Podcast
Questions and Answers
A patient with chronic kidney disease presents with increased thirst and frequent urination at night. Which metabolic effect is most likely contributing to these symptoms?
A patient with chronic kidney disease presents with increased thirst and frequent urination at night. Which metabolic effect is most likely contributing to these symptoms?
- Decreased glucose in urine, leading to reduced fluid reabsorption.
- Electrolyte disturbances affecting the kidney's ability to concentrate urine. (correct)
- Increased production of erythropoietin causing excessive red blood cell production.
- Reduced urea production leading to decreased osmotic diuresis.
A patient with chronic kidney disease is prescribed an anticoagulant medication. Which hematological effect poses the greatest risk in this scenario?
A patient with chronic kidney disease is prescribed an anticoagulant medication. Which hematological effect poses the greatest risk in this scenario?
- Bleeding complications due to the combined effect of the medication and platelet dysfunction. (correct)
- Increased erythropoietin production leading to polycythemia.
- Thrombocytosis contributing to the formation of blood clots.
- Reduced white blood cell count increasing the risk of infection.
A patient with chronic kidney disease experiences a loss of appetite, nausea, and occasional vomiting. Which of the following gastrointestinal complications is LEAST likely to be the primary cause of these symptoms?
A patient with chronic kidney disease experiences a loss of appetite, nausea, and occasional vomiting. Which of the following gastrointestinal complications is LEAST likely to be the primary cause of these symptoms?
- Peptic ulcer formation.
- General gastrointestinal irritation from accumulated waste products.
- Reduced gastric motility
- Weight loss. (correct)
Which combination of factors creates the most significant risk for cardiovascular complications in patients with chronic kidney disease?
Which combination of factors creates the most significant risk for cardiovascular complications in patients with chronic kidney disease?
A patient with chronic kidney disease reports experiencing frequent headaches and drowsiness. Which underlying issue related to neuromuscular effects is most likely contributing to these symptoms?
A patient with chronic kidney disease reports experiencing frequent headaches and drowsiness. Which underlying issue related to neuromuscular effects is most likely contributing to these symptoms?
Which of the following scenarios would most likely lead to renal hypofunction?
Which of the following scenarios would most likely lead to renal hypofunction?
A patient with end-stage renal disease (ESRD) is undergoing haemodialysis. What is the PRIMARY reason normal body fluid volume and composition are disrupted in ESRD?
A patient with end-stage renal disease (ESRD) is undergoing haemodialysis. What is the PRIMARY reason normal body fluid volume and composition are disrupted in ESRD?
A patient with a history of glomerulonephritis is being evaluated for a kidney transplant. What underlying physiological derangement is the MOST critical consideration in determining their suitability for transplantation?
A patient with a history of glomerulonephritis is being evaluated for a kidney transplant. What underlying physiological derangement is the MOST critical consideration in determining their suitability for transplantation?
A patient presents with previously fatal renal disease, now successfully managed with treatment. What is the MOST likely long-term implication for their dental care?
A patient presents with previously fatal renal disease, now successfully managed with treatment. What is the MOST likely long-term implication for their dental care?
What is the MAIN purpose of studying kidney diseases in the context of dental practice?
What is the MAIN purpose of studying kidney diseases in the context of dental practice?
Flashcards
Chronic Kidney Disease
Chronic Kidney Disease
Progressive, irreversible damage to the kidneys that reduces their function over time.
Hypertension (in CKD)
Hypertension (in CKD)
Increased blood pressure, a common cardiovascular effect of chronic kidney disease.
Atheroma (in CKD)
Atheroma (in CKD)
A condition where arteries harden and narrow, potentially worsened by chronic kidney disease.
Anemia (in CKD)
Anemia (in CKD)
Signup and view all the flashcards
Infection Risk (in CKD)
Infection Risk (in CKD)
Signup and view all the flashcards
Renal Function
Renal Function
Signup and view all the flashcards
Causes of Renal Disease
Causes of Renal Disease
Signup and view all the flashcards
Renal Hypofunction
Renal Hypofunction
Signup and view all the flashcards
Causes of Renal Hypofunction
Causes of Renal Hypofunction
Signup and view all the flashcards
Blockage of Renal Outflow
Blockage of Renal Outflow
Signup and view all the flashcards
Study Notes
- Renal diseases falls under the realm of biomedical science.
GDC Learning Outcomes
- Understanding general and systemic diseases is crucial, especially concerning their impact on oral health
- The effect of a patient's periodontal and general health on their treatment plan and outcomes should be considered.
Learning Outcomes
- Understanding renal function, its effects on the body, as well as the dental relevance is important
- Listing the causes of renal function loss is necessary
- Describing the effects of kidney disease on the body is important
- Listing the symptoms of kidney disease is key
- Stating the management options for treating patients with kidney diseases will be discussed
- Highlighting the dental relevance and providing dental management skills, should form part of the treatment
- Describing any relating oral manifestation should be understood
Why Study Kidney Disease
- Kidney diseases are studied because of clinical presentations, associated oral manifestations and their dental management
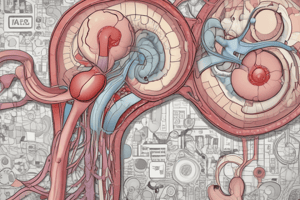
Renal Function
- Renal function is needed to maintain normal body and fluid volume and its composition
- It is essential for the excretion of waste products and drugs
- Some previously fatal kidney diseases can now be managed effectively
- The number of patients being treated with kidney transplants is growing
Loss of Renal function
- Renal disease can cause loss of renal function, which is triggered by infections, glomerulonephritis, hypertension, diabetes and congenital abnormalities
- Renal hypofunction can be a cause, an example of which is severe shock or hemorrhage
- Blockage of renal outflow can trigger loss of renal function, for example kidney stones and prostate tumors
Chronic Kidney Disease
- Chronic kidney disease, also know as chronic renal failure effects most body systems
- This may follow on from loss of renal function
- It is as a result of progressive irreversible kidney damage
- At first there are no symptoms of chronic kidney disease
- Later all kidney functions are reduced
Potential Impact of Chronic Kidney Disease
- Chronic kidney disease can have a metabolic, cardiovascular, gastrointestinal, neuromuscular, haematological, skin and immunological impact
Metabolic Effect
- The metabolic effects of chronic kidney disease include thirst, urination at night, glucose in urine and electrolyte disturbances
Cardiovascular Effects
- Hypertension is a cardiovascular effect
- Atheroma
Gastrointestinal Effects
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Peptic ulcer
- Hiccups
Neuromuscular
- Headaches
- Drowsiness
- Tremors
Haematological Effects
- Bleeding due to platelet dysfunction and/or anticoagulant medication
- Anemia due to deficiency of erythropoietin
Other Effects
- Bruises
- Rashes
- Prone to infection
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore renal diseases within biomedical science and their impact on oral health. Learn about kidney function, causes of loss, systemic effects, and symptoms. Understand dental relevance, management options, and oral manifestations for effective patient care.