collagen spacing.
Aging Changes
- Liquefaction originates in the central region due to changes in hyaluronic acid conformation.
- Floaters occur when collagen fibril networks become free-floating bundles.
Vitreous Anatomy
- The vitreous is a flattened sphere that takes up approximately 80% of the globe's volume.
- It is a gel surrounded by a thin collagenous membrane.
- The anterior indentation, also known as the hyaloid/patellar fossa, surrounds the lens.
- The vitreous has a firm attachment to the retina.
Vitreous Composition
- The vitreous is composed of 99% water, 1% structural proteins, and few hyalocytes in the periphery.
- 15-20% of the water is bound to structural proteins.
- The structural proteins include:
- 75% type II collagen
- 15% type IX collagen
- Rest: V, VI, XI collagen, and hyaluronic acid (major GAG)
Vitreous Functions
- The vitreous maintains optical clarity due to its biochemical structure.
- It provides structural support to the globe, making up approximately 80% of the globe's volume.
- The vitreous supports the lens anteriorly and keeps the retinal adherence to the choroid/sclera.
- It absorbs external forces and reduces mechanical deformation of the globe.
- The vitreous acts as a molecule repository, receiving metabolites from the ciliary body and retina, and containing ions and organic molecules.
- It promotes intraocular wound healing via vitamin C reservoir and serves as an antioxidant.
Anatomical Zones
- The central/medullary zone is cell-free, contains collagen fibrils and hyaluronic acid, and is in a gel state.
- The cortex is approximately 100 µm thick, has a higher collagen concentration, and is 2% of the vitreous volume.
- The basal zone is located at the ora serrata, has dense, thickened collagen fibers, and is the site of strongest adherent to the retina.
Vitreous Biochemistry
- Type II collagen forms fibrils, while type IX collagen provides structural support to the fibrils.
- Type V/XI collagen co-assembles fibrils with type II collagen, and type VI collagen links fibrils to hyaluronan.
- Hyaluronic acid is a large glycosaminoglycan arranged in a network of long chains, interconnected to collagen fibrils, and ensures proper vitreous hydration and collagen spacing.
Aging Changes
- Liquefaction originates in the central region due to changes in hyaluronic acid conformation.
- Floaters occur when collagen fibril networks become free-floating bundles.
Retinal Landmarks
- Posterior pole landmarks include macula, perifovea, parafovea, fovea, foveola, and umbo.
- The optic nerve head (optic disc) is a pinkish, oval area approximately 2 * 1.5 mm in size, located 17° (4.5 to 5 mm) nasal to the fovea.
- The foveal avascular zone has minimal overlying inner retina, and its centre is the point of fixation.
Retina Structure
- The retina is a circular disc of between 30 and 40 mm in diameter.
- The central retina is thicker than the peripheral retina.
- The retina has ten distinct layers, including the retinal pigmented epithelium (RPE), photoreceptor layer, outer nuclear layer, outer plexiform layer, inner nuclear layer, inner plexiform layer, ganglion cell layer, nerve fibre layer, and inner limiting membrane.
Retinal Layers
- The retinal pigmented epithelium (RPE) is the outermost layer, supporting the retina and playing a crucial role in photopigment regeneration and the blood-retinal barrier.
- The photoreceptor layer contains the outer and inner segments of rod and cone photoreceptors.
- The outer nuclear layer contains the cell bodies of rods and cones.
- The outer plexiform layer is the junction between rod and cone axons and the dendrites of horizontal and bipolar cells.
- The inner nuclear layer contains the cell bodies of horizontal, bipolar, amacrine, and Müller cells.
- The inner plexiform layer is the junction between the axons of bipolar and amacrine cells and the dendrites of ganglion cells.
- The ganglion cell layer contains the nuclei of the ganglion cells and displaced amacrine cells.
- The retinal nerve fibre layer contains the fibres from ganglion cells traversing the retina to leave the eyeball at the optic disc.
- The inner limiting membrane is the end feet of the Müller cells.
Photoreceptors
- There are 126 million rods and cones in the human retina, converging to 1 million ganglion cells.
- Rods have a higher convergence ratio than cones, with an average of 120 rods to one ganglion cell.
- Cones have a lower convergence ratio, with an average of 6 cones to one ganglion cell.
- Cones in the fovea have a 1:1 connection to ganglion cells.
Visual Pathways
- The through pathway consists of photoreceptors, bipolar cells, and ganglion cells.
- The lateral pathway involves horizontal and amacrine cells, providing local feedback to optimize the through pathway.
Glial Cells
- There are three types of glial cells: Müller cells, astrocytes, and microglia.
- Müller cells span the entire retina, clearing metabolic waste, facilitating neurotransmitter recycling, and maintaining ionic balances.
- Astrocytes are found in the retinal nerve fibre layer, with a peak distribution on the optic nerve head.
- Microglia are found in every retinal layer and function as macrophages in response to trauma.
Retinal Pigment Epithelium (RPE)
- The RPE is a single-layer cell between the photoreceptors and choroid, connected by tight junctions.
- The RPE acts as a sieve between the choriocapillaris and photoreceptors, and forms part of the blood-retina barrier.
- The RPE also plays a crucial role in photopigment regeneration and recycling.
Retinal Landmarks
- Posterior pole landmarks include macula, perifovea, parafovea, fovea, foveola, and umbo.
- The optic nerve head (optic disc) is a pinkish, oval area approximately 2 * 1.5 mm in size, located 17° (4.5 to 5 mm) nasal to the fovea.
- The foveal avascular zone has minimal overlying inner retina, and its centre is the point of fixation.
Retina Structure
- The retina is a circular disc of between 30 and 40 mm in diameter.
- The central retina is thicker than the peripheral retina.
- The retina has ten distinct layers, including the retinal pigmented epithelium (RPE), photoreceptor layer, outer nuclear layer, outer plexiform layer, inner nuclear layer, inner plexiform layer, ganglion cell layer, nerve fibre layer, and inner limiting membrane.
Retinal Layers
- The retinal pigmented epithelium (RPE) is the outermost layer, supporting the retina and playing a crucial role in photopigment regeneration and the blood-retinal barrier.
- The photoreceptor layer contains the outer and inner segments of rod and cone photoreceptors.
- The outer nuclear layer contains the cell bodies of rods and cones.
- The outer plexiform layer is the junction between rod and cone axons and the dendrites of horizontal and bipolar cells.
- The inner nuclear layer contains the cell bodies of horizontal, bipolar, amacrine, and Müller cells.
- The inner plexiform layer is the junction between the axons of bipolar and amacrine cells and the dendrites of ganglion cells.
- The ganglion cell layer contains the nuclei of the ganglion cells and displaced amacrine cells.
- The retinal nerve fibre layer contains the fibres from ganglion cells traversing the retina to leave the eyeball at the optic disc.
- The inner limiting membrane is the end feet of the Müller cells.
Photoreceptors
- There are 126 million rods and cones in the human retina, converging to 1 million ganglion cells.
- Rods have a higher convergence ratio than cones, with an average of 120 rods to one ganglion cell.
- Cones have a lower convergence ratio, with an average of 6 cones to one ganglion cell.
- Cones in the fovea have a 1:1 connection to ganglion cells.
Visual Pathways
- The through pathway consists of photoreceptors, bipolar cells, and ganglion cells.
- The lateral pathway involves horizontal and amacrine cells, providing local feedback to optimize the through pathway.
Glial Cells
- There are three types of glial cells: Müller cells, astrocytes, and microglia.
- Müller cells span the entire retina, clearing metabolic waste, facilitating neurotransmitter recycling, and maintaining ionic balances.
- Astrocytes are found in the retinal nerve fibre layer, with a peak distribution on the optic nerve head.
- Microglia are found in every retinal layer and function as macrophages in response to trauma.
Retinal Pigment Epithelium (RPE)
- The RPE is a single-layer cell between the photoreceptors and choroid, connected by tight junctions.
- The RPE acts as a sieve between the choriocapillaris and photoreceptors, and forms part of the blood-retina barrier.
- The RPE also plays a crucial role in photopigment regeneration and recycling.
Retinal Landmarks
- Posterior pole landmarks include macula, perifovea, parafovea, fovea, foveola, and umbo.
- The optic nerve head (optic disc) is a pinkish, oval area approximately 2 * 1.5 mm in size, located 17° (4.5 to 5 mm) nasal to the fovea.
- The foveal avascular zone has minimal overlying inner retina, and its centre is the point of fixation.
Retina Structure
- The retina is a circular disc of between 30 and 40 mm in diameter.
- The central retina is thicker than the peripheral retina.
- The retina has ten distinct layers, including the retinal pigmented epithelium (RPE), photoreceptor layer, outer nuclear layer, outer plexiform layer, inner nuclear layer, inner plexiform layer, ganglion cell layer, nerve fibre layer, and inner limiting membrane.
Retinal Layers
- The retinal pigmented epithelium (RPE) is the outermost layer, supporting the retina and playing a crucial role in photopigment regeneration and the blood-retinal barrier.
- The photoreceptor layer contains the outer and inner segments of rod and cone photoreceptors.
- The outer nuclear layer contains the cell bodies of rods and cones.
- The outer plexiform layer is the junction between rod and cone axons and the dendrites of horizontal and bipolar cells.
- The inner nuclear layer contains the cell bodies of horizontal, bipolar, amacrine, and Müller cells.
- The inner plexiform layer is the junction between the axons of bipolar and amacrine cells and the dendrites of ganglion cells.
- The ganglion cell layer contains the nuclei of the ganglion cells and displaced amacrine cells.
- The retinal nerve fibre layer contains the fibres from ganglion cells traversing the retina to leave the eyeball at the optic disc.
- The inner limiting membrane is the end feet of the Müller cells.
Photoreceptors
- There are 126 million rods and cones in the human retina, converging to 1 million ganglion cells.
- Rods have a higher convergence ratio than cones, with an average of 120 rods to one ganglion cell.
- Cones have a lower convergence ratio, with an average of 6 cones to one ganglion cell.
- Cones in the fovea have a 1:1 connection to ganglion cells.
Visual Pathways
- The through pathway consists of photoreceptors, bipolar cells, and ganglion cells.
- The lateral pathway involves horizontal and amacrine cells, providing local feedback to optimize the through pathway.
Glial Cells
- There are three types of glial cells: Müller cells, astrocytes, and microglia.
- Müller cells span the entire retina, clearing metabolic waste, facilitating neurotransmitter recycling, and maintaining ionic balances.
- Astrocytes are found in the retinal nerve fibre layer, with a peak distribution on the optic nerve head.
- Microglia are found in every retinal layer and function as macrophages in response to trauma.
Retinal Pigment Epithelium (RPE)
- The RPE is a single-layer cell between the photoreceptors and choroid, connected by tight junctions.
- The RPE acts as a sieve between the choriocapillaris and photoreceptors, and forms part of the blood-retina barrier.
- The RPE also plays a crucial role in photopigment regeneration and recycling.
Optic Nerve Head (ONH) Anatomy and Function
- The optic nerve head (ONH) is the exit point for ganglion cell axons from the globe, carrying visual information to the brain.
- The optic nerve consists of four main sections: intraocular, intraorbital, intracanalicular, and intracranial.
Retina Structure
- The retina consists of 10 layers:
- Internal limiting membrane
- Nerve fibre layer
- Ganglion cell layer
- Inner plexiform layer
- Inner nuclear layer
- Outer plexiform layer
- Outer nuclear layer
- Photoreceptor layer (inner and outer segments)
- External limiting membrane
- Retinal pigment epithelium
- Choroid
Optic Disc/Optic Nerve Head (ONH)
- The optic disc is the area where the optic nerve meets the eye.
- The optic disc has a vertical oval shape and is slightly raised due to the convergence of nerve fibers.
- The optic cup is a funnel-shaped depression in the optic disc.
- The optic disc is pink due to a rich capillary supply to its rim.
- The white portion is the base of the cup.
ONH Divisions
- The optic nerve head (ONH) extends from the inner retina to a plane level with the posterior sclera.
- The ONH can be divided into four sections:
- Superficial nerve fibre layer (A)
- Prelaminar region (B)
- Lamina cribrosa (C)
- Retrolaminar region (D)
Superficial Nerve Fibre Layer (RNFL)
- The superficial nerve fibre layer consists of nerve fibres organized into bundles that converge towards the disc.
- There is no overlap between the upper and lower halves of the retinal fibres.
- The nerve fibres at the edge of the nerve serve the retina furthest from the nerve.
Prelaminar Region
- The prelaminar region consists of astrocytes and nerve fibres arranged in bundles.
- The astrocytes increase in number posteriorly, forming a sieve-like structure, the glial lamina cribrosa.
Lamina Cribrosa
- The lamina cribrosa is a band of dense, specialized extracellular matrix that provides mechanical protection to the ONH against IOP.
- It is composed of fenestrated sheets of connective tissue and occasional elastic fibres.
- It bridges the scleral canal and allows passage of RGC axons and blood vessels.
Retrolaminar Region
- The retrolaminar region is the transition zone from the optic nerve head to the orbital optic nerve.
- Nerve axons become myelinated, increasing the nerve diameter and allowing for faster and more efficient signal conduction.
- The optic nerve is surrounded by the meningeal sheath, which consists of dura mater, arachnoid mater, and pia mater.
Blood Supply
- The optic disc surface is supplied by the central retinal artery (CRA) and choroid.
- The prelaminar and laminar regions are supplied by short posterior ciliary arteries, which form a circular arterial anastomosis at the scleral level, the circle of Zinn-Haller.
- The retrolaminar region is supplied by pial blood vessels.
Blood-Retina Barrier
- The blood-retina barrier is formed by a series of tight junctions between the lining glial cells and the adjacent RPE.
- Plasma proteins readily leak from the choroid into the ONH directly and through the sclera.
- The entry of proteins from the ONH into the retina is blocked by the blood-retina barrier.
Optic Nerve Head (ONH) Anatomy and Function
- The optic nerve head (ONH) is the exit point for ganglion cell axons from the globe, carrying visual information to the brain.
- The optic nerve consists of four main sections: intraocular, intraorbital, intracanalicular, and intracranial.
Retina Structure
- The retina consists of 10 layers:
- Internal limiting membrane
- Nerve fibre layer
- Ganglion cell layer
- Inner plexiform layer
- Inner nuclear layer
- Outer plexiform layer
- Outer nuclear layer
- Photoreceptor layer (inner and outer segments)
- External limiting membrane
- Retinal pigment epithelium
- Choroid
Optic Disc/Optic Nerve Head (ONH)
- The optic disc is the area where the optic nerve meets the eye.
- The optic disc has a vertical oval shape and is slightly raised due to the convergence of nerve fibers.
- The optic cup is a funnel-shaped depression in the optic disc.
- The optic disc is pink due to a rich capillary supply to its rim.
- The white portion is the base of the cup.
ONH Divisions
- The optic nerve head (ONH) extends from the inner retina to a plane level with the posterior sclera.
- The ONH can be divided into four sections:
- Superficial nerve fibre layer (A)
- Prelaminar region (B)
- Lamina cribrosa (C)
- Retrolaminar region (D)
Superficial Nerve Fibre Layer (RNFL)
- The superficial nerve fibre layer consists of nerve fibres organized into bundles that converge towards the disc.
- There is no overlap between the upper and lower halves of the retinal fibres.
- The nerve fibres at the edge of the nerve serve the retina furthest from the nerve.
Prelaminar Region
- The prelaminar region consists of astrocytes and nerve fibres arranged in bundles.
- The astrocytes increase in number posteriorly, forming a sieve-like structure, the glial lamina cribrosa.
Lamina Cribrosa
- The lamina cribrosa is a band of dense, specialized extracellular matrix that provides mechanical protection to the ONH against IOP.
- It is composed of fenestrated sheets of connective tissue and occasional elastic fibres.
- It bridges the scleral canal and allows passage of RGC axons and blood vessels.
Retrolaminar Region
- The retrolaminar region is the transition zone from the optic nerve head to the orbital optic nerve.
- Nerve axons become myelinated, increasing the nerve diameter and allowing for faster and more efficient signal conduction.
- The optic nerve is surrounded by the meningeal sheath, which consists of dura mater, arachnoid mater, and pia mater.
Blood Supply
- The optic disc surface is supplied by the central retinal artery (CRA) and choroid.
- The prelaminar and laminar regions are supplied by short posterior ciliary arteries, which form a circular arterial anastomosis at the scleral level, the circle of Zinn-Haller.
- The retrolaminar region is supplied by pial blood vessels.
Blood-Retina Barrier
- The blood-retina barrier is formed by a series of tight junctions between the lining glial cells and the adjacent RPE.
- Plasma proteins readily leak from the choroid into the ONH directly and through the sclera.
- The entry of proteins from the ONH into the retina is blocked by the blood-retina barrier.
Choroid Anatomy
- Located underneath the retina, highly vascularized
- Supplied by short posterior ciliary arteries (SPCA) and long posterior ciliary arteries (LPCA), drains via vortex veins
- Thickness decreases with age, from ~200 µm at birth to 80 µm by 90 years old
Choroid Functions
- Supplies nutrients and oxygen to outer retina
- Regulates temperature through heat dissipation
- Modulates intraocular pressure (IOP) via blood flow control
- Drains aqueous humour via uveoscleral pathway, accounting for approximately 10-15% of drainage in humans
Choroid Layers
- Arterial vessels are interspersed with veins
- Consists of 5 layers, including:
- Sattler's layer (~ 100 µm thick, contains medium to small-sized vessels)
- Haller's layer (~ 200 µm thick, contains large-sized vessels)
- Note: Haller's and Sattler's layers are histologically defined but do not have precise borders in imaging
Bruch's Membrane
- Thickness: ~ 2-4 µm
- Composition: elastin and collagen-rich extracellular matrix (ECM)
- Function: regulates movement of molecules between RPE and choroidal circulation
- Aging changes: fibre calcification, increased fibre cross-linkage, accumulation of fat and advanced glycation end products
Choriocapillaris
- Thickness: ~ 10 µm at fovea, thinning to ~7 µm peripherally
- Feeder arteriole from Sattler's layer supplies a hexagonal area
Suprachoroid
- Thickness: ~ 30 µm
- Transition zone between choroid and sclera
- Composition: collagen fibres, fibroblasts, and melanocytes
- Of pharmacological interest as a drug delivery target for chorioretinal layer
Clinical Assessment of the Choroid
- Indocyanine green (ICG) angiography: aka choroidal angiography, appears as generalized hyperfluorescence
- Optical coherence tomography angiography (OCTa): non-invasive, detects movement of red blood cells, produces enface imaging of retina and choroid vessels
Clinical Relevance
- Choroid is critical in retinal homeostasis
- Associated with diseases such as Vogt-Koyanagi-Harada's disease and age-related macular degeneration (AMD)
Choroid Anatomy
- Located underneath the retina, highly vascularized
- Supplied by short posterior ciliary arteries (SPCA) and long posterior ciliary arteries (LPCA), drains via vortex veins
- Thickness decreases with age, from ~200 µm at birth to 80 µm by 90 years old
Choroid Functions
- Supplies nutrients and oxygen to outer retina
- Regulates temperature through heat dissipation
- Modulates intraocular pressure (IOP) via blood flow control
- Drains aqueous humour via uveoscleral pathway, accounting for approximately 10-15% of drainage in humans
Choroid Layers
- Arterial vessels are interspersed with veins
- Consists of 5 layers, including:
- Sattler's layer (~ 100 µm thick, contains medium to small-sized vessels)
- Haller's layer (~ 200 µm thick, contains large-sized vessels)
- Note: Haller's and Sattler's layers are histologically defined but do not have precise borders in imaging
Bruch's Membrane
- Thickness: ~ 2-4 µm
- Composition: elastin and collagen-rich extracellular matrix (ECM)
- Function: regulates movement of molecules between RPE and choroidal circulation
- Aging changes: fibre calcification, increased fibre cross-linkage, accumulation of fat and advanced glycation end products
Choriocapillaris
- Thickness: ~ 10 µm at fovea, thinning to ~7 µm peripherally
- Feeder arteriole from Sattler's layer supplies a hexagonal area
Suprachoroid
- Thickness: ~ 30 µm
- Transition zone between choroid and sclera
- Composition: collagen fibres, fibroblasts, and melanocytes
- Of pharmacological interest as a drug delivery target for chorioretinal layer
Clinical Assessment of the Choroid
- Indocyanine green (ICG) angiography: aka choroidal angiography, appears as generalized hyperfluorescence
- Optical coherence tomography angiography (OCTa): non-invasive, detects movement of red blood cells, produces enface imaging of retina and choroid vessels
Clinical Relevance
- Choroid is critical in retinal homeostasis
- Associated with diseases such as Vogt-Koyanagi-Harada's disease and age-related macular degeneration (AMD)
Inflammation
- Inflammation is the body's immune system response to an irritant, and can be acute or chronic
- Involves cells, proteins, and other mediators from both innate and adaptive immune systems
- Initiated by signals from injured cells or immune system cells
- Causes controlled destabilization of blood vessels and associated exudation of blood contents
- Alters blood flow in the local area
Purpose of Inflammation
- Protects against injury by eliminating its cause, limiting its consequences, and preventing sequelae
- Initiates the healing and regeneration process
- However, excessive inflammation can cause more damage than the initial injury
Clinical Signs of Inflammation
- Signs of acute inflammation include:
- Rubor (redness)
- Calor (heat)
- Tumor (swelling)
- Dolor (pain)
- Lead to loss of function
Inflammation in the Eye
- Ocular surface allergy (e.g., seasonal allergic conjunctivitis) involves eosinophil cells and serous fluid
- Corneal infection (e.g., bacterial keratitis) involves neutrophil cells and spills off the ocular surface
- Anterior chamber reaction (e.g., anterior uveitis) involves various cells and proteins (e.g., fibrin)
- Chorioretinal inflammation (e.g., posterior uveitis in toxoplasma infection) involves cells and proteins
Ocular Immune Privilege
- Cell and protein response in inflammation inside the eye can reduce vision and lead to permanent visual loss
- The system exists to limit excessive immune response inside the eye
- Evidence for ocular immune privilege includes:
- Success of corneal transplantation
- Unrestricted growth of non-self tumor cells inside the eye
- Aqueous and vitreous fluids inhibit inflammatory cells in vitro
- Signaling protein TGF-β2 is high in the eye, produced by RPE and pigment epithelium of the ciliary body and iris, and "disarms" inflammatory cells
Blood-Ocular Barriers
- Three main sites of blood-ocular barriers:
- Iris (blood-aqueous barrier)
- Ciliary body (blood-aqueous barrier)
- Retina (blood-retina barrier, with two separate locations)
- Blood-ocular barrier in the iris:
- Dye stays within iris blood vessels
- Minimal dye detected in aqueous
- Passage of macromolecules is minimized
- Capillaries are not fenestrated, and tight junctions form the cell-cell bond
- Blood-ocular barrier in the ciliary body:
- Dye marker leaks from blood vessels into ciliary body tissue
- Blood vessels in the ciliary stroma leak, but not outside the ciliary stroma
- No barrier to macromolecules
- Blood-ocular barrier in the retina:
- Retinal vessels do not leak marker dye
- Choroidal vessels freely leak marker dye, but not into the retina
- Tight junctions in capillary endothelium, and fenestrated blood vessels in the choroid
- Breakdown of blood-ocular barriers in inflammation:
- Inflammatory cells and proteins mix with aqueous when the iris and ciliary body are inflamed
- Tight junctions break down, allowing macromolecules to pass through
Inflammation
- Inflammation is the body's immune system response to an irritant, and can be acute or chronic
- Involves cells, proteins, and other mediators from both innate and adaptive immune systems
- Initiated by signals from injured cells or immune system cells
- Causes controlled destabilization of blood vessels and associated exudation of blood contents
- Alters blood flow in the local area
Purpose of Inflammation
- Protects against injury by eliminating its cause, limiting its consequences, and preventing sequelae
- Initiates the healing and regeneration process
- However, excessive inflammation can cause more damage than the initial injury
Clinical Signs of Inflammation
- Signs of acute inflammation include:
- Rubor (redness)
- Calor (heat)
- Tumor (swelling)
- Dolor (pain)
- Lead to loss of function
Inflammation in the Eye
- Ocular surface allergy (e.g., seasonal allergic conjunctivitis) involves eosinophil cells and serous fluid
- Corneal infection (e.g., bacterial keratitis) involves neutrophil cells and spills off the ocular surface
- Anterior chamber reaction (e.g., anterior uveitis) involves various cells and proteins (e.g., fibrin)
- Chorioretinal inflammation (e.g., posterior uveitis in toxoplasma infection) involves cells and proteins
Ocular Immune Privilege
- Cell and protein response in inflammation inside the eye can reduce vision and lead to permanent visual loss
- The system exists to limit excessive immune response inside the eye
- Evidence for ocular immune privilege includes:
- Success of corneal transplantation
- Unrestricted growth of non-self tumor cells inside the eye
- Aqueous and vitreous fluids inhibit inflammatory cells in vitro
- Signaling protein TGF-β2 is high in the eye, produced by RPE and pigment epithelium of the ciliary body and iris, and "disarms" inflammatory cells
Blood-Ocular Barriers
- Three main sites of blood-ocular barriers:
- Iris (blood-aqueous barrier)
- Ciliary body (blood-aqueous barrier)
- Retina (blood-retina barrier, with two separate locations)
- Blood-ocular barrier in the iris:
- Dye stays within iris blood vessels
- Minimal dye detected in aqueous
- Passage of macromolecules is minimized
- Capillaries are not fenestrated, and tight junctions form the cell-cell bond
- Blood-ocular barrier in the ciliary body:
- Dye marker leaks from blood vessels into ciliary body tissue
- Blood vessels in the ciliary stroma leak, but not outside the ciliary stroma
- No barrier to macromolecules
- Blood-ocular barrier in the retina:
- Retinal vessels do not leak marker dye
- Choroidal vessels freely leak marker dye, but not into the retina
- Tight junctions in capillary endothelium, and fenestrated blood vessels in the choroid
- Breakdown of blood-ocular barriers in inflammation:
- Inflammatory cells and proteins mix with aqueous when the iris and ciliary body are inflamed
- Tight junctions break down, allowing macromolecules to pass through
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Learn about the structure and dimensions of the cornea, the transparent anterior part of the eye. Explore its layers, shape, and size.