Podcast
Questions and Answers
What is the primary function of the uterus during pregnancy?
What is the primary function of the uterus during pregnancy?
- To provide a place for implantation and nourishment (correct)
- To facilitate menstrual flow
- To store urine until excretion
- To produce hormones for ovulation
Which part of the uterus is considered the uppermost region and connects to the fallopian tubes?
Which part of the uterus is considered the uppermost region and connects to the fallopian tubes?
- Fundus (correct)
- Body (corpus)
- Isthmus
- Cervix
What significant change occurs to the uterus after pregnancy?
What significant change occurs to the uterus after pregnancy?
- It remains larger and heavier than before (correct)
- It becomes permanently rigid and immobile
- It completely dissolves within the body
- It returns to its exact nonpregnant size
During which process is an incision typically made in the isthmus of the uterus?
During which process is an incision typically made in the isthmus of the uterus?
What is the name of the opening at the junction of the cervix and isthmus?
What is the name of the opening at the junction of the cervix and isthmus?
What triggers the hypothalamus to stimulate the anterior pituitary gland in males?
What triggers the hypothalamus to stimulate the anterior pituitary gland in males?
What is the primary androgenic hormone responsible for muscular development in males?
What is the primary androgenic hormone responsible for muscular development in males?
Which of the following changes occurs in males due to rising testosterone levels?
Which of the following changes occurs in males due to rising testosterone levels?
What is the first stage of female sexual development during puberty?
What is the first stage of female sexual development during puberty?
What role does estradiol play in adult males?
What role does estradiol play in adult males?
At what age does menarche typically begin?
At what age does menarche typically begin?
In males, which process is continuous and does not follow a cyclic pattern?
In males, which process is continuous and does not follow a cyclic pattern?
Which of the following is true regarding the growth of female reproductive organs during puberty?
Which of the following is true regarding the growth of female reproductive organs during puberty?
What defines the unitive aspect of sexual intercourse?
What defines the unitive aspect of sexual intercourse?
During which stage does sex assigned at birth get determined?
During which stage does sex assigned at birth get determined?
What initiates the development of secondary sex characteristics in females during puberty?
What initiates the development of secondary sex characteristics in females during puberty?
What occurs if testosterone is not available during the development in utero?
What occurs if testosterone is not available during the development in utero?
What is a requirement for the procreative meaning of sexual acts?
What is a requirement for the procreative meaning of sexual acts?
What are gonads responsible for?
What are gonads responsible for?
At what week do external genitals begin to form?
At what week do external genitals begin to form?
What must a female generally reach for puberty to be initiated?
What must a female generally reach for puberty to be initiated?
What is the primary function of the scrotum?
What is the primary function of the scrotum?
What condition is described as the presence of testes that remain in the pelvic cavity?
What condition is described as the presence of testes that remain in the pelvic cavity?
Which hormone is primarily responsible for stimulating testosterone release from the testes?
Which hormone is primarily responsible for stimulating testosterone release from the testes?
Which structure is responsible for conducting sperm from the epididymis to the ejaculatory duct?
Which structure is responsible for conducting sperm from the epididymis to the ejaculatory duct?
What role does the seminal vesicle play in male reproductive physiology?
What role does the seminal vesicle play in male reproductive physiology?
What is the composition breakdown of semen from the different glands?
What is the composition breakdown of semen from the different glands?
What causes the penis to become engorged during sexual excitement?
What causes the penis to become engorged during sexual excitement?
What is the average length of the male urethra?
What is the average length of the male urethra?
Which of the following glands contributes the least to semen volume?
Which of the following glands contributes the least to semen volume?
What is the primary function of the labia majora?
What is the primary function of the labia majora?
Which of the following structures is associated with the Clitoris?
Which of the following structures is associated with the Clitoris?
What role do the Skene and Bartholin glands play during coitus?
What role do the Skene and Bartholin glands play during coitus?
What happens to the labia minora after menopause?
What happens to the labia minora after menopause?
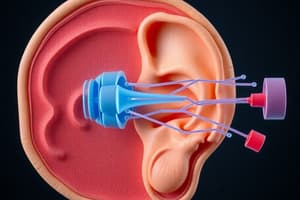
How is the fallopian tube anatomically divided?
How is the fallopian tube anatomically divided?
What occurs when the ischiocavernosus muscle contracts?
What occurs when the ischiocavernosus muscle contracts?
What is the purpose of the mons veneris?
What is the purpose of the mons veneris?
Which structure is likely to tear during childbirth?
Which structure is likely to tear during childbirth?
What is the main vascular supply to the external genitalia?
What is the main vascular supply to the external genitalia?
Which part of the fallopian tube is the site where fertilization usually occurs?
Which part of the fallopian tube is the site where fertilization usually occurs?
What can happen if there is pressure on the veins by the fetal head during labor?
What can happen if there is pressure on the veins by the fetal head during labor?
What is hematocolpometra?
What is hematocolpometra?
What is a common characteristic of the labia minora before menarche?
What is a common characteristic of the labia minora before menarche?
What is the function of mucus in the fallopian tube?
What is the function of mucus in the fallopian tube?
Study Notes
Unitive and Procreative Health
-
Unitive Health emphasizes the specific physical union of a man and a woman in natural intercourse, open to life and towards procreation. This meaning is solely found in natural intercourse between a man and a woman. Consequently, other sexual acts are considered non-unitive and inherently wrong, even between partners.
-
Procreative Health is found exclusively in natural intercourse. Even if every natural sexual act doesn't produce new life, the potential for new life is essential for a good moral object of the procreative meaning. Any sexual act not ordered towards procreation is inherently wrong.
Intrauterine Development
-
Intrauterine Development is the period between conception and birth, where sex assignment at birth is usually determined by chromosomal information at conception.
-
Gonads, the organs responsible for producing reproductive cells, are present by 5 weeks.
-
By week 7 or 8, in chromosomal males, testosterone production begins in early gonadal tissue, leading to development of male reproductive organs.
-
By week 10, if testosterone isn't present, female reproductive organs develop.
-
By week 12, external genitalia begin to form, including the penis for chromosomal males and uterus, labia minora, and majora for chromosomal females.
-
Ambiguous genitalia can occur if testosterone production halts in utero.
Pubertal Development
-
Puberty is the stage where secondary sex changes begin.
-
In most chromosomal females, these changes are triggered by GnRH release from the hypothalamus which stimulates the anterior pituitary gland to release FSH and LH. These gonadotropins initiate the production of androgens and estrogens, which lead to secondary characteristics and egg production.
-
Prepubescent boys and girls need to reach a critical weight (around 95 lbs or 43 kg) or body fat percentage before the hypothalamus is triggered.
-
Androgens are responsible for muscle development, physical growth, and increased sebaceous gland secretions leading to acne in adolescents.
-
In males, testosterone production starts in the adrenal cortex and testes. During puberty, testosterone production increases leading to changes in the testes, scrotum, penis, prostate, seminal vesicles, pubic, axillary and facial hair growth, larynx enlargement, voice changes, sperm maturation, and closure of growth plates in long bones.
-
In females, androgen is produced in the adrenal cortex and ovaries. Androgen primarily leads to the enlargement of the labia majora and clitoris and the formation of axillary and pubic hair.
-
Estrogen production begins in the ovarian follicle in females at puberty. Estrogen drives the development of the uterus, fallopian tubes, vagina, typical fat distribution, hair patterns, breast development, and closes the epiphyses.
-
Thelarche, the beginning of breast enlargement, starts 1-2 years before menstruation.
-
In males, estradiol is crucial for modulating libido, erectile function, and spermatogenesis.
Secondary Sex Characteristics
- Adolescent sexual development occurs in distinct stages, with different characteristics emerging for both sexes.
Females
-
Growth spurt, increases in transverse pelvic diameter, breast development, pubic hair growth, and the onset of menstruation.
-
Menarche, the onset of menstruation, typically occurs at 12.4 years of age.
-
Regular menstruation doesn't start until consistent ovulation, which usually happens 1-2 years after menarche.
-
Ova production ceases at menopause.
-
Growth of axillary hair and vaginal secretions.
Males
-
Weight gain, growth of testes, facial, axillary, and pubic hair, voice changes, penile growth, increases in height, and spermatogenesis.
-
Unlike ova, sperm production does not begin in intrauterine life and does not occur cyclically.
-
Sperm production is a continuous process from puberty throughout life.
Male Reproductive System
-
The male reproductive system, associated with the XY chromosome, differs greatly in appearance and function from the female reproductive system. However, they are homologues, meaning they have a shared embryonic origin.
-
Andrology focuses on the male reproductive system.
External Structures
-
Testes, encased in the scrotum and penis.
-
Scrotum, a muscular pouch suspended from the perineum, supports the testes and regulates sperm temperature.
-
Testes, two ovoid glands located within the scrotum, are encased in a protective fibrous capsule. Each testis contains lobules that produce testosterone and spermatozoa.
-
Cryptorchidism, the failure of testes to descend into the scrotal sac, requires monitoring after birth.
-
Penis, containing three cylindrical masses of erectile tissue, acts as the outlet for both the urinary and reproductive tracts.
-
Glans, the bulging, sensitive ridge of tissue at the distal end of the penis, is protected by the prepuce.
-
Circumcision, surgical removal of the prepuce, is associated with reduced risk of STIs and penile cancer.
Internal Structures
-
Epididymis, tightly coiled tube that receives sperm from seminiferous tubules and conducts it to the vas deferens.
-
Vas Deferens, a hollow tube carrying sperm from the epididymis to the abdominal cavity and ends at the seminal vesicle.
-
Seminal Vesicle, a pair of pouches that secrete viscous alkaline fluid, making sperm mobile.
-
Prostate Gland, located below the bladder, secretes alkaline fluid, increasing the sperm's pH.
-
Bulbourethral Glands, located beside the prostate gland, contribute alkaline fluid further enhancing sperm safety.
-
Urethra, a hollow tube extending from the bladder through the penis, carrying both urine and semen.
Female Reproductive System
- The female reproductive system, associated with the XX chromosome, has both internal and external components. Gynecology studies the female reproductive system.
External Structures
-
Vulva: encompassing the mons veneris, labia majora and minora, vestibule, clitoris, prepuce, Skene glands, Bartholin glands, fourchette, perineal body, and hymen.
-
Mons Veneris: a pad of adipose tissue located over the pubic symphysis, protects the pubic bone joint.
-
Labia Minora: hairless folds of connective tissue varying in size and shape.
-
Labia Majora: fused folds of tissue laterally positioned to the labia minora, protecting the external genitalia.
-
Vestibule: flattened surface where the opening of the bladder and uterus are located.
-
Clitoris: a sensitive organ of erectile tissue, central to sexual arousal and orgasm.
-
Skene glands: located between the urinary meatus, ducts open into the urethra.
-
Bartholin glands: located on each side of the vagina, ducts open into the proximal vagina near the labia minora and hymen.
-
Fourchette: a ridge of tissue formed by the posterior labia minora and majora, susceptible to tearing (laceration) or cutting (episiotomy) during childbirth.
-
Perineal Body/Muscle: located posterior to the fourchette, stretches to accommodate fetal head passage during childbirth.
-
Hymen: a thin, elastic membrane covering the vaginal opening during childhood. Often torn during first sexual intercourse.
Blood and Nerve Supply
-
Vulvar blood supply is primarily from the pudendal artery and partially from the anterior rectal artery.
-
Vulvar nerve supply is from the ilioinguinal and genitofemoral nerves (L1 level) in the anterior portion and the pudendal nerve (S3 level) in the posterior portion.
-
Extensive venous pressure from the fetal head can lead to varicosities in the labia majora and legs.
Internal Structures
-
Ovaries: almond-shaped organs, responsible for producing and releasing ova, estrogen, and progesterone.
-
Fallopian Tubes: connecting the ovaries to the uterus, responsible for conveying ova and providing a site for fertilization.
-
Uterus: a hollow muscular organ, responsible for receiving ova, providing a site for implantation, nourishing the fetus, and expelling the fetus at maturity.
-
Vagina: a muscular canal leading from the uterus to the outside of the body.
-
Cervix: the lower portion of the uterus, with the central canal, internal cervical os, and external cervical os.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your understanding of unitive and procreative health concepts in human sexuality, specifically focusing on the importance of natural intercourse and intrauterine development. This quiz covers the key principles regarding the moral implications of sexual acts and the biological development from conception to birth.