Podcast
Questions and Answers
The pyramidal lobe of the thyroid gland, when present, is most likely to:
The pyramidal lobe of the thyroid gland, when present, is most likely to:
- Undergo atrophy in response to thyroid-stimulating hormone (TSH) suppression.
- Be easily palpable in healthy adults due to its size and superficial location.
- Remain constant in size, irrespective of the overall functional state of the thyroid gland.
- Enlarge in the presence of thyroid disease, potentially becoming more noticeable. (correct)
Which anatomical structure serves as the superior boundary for defining the location of the thyroid gland?
Which anatomical structure serves as the superior boundary for defining the location of the thyroid gland?
- Cricoid cartilage
- Sternohyoid muscle
- Hyoid bone (correct)
- Cricothyroid membrane
A surgeon is planning to perform a thyroidectomy. Which anatomical landmark is MOST critical for them to identify to ensure precise and safe removal of the thyroid while minimizing the risk of damage to nearby structures?
A surgeon is planning to perform a thyroidectomy. Which anatomical landmark is MOST critical for them to identify to ensure precise and safe removal of the thyroid while minimizing the risk of damage to nearby structures?
- The hyoid bone, as it indicates the superior extent of the surgical field.
- The strap muscles, to guide the initial incision and superficial dissection.
- The carotid sheath, to avoid potential vascular complications.
- The cricoid cartilage, because the thyroid isthmus is located immediately above it. (correct)
A patient presents with an enlarged thyroid gland extending superiorly towards the hyoid bone. Which statement best describes the anatomical relationship?
A patient presents with an enlarged thyroid gland extending superiorly towards the hyoid bone. Which statement best describes the anatomical relationship?
During a physical examination, a medical student palpates a structure in the anterior neck, immediately below the thyroid cartilage. Deep to the strap muscles. Which of the following is MOST likely to be the structure that the student is palpating?
During a physical examination, a medical student palpates a structure in the anterior neck, immediately below the thyroid cartilage. Deep to the strap muscles. Which of the following is MOST likely to be the structure that the student is palpating?
How does the thyroid hormone receptor (TR) complex initiate transcription upon binding to the thyroid response element (TRE) on DNA?
How does the thyroid hormone receptor (TR) complex initiate transcription upon binding to the thyroid response element (TRE) on DNA?
Which metabolic effect is NOT typically associated with thyroid hormone ($T_3$) stimulation?
Which metabolic effect is NOT typically associated with thyroid hormone ($T_3$) stimulation?
Which of the following scenarios would result in decreased thyroid hormone synthesis due to direct impact on iodide trapping?
Which of the following scenarios would result in decreased thyroid hormone synthesis due to direct impact on iodide trapping?
An individual with hyperthyroidism is likely to exhibit which of the following lipid profiles?
An individual with hyperthyroidism is likely to exhibit which of the following lipid profiles?
A patient with Pendred syndrome is likely to exhibit which of the following hormonal imbalances as a direct consequence of the affected protein's function?
A patient with Pendred syndrome is likely to exhibit which of the following hormonal imbalances as a direct consequence of the affected protein's function?
How does thyroid hormone influence the cardiovascular system at slightly elevated levels?
How does thyroid hormone influence the cardiovascular system at slightly elevated levels?
What is the combined effect of thyroid hormone and catecholamines on heart rate?
What is the combined effect of thyroid hormone and catecholamines on heart rate?
What is the immediate consequence if thyroid peroxidase (TPO) is completely inhibited in thyroid hormone synthesis?
What is the immediate consequence if thyroid peroxidase (TPO) is completely inhibited in thyroid hormone synthesis?
Which of the following is a direct substrate of thyroid peroxidase (TPO) during the organification of iodine in thyroglobulin?
Which of the following is a direct substrate of thyroid peroxidase (TPO) during the organification of iodine in thyroglobulin?
A novel drug is designed to specifically enhance the activity of the sodium-iodide symporter (NIS) in thyroid follicular cells. What downstream effect would be expected from this drug?
A novel drug is designed to specifically enhance the activity of the sodium-iodide symporter (NIS) in thyroid follicular cells. What downstream effect would be expected from this drug?
Why is T4 considered a prohormone for T3?
Why is T4 considered a prohormone for T3?
Considering the properties of thyroid hormones, what is the most likely reason they require carrier proteins in the bloodstream?
Considering the properties of thyroid hormones, what is the most likely reason they require carrier proteins in the bloodstream?
Which of the following statements accurately compares the characteristics of T3 and T4?
Which of the following statements accurately compares the characteristics of T3 and T4?
How does the proteolysis of thyroglobulin contribute to thyroid hormone production?
How does the proteolysis of thyroglobulin contribute to thyroid hormone production?
A patient has a genetic defect resulting in a complete absence of transthyretin (TBPA). How would this condition most likely affect thyroid hormone levels in the blood?
A patient has a genetic defect resulting in a complete absence of transthyretin (TBPA). How would this condition most likely affect thyroid hormone levels in the blood?
A thyroglossal duct cyst is clinically apparent when the thyroglossal duct fails to undergo which of the following processes during embryonic development?
A thyroglossal duct cyst is clinically apparent when the thyroglossal duct fails to undergo which of the following processes during embryonic development?
At what gestational age does the thyroid gland reach its final location anterior to the trachea?
At what gestational age does the thyroid gland reach its final location anterior to the trachea?
Ectopic thyroid tissue along the path of the thyroglossal duct is most likely to be found in which of the following locations?
Ectopic thyroid tissue along the path of the thyroglossal duct is most likely to be found in which of the following locations?
A 4-year-old girl presents with slowed growth. Lab results show elevated TSH and low T4 levels. This is most indicative of a defect in which of the following?
A 4-year-old girl presents with slowed growth. Lab results show elevated TSH and low T4 levels. This is most indicative of a defect in which of the following?
What are the two main components required for the synthesis of thyroid hormones (T3 and T4)?
What are the two main components required for the synthesis of thyroid hormones (T3 and T4)?
Why is 'reverse T3' (rT3) considered biologically inactive?
Why is 'reverse T3' (rT3) considered biologically inactive?
During thyroid gland embryogenesis, what structure connects the developing thyroid to the tongue, and along which ectopic thyroid tissue may arise?
During thyroid gland embryogenesis, what structure connects the developing thyroid to the tongue, and along which ectopic thyroid tissue may arise?
If the thyroid gland does not descend properly during development, which of the following is least likely to occur?
If the thyroid gland does not descend properly during development, which of the following is least likely to occur?
Which statement accurately describes the role of T4 deiodination in thyroid hormone activity?
Which statement accurately describes the role of T4 deiodination in thyroid hormone activity?
How does the cell regulate thyroid hormone activity when sufficient T3 is present?
How does the cell regulate thyroid hormone activity when sufficient T3 is present?
What is the primary mechanism by which increased levels of thyroid hormones affect TSH release from the pituitary gland?
What is the primary mechanism by which increased levels of thyroid hormones affect TSH release from the pituitary gland?
Iodine deficiency can lead to goiter. What is the mechanism?
Iodine deficiency can lead to goiter. What is the mechanism?
Which intracellular event directly mediates the thyroid cell's response to TSH stimulation?
Which intracellular event directly mediates the thyroid cell's response to TSH stimulation?
What is the most important factor in the synthesis of thyroid hormones?
What is the most important factor in the synthesis of thyroid hormones?
Which of the following is NOT a direct effect of thyroid stimulating hormone (TSH) on the thyroid gland:
Which of the following is NOT a direct effect of thyroid stimulating hormone (TSH) on the thyroid gland:
Which of the following processes is increased as a result of thyroid response to TSH:
Which of the following processes is increased as a result of thyroid response to TSH:
What is the role of RXR (retinoid X receptor) in the mechanism of action of thyroid hormone?
What is the role of RXR (retinoid X receptor) in the mechanism of action of thyroid hormone?
How the secretion of TSH is characterized?
How the secretion of TSH is characterized?
Flashcards
Thyroid Gland Location
Thyroid Gland Location
Located below the thyroid cartilage and behind strap muscles.
Thyroid Gland Structure
Thyroid Gland Structure
Comprises two lobes joined by an isthmus; can have a pyramidal lobe.
Isthmus of Thyroid
Isthmus of Thyroid
The narrow band connecting the two lobes of the thyroid gland.
Pyramidal Lobe
Pyramidal Lobe
Signup and view all the flashcards
Thyroid Cartilage
Thyroid Cartilage
Signup and view all the flashcards
Iodide Trapping
Iodide Trapping
Signup and view all the flashcards
Pendrin
Pendrin
Signup and view all the flashcards
Pendred Syndrome
Pendred Syndrome
Signup and view all the flashcards
Thyroid Peroxidase (TPO)
Thyroid Peroxidase (TPO)
Signup and view all the flashcards
Monoiodinated Tyrosine (MIT)
Monoiodinated Tyrosine (MIT)
Signup and view all the flashcards
Thyroglossal duct cyst
Thyroglossal duct cyst
Signup and view all the flashcards
Ectopic thyroid tissue
Ectopic thyroid tissue
Signup and view all the flashcards
Thyroid hormone synthesis
Thyroid hormone synthesis
Signup and view all the flashcards
Reverse T3 (rT3)
Reverse T3 (rT3)
Signup and view all the flashcards
Thyroglobulin
Thyroglobulin
Signup and view all the flashcards
Thyroid gland development
Thyroid gland development
Signup and view all the flashcards
Thyroid function tests
Thyroid function tests
Signup and view all the flashcards
Midline cystic masses
Midline cystic masses
Signup and view all the flashcards
T4 to T3 Conversion
T4 to T3 Conversion
Signup and view all the flashcards
Deiodinase Enzymes
Deiodinase Enzymes
Signup and view all the flashcards
Circulating T3 Sources
Circulating T3 Sources
Signup and view all the flashcards
rT3 Production
rT3 Production
Signup and view all the flashcards
Prohormone Role of T4
Prohormone Role of T4
Signup and view all the flashcards
Thyroid Regulation Mechanism
Thyroid Regulation Mechanism
Signup and view all the flashcards
TSH Function
TSH Function
Signup and view all the flashcards
Hypothalamic Control of TSH
Hypothalamic Control of TSH
Signup and view all the flashcards
Impact of Thyroid Hormones on TSH
Impact of Thyroid Hormones on TSH
Signup and view all the flashcards
Thyroid Hormone Mechanism of Action
Thyroid Hormone Mechanism of Action
Signup and view all the flashcards
Thyroid Hormone Action
Thyroid Hormone Action
Signup and view all the flashcards
Metabolic Effects of T3
Metabolic Effects of T3
Signup and view all the flashcards
Effects on Mitochondria
Effects on Mitochondria
Signup and view all the flashcards
Systemic Cardiovascular Effects
Systemic Cardiovascular Effects
Signup and view all the flashcards
Na+/K+ ATPase Function
Na+/K+ ATPase Function
Signup and view all the flashcards
Proteolysis of Thyroid Hormones
Proteolysis of Thyroid Hormones
Signup and view all the flashcards
Carrier Proteins for Thyroid Hormones
Carrier Proteins for Thyroid Hormones
Signup and view all the flashcards
Serum Binding Proteins
Serum Binding Proteins
Signup and view all the flashcards
Biological Activity of T3 and T4
Biological Activity of T3 and T4
Signup and view all the flashcards
Half-life of Thyroid Hormones
Half-life of Thyroid Hormones
Signup and view all the flashcards
Study Notes
Thyroid Hormone Synthesis, Transport, and Cellular Mechanism
- Learning Outcomes:
- Describe the structure and location of the thyroid
- Describe the origin of the thyroid gland and its functional relationships
- Explain the mechanisms and control of thyroid hormone synthesis
- Outline the biochemical and clinical functions of thyroid hormones
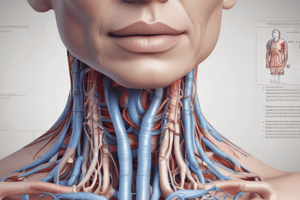
Thyroid Gland: Location and Structure
- Location: Situated below the thyroid cartilage, behind the strap muscles.
- Structure: Comprises two lobes joined by an isthmus, located below the cricoid cartilage.
- Additional finding: Pyramidal lobe in approximately 50% of adults; non-palpable; enlarges with disease.
Thyroid Gland & Follicles
- Functional unit: Thyroid follicle or acinus
- Follicle components: Follicular (epithelial) cells and a lumen filled with colloid.
- Capillaries: Deliver nutrients and transport hormones
- Sympathetic Innervation: Influences hormone synthesis/secretion
- Lymphatics: Drain excess fluid
- C-Cells (Parafollicular Cells): Produce calcitonin
Thyroid Gland: Blood Supply & Innervation
- Arterial Supply:
- Superior thyroid artery (from external carotid)
- Inferior thyroid artery (from thyrocervical trunk)
- Venous Drainage:
- Superior and middle thyroid veins
- Inferior thyroid vein → internal jugular vein
- Brachiocephalic vein
- Innervation:
- Recurrent laryngeal nerve (branch of vagus)
- Damage to the recurrent laryngeal nerve may cause vocal cord paralysis
- Emergency Airway: Cricothyrotomy through the cricothyroid membrane.
Thyroid Gland Origin - Embryology
- The thyroid is the first endocrine gland to develop, appearing around the 24th day of gestation (3rd week of gestation).
- Origin: From the first pharyngeal arch's thyroglossal duct, a diverticulum that arises in the floor of the pharynx.
- Descent and Development: Grows and descends in the neck as an initially hollow structure, eventually solidifying and becoming bilobed with an isthmus.
- Initial descent: Initially anterior to the pharyngeal gut, still connected to the tongue by a thyroglossal duct; eventually bifurcates into two lobes
Thyroid Gland Origin - Embryology (Continuing)
- 7th week: As the gland descends, it takes on its mature shape, positioned anterior to the trachea.
- Complete Obliteration: The thyroglossal duct completely obliterates by 7-10 weeks.
- Remnants: Remnants of the duct may persist.
- Ectopic thyroid tissue: Can arise along this path.
Ectopic Thyroid Gland
- Example: A 4-year-old girl with slowed growth.
- Possible causes: Thyrotropin (TSH) 55 ulU/ml (nl 0.5-4.5), Total Throxine (T4) 3.5 mcg/dl (nl 5-12)
Thyroid Hormone: An Overview
- Synthesis: Thyroid hormones (T3 and T4) are synthesized from iodide (I) and tyrosine residues of thyroglobulin
- 'Reverse T3' (rT3): May be found in significant amounts; biologically inactive.
What Is Thyroid Hormone?
- Critical function: For brain development, skeletal function, and growth in infants
- Metabolic regulation: Regulates metabolic activity in all tissues except brain, spleen, and testes
- Basal metabolic rate and oxygen consumption: Increases these via Na+-K+ ATPase stimulation
- Tissue function: Affects virtually all tissues.
Thyroid Hormone Synthesis - Building Blocks
- Components: Iodine, thyroglobulin, tyrosine
Iodine
- Micronutrient: Crucial for thyroid hormone synthesis
- Dietary sources: Seafood, dairy products, grains, and vegetables grown in iodine-rich soil.
Recommended Daily Intake (IOM) - Iodine
- Kids: About 90-130 mcg
- Adults: About 150 mcg
- Pregnant women: 220 mcg
- Lactating women: 290 mcg
Endemic Goiter
- Cause: Deficiency of iodine in the soil leads to hypothyroidism, with the thyroid gland enlarging (forming a goiter) to produce more thyroid hormone.
- Prevention: Worldwide, table salt (NaCl) is enriched with iodine (iodized salt).
Cretinism in Endemic Severe Iodine Deficiency
- Fetal and postnatal development: Thyroid hormone is vital for fetal and postnatal brain and skeletal development.
- Iodine deficiency during pregnancy and infancy can result in coarse facial features, umbilical hernia, large fontanelles, macroglossia, etc.
- Consequences: Continued iodine deficiency postnatally leads to stunted physical and cognitive/neurologic development.
Thyroid Hormone Synthesis-Building Blocks (Continuing)
- Thyroglobulin: A large glycoprotein, created by the rough ER of thyroid follicular epithelial cells; stored in vesicles and exocytosed into colloid
- Composed of two subunits, containing tyrosine residues sterically oriented for thyroid hormone production
Synthesis of Thyroid Hormones
- Steps: Iodine trapping, oxidation/organification, coupling, endocytosis, proteolysis, transport, action on receptors
Synthesis of Thyroid Hormones (details)
- Iodide trapping: Active transport across the basal membrane of follicular cells against a gradient, involving a sodium-iodide symporter (Na+/K+ ATPase). Stimulated by TSH. Perchlorate anions (CIO4) inhibit uptake.
- Oxidation:Conversion of I− to I2, essential for its incorporation into thyroglobulin, catalyzed by thyroid peroxidase (TPO), requires H2O2
Synthesis of Thyroid Hormones (details 2)
- Coupling: Formation of T4 and T3, through the combination of MIT and DIT molecules within thyroglobulin,catalyzed by TPO
- Endocytosis: Colloid uptake by follicular cells.
- Proteolysis: Lysosomal proteases digest thyroglobulin, releasing free T3 and T4
Transport of Thyroid Hormones
- Hydrophobic nature: Thyroid hormones are hydrophobic and require carrier proteins to be transported in the bloodstream.
- Binding proteins. T4 binds more tightly to three significant serum binding proteins (TBG>TBPA>albumin)
Thyroid Hormone Circulates Bound to Serum Proteins
- Majority bound: T4 and T3 are primarily bound to serum proteins (>99%).
- Free hormone: A small percentage of T4 (0.04%) and T3 (0.5%) is unbound and biologically active.
Conversion of Iodothyronines
- T4 to T3: Peripheral tissues, particularly the liver and kidneys, convert T4 to T3 through deiodination.
- Biological activity T3: T3 is considerably more bio-active than T4.
- Half-life: T4 has a longer half-life than T3.
- Prohormone: T4 is a prohormone for T3.
Thyroid is Under Hypothalamic/Pituitary Control - Negative Feedback Loop
- Hypothalamic-pituitary-thyroid axis: A negative feedback loop involving TRH, TSH, and thyroid hormones.
- Regulation: Thyroid hormone levels regulate the release of TRH and TSH.
Regulation of Thyroid Hormone Synthesis
- Factors: Hypothalamus (TRH), Anterior pituitary gland (TSH), Availability of iodine, Thyroid gland integrity, Tissue conversion (T4 to T3).
Thyroid Stimulating Hormone (TSH)
- Glycoprotein: Created in the anterior pituitary, with slight increased levels at night.
- Effects: Stimulates thyroid hormone synthesis and increases thyroid gland size/vascularity.
- Feedback: Increased thyroid hormone levels decrease TSH release. Decreased levels increase TSH release; Crucial for iodine deficiency goiter.
Thyroid Response to TSH
- Effects: Increased cAMP, Ca2 +, protein kinase activity, colloid uptake, T3 and T4 liberation, thyroglobulin production, iodine uptake, thyroglobulin iodination. Thyroid size and activity increase.
Inhibitors of Thyroid Hormone Synthesis
- Inhibitors: Drugs and goitrogens. These substances hinder steps in thyroid hormone synthesis
Biochemical and Clinical Functions of Thyroid Hormones (Mechanism of Action)
- Mechanism: T4 converts to T3, binds to thyroid receptor, complexes with RXR, and binds to the thyroid response element in DNA. Protein synthesis then mediates the cellular responses.
Effects-Metabolic
- Carbohydrate metabolism effects: Increased glucose uptake, enhanced glycolysis, enhanced gluconeogenesis, and increased insulin secretion.
- Lipid metabolism effects: Increased lipolysis, decrease fatty acid and fat stores, increased B-oxidation, decreased plasma cholesterol phospholipids & TAG levels.
- Other metabolic functions: Increased mitochondria count, Na+/K+ ATPase activity, 02 consumption, and protein synthesis, and an increase in the metabolic rate.
Effects-Systemic
- Cardiovascular effects: Increased blood flow, cardiac output, heart rate, and heart strength.
- Respiratory effects: Increased respiration.
- Central nervous system effects: Essential for normal CNS neuronal development, enhances wakefulness, alertness, memory, learning, and emotional tone; increases speed/amplitude of peripheral nerve reflexes.
Effects-Growth & Development
- Growth effects: Growth and maturation of bone, teeth, and skin; increase in hair, follicles, and nails.
- Skeletal muscle: Increased rate and force of skeletal muscle contraction, and fetal CNS development.
- General child growth.
Summary of Actions
- Development: Inhibits nerve cell replication, enhances nerve cell body growth, branches of dendrites, and axon myelinization rate.
- Body Growth: Stimulates gene expression for growth hormone, increased structural and enzymatic protein synthesis, and bone calcification.
- Basal Energy: Regulates basal metabolic rates of oxidative phosphorylation, body heat production, and O2 consumption ("thermogenic effect")
- Metabolism: Stimulates the synthesis and degradation pathways of carbohydrates, lipids, and proteins
- TSH secretion: Inhibits TSH secretion by decreasing sensitivity of thyrotrophs to TRH.
Tests of Thyroid Function
- Thyroid Stimulating Hormone (TSH): Measures pituitary secretion of TSH in response to T4 feedback. Normal range = 0.5 – 4.5mU/L
- Free Thyroxine (FT4): Measures unbound T4. Normal range = 0.8 – 1.8ng/dL
- Free Triiodothyronine (FT3): Measures unbound T3. Normal range = 2.3 – 4.2pg/mL
- Total Thyroxine (T4): Measures bound plus free T4. Normal range = 5–12mcg/dL
- Total Triiodothyronine (T3): Measures bound plus free T3. Normal range = 60–180ng/dL
Log-Linear Inverse Relationship between TSH and T4
- Wide variation in individual "set points"
- Specific TSH:T4 set-point for each individual.
TSH Assay as Screening Test
- Optimal screening test for ambulatory healthy patients. Low TSH (<0.5 mU/L) suggests hyperthyroidism. Normal TSH (0.5–4.5 mU/L) means euthyroidism. High TSH (>4.5 mU/L) suggests hypothyroidism.
Thyroid Disorders (TSH, T4, T3, FT4)
- Primary hypothyroidism: Elevated TSH, decreased T4, T3, and FT4.
- Graves' Disease: Increased TSH, decreased T4 and T3, and increased FT4 and FT3.
- TSH deficiency (secondary hypothyroidism): Decreased TSH causing decreased T4 and T3.
MCQ (Multiple Choice Questions)
- MCQ 1 (Iodine activation): Thyroid peroxidase (TPO).
- MCQ 2 (Primary hypothyroidism): High TRH, high TSH, low T4.
Case Presentations
- Case presentations highlight clinical conditions and associated laboratory findings. Examples include primary hyperthyroidism in a 46-year-old woman, with elevated total/free T4 and suppressed TSH, presenting with weight loss and diarrhea;
- Case presentation for Primary Hypothyroidism, in a 72 year old man, presenting with decreased total/free T4 and elevated TSH, and vague symptoms/ reduced cognition. .
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the anatomy and function of the thyroid gland, including the pyramidal lobe, anatomical boundaries, and surgical considerations during thyroidectomy. Also covers the thyroid hormone receptor (TR) complex and its role in initiating transcription.