Podcast
Questions and Answers
What is the anatomical relationship between the thyroid gland and the trachea?
What is the anatomical relationship between the thyroid gland and the trachea?
The thyroid gland is anterior to the second to fourth tracheal rings.
What is the function of parafollicular cells in the thyroid gland?
What is the function of parafollicular cells in the thyroid gland?
Parafollicular cells produce calcitonin, which inhibits bone resorption.
What is the role of TSH in the regulation of thyroid hormone synthesis and secretion?
What is the role of TSH in the regulation of thyroid hormone synthesis and secretion?
TSH stimulates thyroid cell growth, iodide uptake, and thyroid hormone synthesis and secretion.
What is the source of T4 and T3 in the body?
What is the source of T4 and T3 in the body?
What is the binding pattern of T4 and T3 in the blood?
What is the binding pattern of T4 and T3 in the blood?
What is the negative feedback mechanism that regulates thyroid hormone synthesis and secretion?
What is the negative feedback mechanism that regulates thyroid hormone synthesis and secretion?
What is the biological significance of free T4 and T3?
What is the biological significance of free T4 and T3?
What is the specific effect of T3 on the cardiovascular system?
What is the specific effect of T3 on the cardiovascular system?
What percentage of the population has nodules identified on ultrasound?
What percentage of the population has nodules identified on ultrasound?
What is the approximate percentage of thyroid nodules that contain malignancy?
What is the approximate percentage of thyroid nodules that contain malignancy?
What is the primary laboratory test used to evaluate a thyroid nodule?
What is the primary laboratory test used to evaluate a thyroid nodule?
What is the purpose of a thyroid scan in evaluating a thyroid nodule?
What is the purpose of a thyroid scan in evaluating a thyroid nodule?
What is the significance of a 'hot' nodule in thyroid evaluation?
What is the significance of a 'hot' nodule in thyroid evaluation?
According to the American Thyroid Association guidelines, how are thyroid nodules classified?
According to the American Thyroid Association guidelines, how are thyroid nodules classified?
What percentage of biopsied nodules have evidence of malignancy?
What percentage of biopsied nodules have evidence of malignancy?
What is the recommended approach for performing thyroid FNAB?
What is the recommended approach for performing thyroid FNAB?
What measurement is indicated for all thyroid nodules and why is it important?
What measurement is indicated for all thyroid nodules and why is it important?
How often should repeat ultrasonography be performed for high-suspicion nodules?
How often should repeat ultrasonography be performed for high-suspicion nodules?
When is repeat FNAB indicated?
When is repeat FNAB indicated?
What is the initial evaluation step for a thyroid nodule?
What is the initial evaluation step for a thyroid nodule?
What is the most common cause of goiter worldwide?
What is the most common cause of goiter worldwide?
What symptoms may indicate compression in patients with goiter?
What symptoms may indicate compression in patients with goiter?
What is the first laboratory step to assess goiter?
What is the first laboratory step to assess goiter?
What is multinodular goiter (MNG)?
What is multinodular goiter (MNG)?
What should patients with goiter be questioned about?
What should patients with goiter be questioned about?
What is the indication for thyroid ultrasonography in patients with goiter?
What is the indication for thyroid ultrasonography in patients with goiter?
What is the most sensitive test of thyroid function and when is it sufficient as an initial test?
What is the most sensitive test of thyroid function and when is it sufficient as an initial test?
What is the difference between hyperthyroidism and thyrotoxicosis?
What is the difference between hyperthyroidism and thyrotoxicosis?
What is the significance of a low TSH and elevated free T4 and/or total T3 in diagnosing thyrotoxicosis?
What is the significance of a low TSH and elevated free T4 and/or total T3 in diagnosing thyrotoxicosis?
What is the purpose of thyroid scintigraphy with RAIU in the diagnosis of hyperthyroidism?
What is the purpose of thyroid scintigraphy with RAIU in the diagnosis of hyperthyroidism?
What is the significance of lid lag in thyrotoxicosis?
What is the significance of lid lag in thyrotoxicosis?
What is the prevalence of hyperthyroidism in the United States?
What is the prevalence of hyperthyroidism in the United States?
What additional test is indicated in patients with suspected substernal extension of the thyroid gland?
What additional test is indicated in patients with suspected substernal extension of the thyroid gland?
Why should administration of iodinated contrast be avoided in thyroid imaging?
Why should administration of iodinated contrast be avoided in thyroid imaging?
What is the most common cause of diffuse goiter in the United States?
What is the most common cause of diffuse goiter in the United States?
When is thyroid surgery considered in patients with diffuse goiter?
When is thyroid surgery considered in patients with diffuse goiter?
What is the incidence rate of thyroid cancer in the United States?
What is the incidence rate of thyroid cancer in the United States?
What type of thyroid carcinoma commonly spreads to cervical lymph nodes?
What type of thyroid carcinoma commonly spreads to cervical lymph nodes?
What is a risk factor for thyroid cancer?
What is a risk factor for thyroid cancer?
What is the mainstay of thyroid cancer treatment?
What is the mainstay of thyroid cancer treatment?
What is the diagnostic test of choice for thyroid cancer?
What is the diagnostic test of choice for thyroid cancer?
What is a symptom that suggests malignancy in a thyroid nodule?
What is a symptom that suggests malignancy in a thyroid nodule?
When is hemithyroidectomy acceptable for thyroid cancer?
When is hemithyroidectomy acceptable for thyroid cancer?
What is a potential risk of thyroid surgery?
What is a potential risk of thyroid surgery?
What is the definition of low-risk PTC?
What is the definition of low-risk PTC?
Why is postoperative 131I considered for thyroid remnant ablation and adjuvant therapy?
Why is postoperative 131I considered for thyroid remnant ablation and adjuvant therapy?
What is the purpose of whole-body scanning after 131I therapy?
What is the purpose of whole-body scanning after 131I therapy?
What is the significance of persistent thyroglobulin (Tg) levels after initial cancer treatment?
What is the significance of persistent thyroglobulin (Tg) levels after initial cancer treatment?
Why is thyroid ultrasonography repeated in routine thyroid cancer surveillance?
Why is thyroid ultrasonography repeated in routine thyroid cancer surveillance?
What is the purpose of TSH suppression with daily levothyroxine in differentiated thyroid cancer treatment?
What is the purpose of TSH suppression with daily levothyroxine in differentiated thyroid cancer treatment?
How is metastatic thyroid cancer managed?
How is metastatic thyroid cancer managed?
What is the characteristic presentation of anaplastic thyroid cancer?
What is the characteristic presentation of anaplastic thyroid cancer?
What is the genetic association with medullary thyroid cancer?
What is the genetic association with medullary thyroid cancer?
What is the primary goal of TSH level management in patients with medullary thyroid cancer?
What is the primary goal of TSH level management in patients with medullary thyroid cancer?
What is the preferred treatment for medullary thyroid cancer?
What is the preferred treatment for medullary thyroid cancer?
Why should MEN be ruled out before surgery in patients with medullary thyroid cancer?
Why should MEN be ruled out before surgery in patients with medullary thyroid cancer?
What laboratory tests are part of routine cancer surveillance in patients with medullary thyroid cancer?
What laboratory tests are part of routine cancer surveillance in patients with medullary thyroid cancer?
What is the most sensitive thyroid function test in patients with normal pituitary function?
What is the most sensitive thyroid function test in patients with normal pituitary function?
What is the significance of a suppressed TSH level in patients with thyroid dysfunction?
What is the significance of a suppressed TSH level in patients with thyroid dysfunction?
What is the effect of biotin supplementation on thyroid function tests?
What is the effect of biotin supplementation on thyroid function tests?
In what settings is measurement of T3 recommended in patients with hyperthyroidism?
In what settings is measurement of T3 recommended in patients with hyperthyroidism?
Why is levothyroxine used in patients with differentiated thyroid cancer?
Why is levothyroxine used in patients with differentiated thyroid cancer?
What is the preferred test for measuring free T4 in patients with thyroid dysfunction?
What is the preferred test for measuring free T4 in patients with thyroid dysfunction?
Flashcards
Thyroid Gland
Thyroid Gland
The thyroid gland, a butterfly-shaped organ located in the neck, produces hormones that regulate metabolism.
Thyroid Hormones
Thyroid Hormones
Thyroxine (T4) and triiodothyronine (T3) are the main hormones produced by the thyroid gland.
Hypothalamic-Pituitary-Thyroid Axis
Hypothalamic-Pituitary-Thyroid Axis
The hypothalamus, pituitary gland, and thyroid gland work together to regulate thyroid hormone production.
TRH and TSH
TRH and TSH
Signup and view all the flashcards
TSH Function
TSH Function
Signup and view all the flashcards
Negative Feedback
Negative Feedback
Signup and view all the flashcards
T4 and T3 Conversion
T4 and T3 Conversion
Signup and view all the flashcards
T3 Action
T3 Action
Signup and view all the flashcards
Thyroid Hormone Effects
Thyroid Hormone Effects
Signup and view all the flashcards
Goiter
Goiter
Signup and view all the flashcards
Multinodular Goiter (MNG)
Multinodular Goiter (MNG)
Signup and view all the flashcards
Thyroid Cancer
Thyroid Cancer
Signup and view all the flashcards
Thyrotoxicosis
Thyrotoxicosis
Signup and view all the flashcards
Hyperthyroidism
Hyperthyroidism
Signup and view all the flashcards
Graves' Disease
Graves' Disease
Signup and view all the flashcards
Hypothyroidism
Hypothyroidism
Signup and view all the flashcards
Hashimoto's Thyroiditis
Hashimoto's Thyroiditis
Signup and view all the flashcards
Thyroid Nodules
Thyroid Nodules
Signup and view all the flashcards
FNAB
FNAB
Signup and view all the flashcards
Serum TSH
Serum TSH
Signup and view all the flashcards
Thyroid Scintigraphy
Thyroid Scintigraphy
Signup and view all the flashcards
Thyroid Ultrasonography
Thyroid Ultrasonography
Signup and view all the flashcards
Radioactive Iodine Therapy
Radioactive Iodine Therapy
Signup and view all the flashcards
Thyroidectomy
Thyroidectomy
Signup and view all the flashcards
Thyroid Hormone Replacement
Thyroid Hormone Replacement
Signup and view all the flashcards
Levothyroxine (Synthroid)
Levothyroxine (Synthroid)
Signup and view all the flashcards
Liothyronine (Cytomel)
Liothyronine (Cytomel)
Signup and view all the flashcards
Liotrix (Thyrolar)
Liotrix (Thyrolar)
Signup and view all the flashcards
Graves' Ophthalmopathy
Graves' Ophthalmopathy
Signup and view all the flashcards
Hashimoto's Thyroiditis
Hashimoto's Thyroiditis
Signup and view all the flashcards
Study Notes
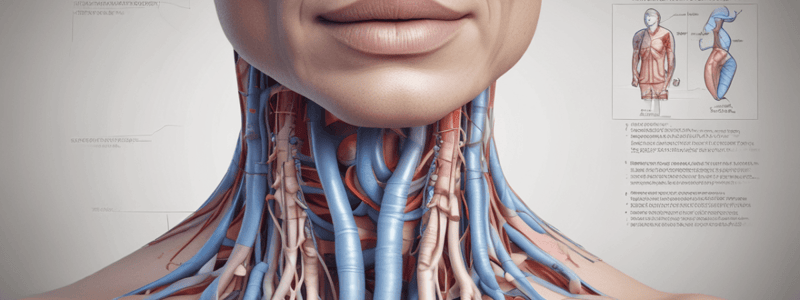
Thyroid Anatomy and Physiology
- The thyroid gland consists of right and left lobes connected by a median isthmus, located in the neck between the sternal notch and thyroid cartilage.
- The parathyroids are located behind the thyroid lobes, with two superior and two inferior parathyroids.
- The recurrent laryngeal nerves course behind the thyroid gland.
- The thyroid gland contains parafollicular cells (C cells) and follicular cells.
- Parafollicular cells produce calcitonin, which inhibits bone resorption and plays a minor role in bone physiology.
- Follicular cells produce thyroid hormones thyroxine (T4) and triiodothyronine (T3).
Thyroid Hormone Regulation
- The hypothalamic-pituitary-thyroid axis regulates thyroid hormone synthesis and secretion.
- Hypothalamic thyrotropin-releasing hormone (TRH) triggers the pulsatile release of thyroid-stimulating hormone (TSH) from the anterior pituitary.
- TSH stimulates thyroid cell growth, iodide uptake, and thyroid hormone synthesis and secretion.
- T4 and T3 exert negative feedback on the hypothalamus and pituitary, which further moderates hormone synthesis.
- The thyroid gland is the exclusive source of T4, while approximately 80% of T3 is from peripheral T4 deiodination, primarily in the liver and kidney.
- Most T4 (99.96%) and T3 (99.6%) are bound to serum proteins, with only free T4 and T3 being biologically available.
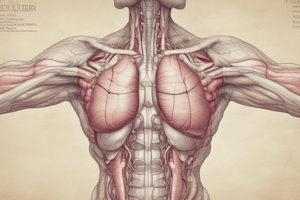
Thyroid Function and Hormone Effects
- T3 binds with high affinity to cellular nuclear receptors, affecting gene transcription in target tissues.
- T3 has positive cardiac inotropic and chronotropic effects, enhances myocardial adrenergic sensitivity, increases myocardial diastolic relaxation, and augments intravascular volume.
- T3 also increases gastrointestinal motility, bone turnover, heat generation, and energy expenditure.
Thyroid Examination
- The thyroid gland is located in the neck between the sternal notch and thyroid cartilage.
- The thyroid gland attaches to the trachea posteriorly and elevates with swallowing and neck extension.
- Examination involves both inspection and palpation while the patient swallows liquid with the neck slightly extended.
Thyroid Nodules
- Palpable nodules are found in 5% of women and 1% of men.
- Approximately 40% of the U.S. population has nodules identified on ultrasound, with an increasing incidence with age.
- Causes of thyroid nodules range from benign cysts and inflammatory nodules to malignancies.
- The initial laboratory evaluation of a thyroid nodule begins with measuring TSH.
- Patients with a suppressed TSH level are evaluated with thyroid scintigraphy, while those with normal or elevated TSH are evaluated with ultrasonography.
- Thyroid nodule characteristics and size determine the need for fine-needle aspiration biopsy (FNAB).
Goiter
- Goiter is an enlarged thyroid gland, which can be associated with normal thyroid function, hypothyroidism, or hyperthyroidism.
- The most common cause of goiter worldwide is iodine deficiency.
- Patients with goiter should be questioned about iodine intake, rate of change in size, and thyroid cancer risk factors.
- Clinical history should focus on symptoms of thyroid hormone excess or deficiency and compression.
- Examination should note the thyroid size, symmetry, and consistency, as well as the presence of nodules or adenopathy and tracheal deviation.
Multinodular Goiter
- Multinodular goiter (MNG) is the most common cause of thyroid enlargement in older adults in the United States.
- Evaluation includes measurement of TSH and thyroid ultrasonography to evaluate discrete nodules.
- The frequency of malignancy in patients with MNG is similar to those with solitary thyroid nodules.
- Signs and symptoms of compression or suspected substernal extension require additional testing, such as CT or MRI of the neck and chest.
Thyroid Cancer
- Thyroid cancer is diagnosed in 13.9 per 100,000 people per year in the United States.
- Thyroid cancer incidence has increased during the past four decades, mainly due to the rise in the diagnosis of small noninvasive cancers.
- Risk factors for thyroid cancer include a history of ionizing radiation exposure and a personal or family history of thyroid cancer.
- The diagnosis is confirmed by FNAB, and surgery is the mainstay of thyroid cancer treatment.
- Postoperative 131I therapy should be considered for thyroid remnant ablation and adjuvant therapy for differentiated thyroid cancer with an intermediate to high risk of recurrence.
Thyroid Function Evaluation
-
Serum TSH is the most sensitive thyroid function test in patients with normal pituitary function.
-
If TSH is suppressed, free T4 and total T3 should be assessed to detect overt or subclinical hyperthyroidism.
-
If TSH is elevated, free T4 should be assessed to detect overt or subclinical hypothyroidism.
-
Measuring TSH alone as an initial test is sufficient except in suspected central hypothyroidism, for which free T4 measurement is preferred.### Thyroid Function Tests
-
Accurate in most clinical settings, but may be inaccurate with significant perturbations (familial dysalbuminemic hyperthyroxinemia)
-
Measuring free T4 by equilibrium dialysis is highly accurate, but expensive and rarely necessary
-
Biotin supplements can interfere with thyroid function tests, causing falsely high free T4, free T3, total T4, and total T3, and falsely low TSH, mimicking thyrotoxicosis
Thyroid Function and Replacement
- Multiple drugs can affect thyroid function and replacement (Table 35)
- Patients taking > 5-10 mg/day of biotin should discontinue it 2-5 days before thyroid function testing
T3 Measurement
- Not necessary in hypothyroidism unless severe, as normal levels are maintained
- Recommended in three settings: evaluating thyrotoxicosis, assessing hyperthyroidism severity, and differentiating hyperthyroidism from destructive thyroiditis
- In T3 toxicosis, the T3-to-T4 ratio is often > 20 due to preferential secretion of T3
Key Points
- Serum TSH is the most sensitive test of thyroid function and is sufficient as an initial test unless central hypothyroidism is suspected
- Triiodothyronine measurement is not necessary in hypothyroidism; normal levels are maintained unless hypothyroidism is severe
Disorders of Thyroid Function
- Thyrotoxicosis describes high levels of circulating thyroid hormones (T4 and T3) from any cause
- Hyperthyroidism is thyrotoxicosis caused by excessive endogenous thyroid hormone production
- Prevalence of hyperthyroidism in the US is 1.3%
Clinical Features and Diagnosis
- Thyrotoxicosis may present with nonclassical symptoms and signs in older adults
- Lid lag (eyelid retraction) can be seen in thyrotoxicosis of any cause due to increased adrenergic tone
- Presence of a diffuse goiter and recently developed proptosis is sufficient for a diagnosis of Graves disease
- Thyrotoxicosis is diagnosed with a low TSH and elevated free T4 and/or total T3
- Thyroid scintigraphy with RAIU can verify the cause
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.