Podcast
Questions and Answers
Where is the thyroid gland located?
Where is the thyroid gland located?
- Below the thyroid cartilage (correct)
- Above the hyoid bone
- In front of the cricoid cartilage
- Beside the carotid arteries
What are the structural components of the thyroid gland?
What are the structural components of the thyroid gland?
- Two separate lobes with no connection
- Two lobes joined by an isthmus (correct)
- Four lobes each connected by a duct
- A single lobe and a non-palpable segment
What could happen to the pyramidal lobe of the thyroid gland?
What could happen to the pyramidal lobe of the thyroid gland?
- It is removed during thyroid surgery
- It may enlarge with disease (correct)
- It always remains prominent
- It is present in all adults
Which cartilage structure is directly located above the thyroid gland?
Which cartilage structure is directly located above the thyroid gland?
What is the significance of the isthmus in the thyroid gland?
What is the significance of the isthmus in the thyroid gland?
What role does the sodium-iodide symporter (NIS) play in iodide trapping?
What role does the sodium-iodide symporter (NIS) play in iodide trapping?
Which statement about Pendrin is true?
Which statement about Pendrin is true?
What is the effect of TSH on iodide trapping in thyroid cells?
What is the effect of TSH on iodide trapping in thyroid cells?
Which of the following substances serves as an inhibitor of iodide uptake?
Which of the following substances serves as an inhibitor of iodide uptake?
What process converts iodide (I-) to iodine (I2)?
What process converts iodide (I-) to iodine (I2)?
What role does increased gluconeogenesis play in excess conditions?
What role does increased gluconeogenesis play in excess conditions?
Which physiological system is critical for normal CNS neuronal development?
Which physiological system is critical for normal CNS neuronal development?
How does growth hormone affect skeletal muscle contraction?
How does growth hormone affect skeletal muscle contraction?
What is one of the specific actions of growth hormone regarding bone development?
What is one of the specific actions of growth hormone regarding bone development?
Which of the following is NOT a characteristic effect of growth hormone on the body?
Which of the following is NOT a characteristic effect of growth hormone on the body?
What is the role of the thyroid hormone receptor in the context of gene expression?
What is the role of the thyroid hormone receptor in the context of gene expression?
Which of the following is NOT a metabolic effect of the thyroid hormone?
Which of the following is NOT a metabolic effect of the thyroid hormone?
How does thyroid hormone influence the cardiovascular system?
How does thyroid hormone influence the cardiovascular system?
Which process is NOT stimulated by thyroid hormones in the context of fat metabolism?
Which process is NOT stimulated by thyroid hormones in the context of fat metabolism?
What is one of the systemic effects of thyroid hormone associated with increased metabolic activity?
What is one of the systemic effects of thyroid hormone associated with increased metabolic activity?
What is the primary functional unit of the thyroid gland?
What is the primary functional unit of the thyroid gland?
Which type of cells within the thyroid gland are responsible for producing calcitonin?
Which type of cells within the thyroid gland are responsible for producing calcitonin?
From which arteries does the arterial supply for the thyroid gland primarily originate?
From which arteries does the arterial supply for the thyroid gland primarily originate?
What role do capillaries play in the thyroid gland?
What role do capillaries play in the thyroid gland?
At which stage of gestation does the thyroid gland first begin to develop?
At which stage of gestation does the thyroid gland first begin to develop?
What structure connects the thyroid gland to the tongue during its development?
What structure connects the thyroid gland to the tongue during its development?
What potential complication may arise from damage to the recurrent laryngeal nerve?
What potential complication may arise from damage to the recurrent laryngeal nerve?
Which of the following nerves is primarily responsible for the innervation of the thyroid gland?
Which of the following nerves is primarily responsible for the innervation of the thyroid gland?
What is the primary form of thyroid hormone found in circulation?
What is the primary form of thyroid hormone found in circulation?
Which enzyme is responsible for converting T4 to the inactive form rT3?
Which enzyme is responsible for converting T4 to the inactive form rT3?
How does T3 influence TSH secretion from the pituitary gland?
How does T3 influence TSH secretion from the pituitary gland?
What is the role of TRH in thyroid hormone regulation?
What is the role of TRH in thyroid hormone regulation?
What happens when the body has sufficient T3 levels?
What happens when the body has sufficient T3 levels?
Which of the following is a direct effect of TSH on the thyroid gland?
Which of the following is a direct effect of TSH on the thyroid gland?
What are the conditions under which TSH levels would increase?
What are the conditions under which TSH levels would increase?
Which factor does NOT affect the synthesis of thyroid hormones?
Which factor does NOT affect the synthesis of thyroid hormones?
What defines T4's role as a prohormone?
What defines T4's role as a prohormone?
What is the consequence of excessive TSH levels?
What is the consequence of excessive TSH levels?
Flashcards
Location of the thyroid gland
Location of the thyroid gland
The thyroid gland is situated below the thyroid cartilage, behind the strap muscles. It comprises two lobes joined by an isthmus, located below the cricoid cartilage.
Structure of the thyroid gland
Structure of the thyroid gland
The thyroid gland is made up of two lobes connected by an isthmus. Approximately 50% of adults also have a pyramidal lobe which is usually not palpable, but may enlarge in cases of thyroid disease.
What is the thyroid cartilage?
What is the thyroid cartilage?
The thyroid cartilage is a structure in the neck that gives the neck its shape, located above the thyroid gland.
What is the cricoid cartilage?
What is the cricoid cartilage?
Signup and view all the flashcards
What are the strap muscles?
What are the strap muscles?
Signup and view all the flashcards
Thyroid follicle
Thyroid follicle
Signup and view all the flashcards
Lumen of thyroid follicle
Lumen of thyroid follicle
Signup and view all the flashcards
Follicular cells
Follicular cells
Signup and view all the flashcards
Thyroglobulin
Thyroglobulin
Signup and view all the flashcards
Thyroglossal duct
Thyroglossal duct
Signup and view all the flashcards
Origin of thyroid gland
Origin of thyroid gland
Signup and view all the flashcards
Blood supply to thyroid gland
Blood supply to thyroid gland
Signup and view all the flashcards
Innervation of thyroid gland
Innervation of thyroid gland
Signup and view all the flashcards
Sodium-Iodide Symporter (NIS)
Sodium-Iodide Symporter (NIS)
Signup and view all the flashcards
Thyroid Stimulating Hormone (TSH)
Thyroid Stimulating Hormone (TSH)
Signup and view all the flashcards
Oxidation of Iodide
Oxidation of Iodide
Signup and view all the flashcards
Pendred Syndrome
Pendred Syndrome
Signup and view all the flashcards
How does T3 regulate gene expression?
How does T3 regulate gene expression?
Signup and view all the flashcards
How does T3 impact carbohydrate metabolism?
How does T3 impact carbohydrate metabolism?
Signup and view all the flashcards
What is the effect of T3 on fat metabolism?
What is the effect of T3 on fat metabolism?
Signup and view all the flashcards
How does T3 affect cellular activity?
How does T3 affect cellular activity?
Signup and view all the flashcards
How does T3 influence the cardiovascular system?
How does T3 influence the cardiovascular system?
Signup and view all the flashcards
What is the role of thyroid hormone in brain development?
What is the role of thyroid hormone in brain development?
Signup and view all the flashcards
How does thyroid hormone influence nerve reflexes?
How does thyroid hormone influence nerve reflexes?
Signup and view all the flashcards
How does thyroid hormone promote growth and development?
How does thyroid hormone promote growth and development?
Signup and view all the flashcards
How does thyroid hormone affect energy metabolism?
How does thyroid hormone affect energy metabolism?
Signup and view all the flashcards
What is the role of thyroid hormone in intermediary metabolism?
What is the role of thyroid hormone in intermediary metabolism?
Signup and view all the flashcards
How is T3 produced?
How is T3 produced?
Signup and view all the flashcards
What is the role of T3?
What is the role of T3?
Signup and view all the flashcards
What is the role of reverse T3 (rT3)?
What is the role of reverse T3 (rT3)?
Signup and view all the flashcards
How is thyroid hormone production regulated?
How is thyroid hormone production regulated?
Signup and view all the flashcards
What is the role of TRH and TSH in thyroid regulation?
What is the role of TRH and TSH in thyroid regulation?
Signup and view all the flashcards
What are the functions of TSH?
What are the functions of TSH?
Signup and view all the flashcards
How is TSH secretion regulated?
How is TSH secretion regulated?
Signup and view all the flashcards
What are the effects of TSH on the thyroid gland?
What are the effects of TSH on the thyroid gland?
Signup and view all the flashcards
What are goitrogens and how do they affect thyroid hormone synthesis?
What are goitrogens and how do they affect thyroid hormone synthesis?
Signup and view all the flashcards
How do thyroid hormones exert their effects at the cellular level?
How do thyroid hormones exert their effects at the cellular level?
Signup and view all the flashcards
Study Notes
Thyroid Hormone Synthesis, Transport and Cellular Mechanism
- The thyroid gland is located below the thyroid cartilage, behind the strap muscles.
- It consists of two lobes connected by an isthmus, situated below the cricoid cartilage.
- A pyramidal lobe is present in about 50% of adults; it's not usually palpable and can enlarge with disease.
Learning Outcomes
- Describe the structure and location of the thyroid gland.
- Describe the origin of the thyroid gland and its functional relationships.
- Explain the mechanisms and control of thyroid hormone synthesis.
- Outline the biochemical and clinical functions of thyroid hormones.
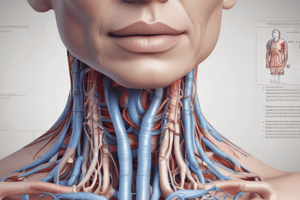
Thyroid Gland: Location and Structure
- The thyroid gland is situated below the thyroid cartilage.
- The thyroid gland comprises two lobes connected by an isthmus.
- The isthmus of the thyroid gland is located below the cricoid cartilage.
- A pyramidal lobe is present in ~50% of adults.
- It is not usually palpable.
- It can enlarge with disease.
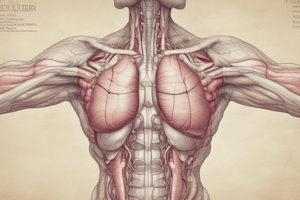
Thyroid Gland & Follicles
- The functional unit of the thyroid gland is the thyroid follicle or acinus.
- Thyroid follicles consist of follicular epithelial cells and a lumen filled with colloid.
- Capillaries deliver nutrients and transport hormones.
- The sympathetic nervous system influences hormone synthesis and secretion.
- Lymphatic vessels drain excess fluid.
- Parafollicular cells (C-cells) produce calcitonin.
Thyroid Gland: Blood Supply & Innervation
-
Arterial Supply:
- Superior thyroid artery (from external carotid)
- Inferior thyroid artery (from thyrocervical trunk)
-
Venous Drainage:
- Superior and middle thyroid veins (drain into the internal jugular vein)
- Inferior thyroid vein (drains into the brachiocephalic vein)
-
Innervation:
- Recurrent laryngeal nerve (branch of vagus)
- Damage to this nerve can cause vocal cord paralysis.
- The cricothyroid membrane can be used for emergency cricothyrotomy.
Thyroid Gland Origin - Embryology
- The thyroid is the first endocrine gland to develop (around the 24th day of gestation).
- It originates from the first pharyngeal arch.
- The thyroid precursor develops from the thyroglossal duct.
- This duct is a diverticulum appearing in the floor of the pharynx.
- It grows and descends in the neck as an initially hollow structure then solidifies and becomes bilobed, connected by an isthmus.
- The thyroglossal duct breaks down by the late fifth week.
- The initial descent is anterior to the pharyngeal gut; it remains connected to the tongue by the thyroglossal duct before bifurcating into two lobes.
- The thyroid gland is positioned in its final location, anterior to the trachea by the seventh week of gestation.
- The thyroglossal duct obliterates completely by the 7th to 10th week.
- Remnants of the duct may persist.
- Ectopic thyroid tissue can arise along this path.
Ectopic Thyroid Gland
- Ectopic thyroid tissue can arise in abnormal locations along the path that the thyroglossal duct descends.
- An example includes the lingual thyroid.
Thyroid Hormone: An Overview
- Thyroid hormones (T3 and T4) are synthesized from iodine and tyrosine residues of thyroglobulin.
- The synthesis of T3 and T4 need the elements iodine (I) and tyrosine.
- "Reverse T3" (rT3) is not biologically active.
What is Thyroid Hormone?
- Thyroid hormones are critical for brain and skeletal development and growth in infants.
- They regulate metabolic activity in most tissues, except for brain, spleen, and testes.
- Thyroid hormones increase basal metabolic rate and oxygen consumption.
- They increase heat production by stimulating Na+-K+ ATPase.
- They affect the functions of virtually all tissues.
Thyroid Hormone Synthesis - Building Blocks
- Iodine
- Thyroglobulin
- Tyrosine
Iodine
- Iodine is a micronutrient found in seafood, dairy products, and grains & vegetables.
- The recommended daily intake varies based on age and pregnancy status.
- Iodized salt has been crucial in the prevention of iodine deficiency disorders.
Endemic Goiter
- In areas where the soil is deficient in iodine, hypothyroidism is common.
- The thyroid gland enlarges (forms a goiter) to produce more thyroid hormone to compensate for the lack of iodine.
- Worldwide, table salt (NaCl) is enriched with iodine (iodized salt) to prevent iodine deficiency.
Cretinism in Endemic Severe Iodine Deficiency
- Thyroid hormone is essential for fetal and postnatal brain as well as skeletal maturation.
- Iodine deficiency during pregnancy in both the mother and the baby can result in coarse facial features, umbilical hernia, large fontanelles, and macroglossia at birth.
- Continued iodine deficiency after birth can lead to severe growth and cognitive/neurological impairments.
Thyroid Hormone Synthesis - Building Blocks (cont'd)
- Thyroglobulin: large glycoprotein produced by the rough endoplasmic reticulum of thyroid follicular epithelial cells.
- It is stored in vesicles and exocytosed into the colloid.
- Composed of two subunits.
- Contains tyrosine residues sterically oriented for thyroid hormone production.
Synthesis of Thyroid Hormones
- Steps of synthesis include iodide trapping, oxidation/organification, coupling, endocytosis, proteolysis, transport, and action on receptors.
Synthesis of Thyroid Hormones (cont'd): Iodide Trapping
- The basal membrane of thyroid follicular endothelial cells actively transport iodide from the bloodstream against the gradient.
- A sodium-iodide symporter (Na+/K+ ATPase) is involved in this active transport.
- Perchlorate anions are inhibitors of iodide uptake clinically.
- Pendrin transports iodide into the colloid.
Synthesis of Thyroid Hormones (cont'd): Oxidation/Organification
- Iodide (I-) is converted to iodine (I2) with H2O2.
- The enzyme thyroid peroxidase (TPO) catalyzes this process.
- Iodide combines with tyrosine residues of thyroglobulin, also catalyzed by TPO.
- Iodotyrosine products generated are monoiodotyrosine (MIT) and diiodotyrosine (DIT).
Synthesis of Thyroid Hormones (cont'd): Coupling
- MIT and DIT combine to form triiodothyronine (T3) and thyroxine (T4).
- Thyroid peroxidase (TPO) catalyzes this action.
- Iodinated thyroglobulin is stored in the colloid.
- Colloid stores enough thyroglobulin for 2-3 months of thyroid hormone needs.
Secretion of Thyroid Hormones: Endocytosis and Proteolysis
- Colloid is pinocytosed into the follicular cell prior to secretion.
- Lysosomal proteases digest thyroglobulin, releasing T3 and T4.
- MIT and DIT are degraded, and the iodine is re-used.
- T4 and T3 diffuse across the basolateral membrane into capillaries and enter the circulation.
Transport of Thyroid Hormones
- Thyroid hormones are hydrophobic and need carrier proteins (like thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and serum albumin) to travel in the bloodstream.
- T4 binds more strongly to serum binding proteins compared to T3, where only a small percentage circulate freely.
Thyroid Hormone Circulates Bound to Serum Proteins
- Almost all thyroid hormone (T3 and T4) is transported bound to carrier proteins.
- Only a tiny percentage of T3 and T4 circulates freely in the blood.
Conversion of Iodothyronines
- The thyroid gland mainly secretes T4.
- T3 is 2-10 times more biologically active than T4.
- Peripheral tissues (especially the liver and kidneys) convert T4 into more active T3.
- T4 serves as a prohormone to T3 producing it through deiodinase enzymes.
- Various percentages of T3 and T4 production occur from peripheral tissues.
Thyroid is Under Hypothalamic/Pituitary Control (Negative Feedback Loop)
- Hypothalamus releases TRH.
- TRH stimulates the anterior pituitary to release TSH.
- TSH stimulates the thyroid gland to release T3 and T4.
- T3 and T4 exert negative feedback on both the anterior pituitary and the hypothalamus to regulate the production process (reducing further TRH and TSH release).
Regulation of Thyroid Hormone Synthesis
- Factors influencing thyroid hormone synthesis include hypothalamic TRH, somatostatin (SS), anterior pituitary TSH, iodine availability, thyroid gland integrity, and T4 to T3 conversion in tissues.
Thyroid Stimulating Hormone (TSH)
- TSH is a glycoprotein produced in the anterior pituitary.
- It is secreted in pulses, with slightly higher levels at night.
- TSH stimulates thyroid hormone synthesis, leading to increased size and vascularity of the thyroid gland.
- Increased levels of TH negatively feedback on TSH release.
- Conversely, decreased TH levels increase TSH release.
- Iodine deficiency causes goiter.
Thyroid Response to TSH
- TSH causes an increase in cAMP, Ca²⁺, and protein kinase activity.
- Increased uptake of colloid results from increased TSH activity.
- Increased liberation of T3 and T4 occurs.
- Increased production of thyroglobulin is stimulated by TSH.
- Increased uptake of iodine is stimulated.
- Increased iodination of thyroglobulin is stimulated.
- TSH causes increased size and activity of thyroid cells and increased thyroid cell numbers (hypertrophy).
Inhibitors (Drugs and Goitrogens) of Thyroid Hormone Synthesis
- Various substances inhibit various steps of thyroid hormone synthesis.
- Iodine and thyroid peroxidase activity are inhibited.
- Blocking any step in thyroid hormone synthesis can result in various changes in the thyroid functions with relevant clinical consequences.
Tests of Thyroid Function
- Thyroid-stimulating hormone (TSH) measures pituitary's response to T3 and T4 levels.
- Free thyroxine (FT4) measures unbound thyroxine in the blood.
- Free triiodothyronine (FT3) measures unbound triiodothyronine in the blood.
- Total thyroxine (T4) and total triiodothyronine (T3) measure both bound and free hormones in the blood.
Mechanism of Action of Thyroid Hormone
- T4 is converted to T3.
- T3 binds to thyroid receptors (TR) along with retinoid X receptors (RXR).
- The resulting complex binds to the thyroid response element (TRE) on DNA.
- This process regulates transcription of target genes by influencing the expression of various proteins that subsequently affect cellular responses.
Effects - Metabolic
- Thyroid hormones stimulate carbohydrate metabolism (increased glucose uptake, enhanced glycolysis, gluconeogenesis, insulin secretion).
- They stimulate fat metabolism (increased lipolysis, decreased fat stores, increased plasma free fatty acids, increased β-oxidation).
- They affect mitochondrial number, Na+/K+ ATPase activity, oxygen consumption, protein synthesis, and basal metabolic rate (BMR).
- Thyroid hormone levels affect cholesterol, phospholipids and TAG levels in the plasma.
- Increase or decrease in levels of cholesterol are linked to specific conditions that arise from thyroid dysfunction.
Effects - Systemic
- Thyroid hormones increase blood flow and cardiac output, heart rate, and heart strength.
- Thyroid hormones affect the cardiovascular system via their effects on O₂ demand.
- Increase in respiration and enhance wakefulness, alertness, memory, learning, and emotional tone.
- They affect speed and amplitude of peripheral nerve reflexes.
Effects - Growth & Development
- Thyroid hormones stimulate growth and maturation of bone, teeth, epidermis, hair follicles, and nails.
- They increase skeletal muscle contraction rate and force.
- They are essential for fetal central nervous system development.
Summary of Actions
- Thyroid hormones influence central nervous system development and growth including body growth.
- They regulate basal energy economy by influencing metabolic actions.
- They affect intermediary metabolism through carbohydrate, lipid, and protein metabolism.
- Thyroid hormones influence TSH secretion through feedback interactions.
Case Presentations
- Case study examples of primary hyperthyroidism and primary hypothyroidism are presented.
- Test results and symptoms for both conditions are included as examples of case presentations.
MCQ
- Questions related to thyroid hormone function are presented and their correct answers are included.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.