Podcast
Questions and Answers
What is the primary cause of morbidity in rheumatoid arthritis patients?
What is the primary cause of morbidity in rheumatoid arthritis patients?
Which demographic has the highest prevalence of rheumatoid arthritis?
Which demographic has the highest prevalence of rheumatoid arthritis?
What role does the HLA-DR4 antigen play in rheumatoid arthritis?
What role does the HLA-DR4 antigen play in rheumatoid arthritis?
Which of the following is NOT considered an extraarticular manifestation of rheumatoid arthritis?
Which of the following is NOT considered an extraarticular manifestation of rheumatoid arthritis?
Signup and view all the answers
What is a significant factor that can exacerbate rheumatoid arthritis severity?
What is a significant factor that can exacerbate rheumatoid arthritis severity?
Signup and view all the answers
How does age affect the prevalence of rheumatoid arthritis?
How does age affect the prevalence of rheumatoid arthritis?
Signup and view all the answers
What is the estimated reduction in life expectancy for rheumatoid arthritis patients compared to the general population?
What is the estimated reduction in life expectancy for rheumatoid arthritis patients compared to the general population?
Signup and view all the answers
Which statement accurately reflects the genetic predisposition in rheumatoid arthritis?
Which statement accurately reflects the genetic predisposition in rheumatoid arthritis?
Signup and view all the answers
Which of the following joints are typically affected by rheumatoid arthritis (RA)?
Which of the following joints are typically affected by rheumatoid arthritis (RA)?
Signup and view all the answers
What is a key laboratory finding for the diagnosis of rheumatoid arthritis?
What is a key laboratory finding for the diagnosis of rheumatoid arthritis?
Signup and view all the answers
What is the dosing schedule for oral Methotrexate in the treatment of rheumatoid arthritis?
What is the dosing schedule for oral Methotrexate in the treatment of rheumatoid arthritis?
Signup and view all the answers
What is a common adverse effect associated with Leflunomide therapy?
What is a common adverse effect associated with Leflunomide therapy?
Signup and view all the answers
What should be monitored regularly during Methotrexate therapy?
What should be monitored regularly during Methotrexate therapy?
Signup and view all the answers
Which of the following is contraindicated when using Methotrexate?
Which of the following is contraindicated when using Methotrexate?
Signup and view all the answers
Which statement accurately describes Hydroxychloroquine's indications in RA treatment?
Which statement accurately describes Hydroxychloroquine's indications in RA treatment?
Signup and view all the answers
What distinguishes rheumatoid arthritis from other diseases?
What distinguishes rheumatoid arthritis from other diseases?
Signup and view all the answers
Which of the following correctly identifies a potential trigger for autoimmune responses?
Which of the following correctly identifies a potential trigger for autoimmune responses?
Signup and view all the answers
What trend has been observed regarding antinuclear antibodies (ANA) prevalence over the years?
What trend has been observed regarding antinuclear antibodies (ANA) prevalence over the years?
Signup and view all the answers
Which time period showed a notable increase in ANA prevalence, reaching 27 million people?
Which time period showed a notable increase in ANA prevalence, reaching 27 million people?
Signup and view all the answers
What does the rise in the prevalence of ANA suggest about autoimmune diseases?
What does the rise in the prevalence of ANA suggest about autoimmune diseases?
Signup and view all the answers
How is rheumatoid arthritis primarily characterized?
How is rheumatoid arthritis primarily characterized?
Signup and view all the answers
Which of the following best describes the relationship between autoimmune diseases and age according to the data?
Which of the following best describes the relationship between autoimmune diseases and age according to the data?
Signup and view all the answers
What can be inferred about the overall impact of antinuclear antibodies on health?
What can be inferred about the overall impact of antinuclear antibodies on health?
Signup and view all the answers
What is one likely consequence of the increase in rheumatoid arthritis cases?
What is one likely consequence of the increase in rheumatoid arthritis cases?
Signup and view all the answers
Which of the following factors is least likely to be associated with the rising trend of autoimmune diseases?
Which of the following factors is least likely to be associated with the rising trend of autoimmune diseases?
Signup and view all the answers
What condition is characterized by splenomegaly and neutropenia, leading to increased susceptibility to bacterial infections?
What condition is characterized by splenomegaly and neutropenia, leading to increased susceptibility to bacterial infections?
Signup and view all the answers
Which of the following are considered extra-articular involvements in Rheumatoid Arthritis?
Which of the following are considered extra-articular involvements in Rheumatoid Arthritis?
Signup and view all the answers
Which symptom is NOT typically associated with extra-articular involvement in Rheumatoid Arthritis?
Which symptom is NOT typically associated with extra-articular involvement in Rheumatoid Arthritis?
Signup and view all the answers
What is the potential consequence of splenomegaly in patients with Rheumatoid Arthritis?
What is the potential consequence of splenomegaly in patients with Rheumatoid Arthritis?
Signup and view all the answers
Which of the following is a common manifestation of Rheumatoid Arthritis that could lead to a secondary condition?
Which of the following is a common manifestation of Rheumatoid Arthritis that could lead to a secondary condition?
Signup and view all the answers
What type of system involvement is common in Felty Syndrome, associated with Rheumatoid Arthritis?
What type of system involvement is common in Felty Syndrome, associated with Rheumatoid Arthritis?
Signup and view all the answers
Which of the following involves symptoms that may occur due to extra-articular manifestations in Rheumatoid Arthritis?
Which of the following involves symptoms that may occur due to extra-articular manifestations in Rheumatoid Arthritis?
Signup and view all the answers
What does the presence of lymphadenopathy indicate in patients with Rheumatoid Arthritis?
What does the presence of lymphadenopathy indicate in patients with Rheumatoid Arthritis?
Signup and view all the answers
Which pulmonary condition could potentially arise from rheumatoid arthritis?
Which pulmonary condition could potentially arise from rheumatoid arthritis?
Signup and view all the answers
What characteristic suggests a poor prognosis in patients suffering from Rheumatoid Arthritis?
What characteristic suggests a poor prognosis in patients suffering from Rheumatoid Arthritis?
Signup and view all the answers
What is the primary consequence of chronic inflammation in rheumatoid arthritis?
What is the primary consequence of chronic inflammation in rheumatoid arthritis?
Signup and view all the answers
What role do T-cells play in the pathology of rheumatoid arthritis?
What role do T-cells play in the pathology of rheumatoid arthritis?
Signup and view all the answers
Which antibody is primarily produced in most rheumatoid arthritis patients?
Which antibody is primarily produced in most rheumatoid arthritis patients?
Signup and view all the answers
What is the significance of rheumatoid factors in rheumatoid arthritis diagnosis?
What is the significance of rheumatoid factors in rheumatoid arthritis diagnosis?
Signup and view all the answers
In the context of serology, what does a value greater than 60 EU/mL indicate?
In the context of serology, what does a value greater than 60 EU/mL indicate?
Signup and view all the answers
Which of the following agents is NOT primarily released by T-cells and macrophages during inflammation?
Which of the following agents is NOT primarily released by T-cells and macrophages during inflammation?
Signup and view all the answers
What is a potential consequence of the invasion of pannus tissue?
What is a potential consequence of the invasion of pannus tissue?
Signup and view all the answers
What is the role of macrophages in the pathophysiology of rheumatoid arthritis?
What is the role of macrophages in the pathophysiology of rheumatoid arthritis?
Signup and view all the answers
How does the presence of anticitrullinated protein antibody (ACPA) influence prognosis in rheumatoid arthritis?
How does the presence of anticitrullinated protein antibody (ACPA) influence prognosis in rheumatoid arthritis?
Signup and view all the answers
Which inflammatory mediators are specifically categorized as cytokines in rheumatoid arthritis?
Which inflammatory mediators are specifically categorized as cytokines in rheumatoid arthritis?
Signup and view all the answers
Study Notes
Rheumatoid Arthritis (RA)
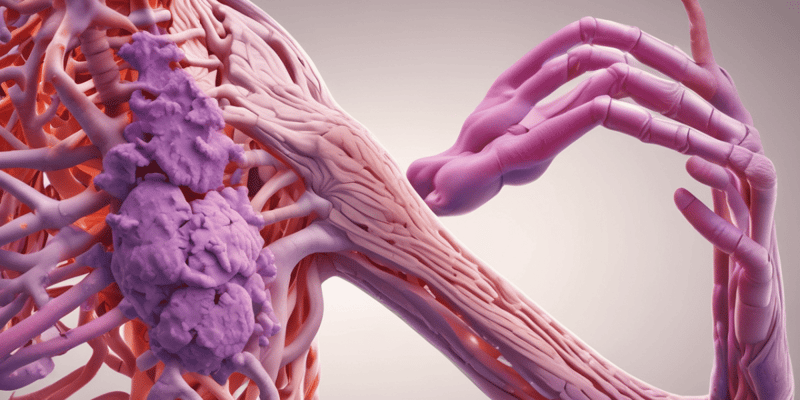
- RA is a chronic, progressive autoimmune disease causing inflammation in joints and other body systems.
- It results in painful deformities and immobility, most commonly affecting fingers, wrists, feet, and ankles.
- RA can affect more than just the joints, also impacting skin, eyes, lungs, heart, and blood vessels.
Objectives of RA Study
- Students will understand epidemiology, pathophysiology, and diagnosis of RA.
- Students understand signs, symptoms, complications, extra-articular manifestations, and treatments of RA.
- Students will learn to select appropriate therapy for individual RA patients, including place in therapy, side effects, and monitoring.
RA Definition
- RA is a chronic, progressive autoimmune disease
- It causes inflammation in joints and other parts of the body, ultimately leading to pain and immobility.
- Deformity and immobility result from the inflammation.
- Usually presents in fingers, wrists, and feet commonly.
Epidemiology
- RA prevalence is 1% worldwide.
- Prevalence rises to age 70.
- RA is three times more prevalent in women than in men (a 6:1 ratio) in the 15-45 age range.
- Cardiovascular disease is the leading cause of death in RA patients.
- RA is a predictor of cardiovascular disease.
- Life expectancy is 3–10 years less than the average.
Genetic Predisposition
- Dizygotic (non-identical) twins and siblings have a 6x higher risk.
- Monozygotic (identical) twins have up to a 30x higher risk.
- HLA-DR4 and HLA-DR1 are antigens associated with a higher RA risk (a 3.5x increase).
Environmental Exposure
- Smoking significantly impacts disease severity.
- Epstein-Barr virus, E. coli, and periodontal disease are infectious mediators potentially contributing to RA.
Pathophysiology
- Synovial inflammation and tissue attacks
- Immune system attacks synovial and other connective tissues.
- Chronic inflammation leads to tissue proliferation, resulting in pannus formation.
- Pannus (abnormal tissue layer) invades cartilage and bone, damaging the joint.
Pathophysiology: Inflammation of the Joint
- Antigen-presenting cells (APCs) present the antigen to T-cells.
- T-cells stimulate B-cells to produce antibodies, and osteoclasts to destroy and remove bone.
- Macrophages promote inflammation, degrade the bone matrix, and produce proinflammatory cytokines.
- TNF-alpha, IL-6, and IL-17 are released by T-cells and macrophages, promoting destruction, increasing blood flow, and increasing cellular invasion.
- Histamine, kinins, and prostaglandins contribute to inflammation.
Pathophysiology: Antibodies
- RA patients may produce antibodies to self-components; these are called rheumatoid factors (RF).
- RF does not indicate the severity of disease.
- Antibodies directed against the Fc portion of Immunoglobulin G (IgG) are also present in RA.
- RF and anti-cyclic citrullinated peptide (anti-CCP) antibodies can aid in diagnosis.
- A negative RF/Anti-CCP does not exclude RA.
Anticitrullinated Protein Antibody (ACPA)
- ACPA is another antibody produced in most RA patients.
- This is observed during various types of inflammation.
- ACPA is diagnosed as an aid but is NOT definitive.
- Can appear before symptoms show an association with poorer prognosis.
Serology
- Normal ACPA values are less than 20 EU/mL (the upper limit of normal).
- 20-39 EU/mL = weakly positive.
- 40-59 EU/mL = moderately positive.
- Greater than 60 EU/mL = strongly positive.
Key Inflammatory Mediators
- Cytokines like TNF, IL-1, and IL-6 are key inflammatory mediators.
- Prostaglandins, leukotrienes, and matrix metalloproteinases also play a role.
Patient Clinical Presentation
- Symptoms include joint pain/stiffness lasting 6 weeks or longer.
- Signs include tenderness, warmth, and swelling in affected joints, particularly in hands and feet.
- Other symptoms including fatigue, weakness, low-grade fever, loss of appetite.
- Possible signs of symmetrical joint involvement and/or rheumatoid nodules.
- Lab tests like RF, anti-CCP, ESR, and CRP often elevated in RA.
- Joint fluid aspiration may reveal increased white blood cell counts, without infection. Presence of crystals in fluid may be observed.
- Joint radiographs may show signs of periarticular osteoporosis, joint space narrowing, and/or erosions.
Extraarticular Involvement
- Rheumatoid nodules: bumps on joints (20% of RA patients), typically located on extensor surfaces of elbows, arms, hands, typically asymptomatic.
- Vasculitis: potentially progress to ulcers, can affect blood vessels, potentially affecting skin, eyes, lungs, heart.
- Eyes: blurred vision can occur.
- Neurological complications.
- Cardiac Involvement
- Pulmonary involvement
- Lymphadenopathy (swollen lymph nodes)
- Splenomegaly (enlarged spleen)
- Felty syndrome: occurs in some patients with RA, characterized by splenomegaly, neutropenia, and an increased susceptibility to bacterial infections.
Joints Affected
- Commonly small joints in hands, feet, and wrists, can potentially expand to larger joints like knees, hips, elbows, and shoulders as inflammation continues.
- Disease is persistent for hours or all day
Diagnosis
- Synovitis (inflammation of a joint) in one joint with no other explanation.
- Positive lab results, including RF, ACPA, CRP, and ESR.
- Duration of symptoms of at least 6 weeks
- Criteria > 6/10 (based on a criteria scale).
Disease Activity Score
- Measures RA disease activity.
- Various scales (like PAS or PASII, RAPID3, CDAI, DAS28) are used.
Prognostic Factors
- Higher tender/swollen joint counts
- Radiographic erosions (bone damage visible on X-ray)
- Elevated RF and anti-CCP Elevated ESR and CRP
- Age
- Female gender
Treatment Goals
- Achieving remission or lowering disease activity.
- Reducing the progression of the disease itself.
- Maintaining joint function.
- Reducing the risk of joint damage.
Non-Pharmacological Treatments
- Rest (appropriate amount): avoid too much rest to prevent muscle atrophy, reduced range of motion.
- Occupational therapy/physical therapy.
- Assistive devices.
- Weight reduction (in people who are overweight or obese).
- Surgery (if needed).
- Mental health support.
Pharmacological Treatments
- Disease-modifying antirheumatic drugs (DMARDs): conventional synthetic DMARDs (methotrexate, sulfasalazine, hydroxychloroquine, and others) and biological DMARDs (TNF-a inhibitors, other biologics, including abatacept , interleukin-6 receptor antagonists, JAK inhibitors)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids (oral or injected)
Additional Treatments
- Methotrexate
- Leflunomide (Arava)
- Hydroxychloroquine (Plaquenil)
- Sulfasalazine
- Other DMARDs
- Biological DMARDs and TNF-a inhibitors
- Biologics or JAK Inhibitors
Monitoring
- Crucial for effective treatment and prevention of complications.
- Regular monitoring of blood counts, liver function tests, etc. is imperative.
- Timing of monitoring will vary on the medications and treatment.
- Early and consistent monitoring is essential.
Treatment Strategies
- DMARD monotherapy
- Combination therapy (dual, triple)
- Selection should be based on patient's individual needs.
Biosimilars
- Biosimilars are extremely similar to an original biologic drug.
- They should be clinically equivalent to the original biologic.
- Integration of biosimilars is beneficial and economical.
Supporting Therapies
- NSAIDs for symptom management (analgesia and anti-inflammatory)
- Corticosteroids for flares (adjunct therapy, bridging therapy)
- Acetaminophen, too, offering symptomatic relief, but less effective than NSAIDs for RA.
How to Select Therapy
- Treat-to-target approach is now favored over a non-target approach.
- Establish a therapy target (remission or reduced activity).
- Continuous monitoring is required.
- Providers should collaborate with patients.
Recommendations
- Employ a treat-to-target strategy.
- Consider MTX as the first choice for single DMARD therapy.
- Add a second/third DMARD or a biologic if monotherapy isn't enough.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the fundamentals of Rheumatoid Arthritis (RA), including its epidemiology, pathophysiology, and diagnosis. Students will learn about the signs, symptoms, complications, and treatments of RA, gaining a comprehensive understanding of this chronic autoimmune disease.