Podcast Beta
Questions and Answers
Which of the following is NOT a criterion for reversible asthma based on FEV1 or FVC improvements?
The diffusion capacity of the lungs (DLCO) would most likely be decreased in which of the following conditions?
In pulmonary function tests, which statement correctly differentiates obstructive from restrictive lung disease?
What type of medical device is commonly used for delivering a medicinal drug in mist form for inhalation?
Signup and view all the answers
Which of the following correctly describes a condition in which DLCO is typically normal?
Signup and view all the answers
What is the primary aim of pulmonary rehabilitation?
Signup and view all the answers
Which of the following supplements is administered through devices such as nasal cannula and face masks?
Signup and view all the answers
Which test is used to assess a patient's oxygen level, blood pressure, and heart rate during exercise?
Signup and view all the answers
Which of the following inhaled medications typically provides a rapid onset of bronchodilation?
Signup and view all the answers
Why is chest physiotherapy commonly employed in patients with conditions like cystic fibrosis?
Signup and view all the answers
What is the primary characteristic of restrictive lung disease regarding Forced Vital Capacity (FVC)?
Signup and view all the answers
What is the expected FEV1/FVC ratio in a patient with obstructive lung disease?
Signup and view all the answers
What does a decreased Forced Expiratory Volume in 1 Second (FEV1) most commonly indicate?
Signup and view all the answers
In a patient with normal lung function, what percentage of the FVC is typically exhaled in the first second during forced expiration?
Signup and view all the answers
What aspect of lung function testing can help assess the reversibility of airway obstruction in asthmatic patients?
Signup and view all the answers
Which parameter is used to assess the gas exchange ability of the lungs?
Signup and view all the answers
Which of the following conditions is most likely associated with a significantly decreased FEV1?
Signup and view all the answers
In bronchodilator response testing, a significant improvement is indicated by what percentage increase in FEV1?
Signup and view all the answers
Which type of lung disease is characterized by air trapping due to narrowed airways?
Signup and view all the answers
What is the primary difference between obstructive and restrictive lung disease as indicated by pulmonary function testing?
Signup and view all the answers
What would be measured to establish Functional Residual Capacity (FRC)?
Signup and view all the answers
In pulmonary function tests, what would indicate abnormal results in terms of FEV1?
Signup and view all the answers
What is a major difference between obstructive and restrictive lung diseases regarding lung mechanics?
Signup and view all the answers
Which pulmonary function test is considered the gold standard for determining lung volumes?
Signup and view all the answers
Which condition is typically noted to have a normal FEV1/FVC ratio?
Signup and view all the answers
The clinical management of bronchospasm typically includes which of the following?
Signup and view all the answers
What is the primary factor affecting residual volume (RV) in restrictive lung disease?
Signup and view all the answers
What limitation is associated with traditional spirometers when evaluating lung function?
Signup and view all the answers
How is Total Lung Capacity (TLC) calculated?
Signup and view all the answers
Which of the following findings most likely indicates a restrictive lung disease pattern?
Signup and view all the answers
Study Notes
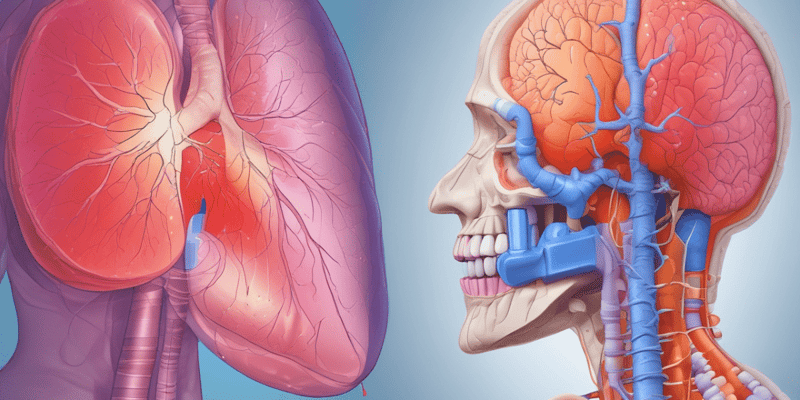
Pulmonary Function Tests (PFTs)
- PFTs are used for the evaluation of signs and symptoms such as cough, shortness of breath, wheezing, hypoxemia, hypercapnia, and crackles.
-
Indications for PFTs:
- Evaluation of signs and symptoms
- Abnormal Chest X-Ray or CT scan
- Assessment & monitoring of disease severity and progression
- Monitoring drug efficacy
- Pre-operative assessment
- Screening at-risk patients
-
Types of PFTs:
- Spirometry: measures volume versus time.
- Flow-Volume loops: Visual representation of air flow during inhalation and exhalation.
- Lung Volume Determination (Body Plethysmography): Gold standard for lung volume determination.
- Diffusion Capacity (DLCO): Assesses the gas exchange ability of the lungs. A DLCO greater than 75% of predicted value is considered normal.
- Bronchodilator Response Testing: Determines if there's a change in lung function after bronchodilator medication is administered.
PFT Parameters
- Tidal Volume (TV): volume of air moved during normal breath on quiet respiration.
- Inspiratory Reserve Volume (IRV): Maximum volume of air inhaled AFTER normal inhalation.
- Inspiratory Capacity (IC): Maximum volume of air that can be inhaled (TV + IRV).
- Expiratory Reserve Volume (ERV): Maximum volume of air exhaled AFTER normal exhalation.
- Forced Vital Capacity (FVC/VC): Maximum amount of air that can be exhaled after maximal inspiration.
- Residual Volume (RV): volume of air left in lungs after maximal expiration.
- Functional Residual Capacity (FRC): Volume of air in lung at end of normal expiration.
- Total Lung Capacity (TLC): Total volume of air in lungs after maximal inspiration.
- Peak Flow: Maximal flow rate that can be achieved during forceful expiration.
- Forced Expiratory Volume in 1 Second (FEV1): Amount of air forcefully exhaled in 1 second.
- Forced Expiratory Flow (FEF): Measurement of flow/speed of air being exhaled during portions of expirations.
Interpreting PFTs
-
Restrictive Lung Disease: Reduced compliance and lung volume.
- Examples: Interstitial lung disease, Scoliosis, Neuromuscular disease.
-
Obstructive Lung Disease: Narrowing of pulmonary airways hinder the person's ability to expel air from the lungs.
- Examples: COPD, Asthma, Bronchiectasis.
- FEV1: Forced expiratory volume in 1 second.
- FVC: Forced vital capacity.
- FEV1/FVC ratio: Indicates the percentage of air exhaled in the first second of a forced expiration.
- FEV1/FVC ratio of 0.7: Suggests obstructive lung disease.
Management of Pulmonary Conditions
- Oxygen Therapy: Used for hypoxemia, carbon monoxide poisoning, and cluster headaches.
-
Nebulizers: Medical device to deliver mist for inhaling a medicinal drug.
-
Types:
- Short-acting beta 2 agonist - albuterol
- Short-acting anticholinergic - ipratropium (Atrovent)
- Long-acting beta 2 agonist - formoterol/salmeterol
- Inhaled corticosteroids - budesonide (Pulmicort)
- Alpha/Beta Agonist - Racemic Epinephrine
-
Types:
- Inhalers: Medication in pressurized canister, delivered with propellant.
- Peak Flow Meters: Measure peak expiratory flow rate.
-
Chest Physiotherapy: Used in patients with cystic fibrosis, pneumonia, bronchiectasis, and neuromuscular disorders.
- Goal: mobilize bronchial secretions to large airways for easier expectoration.
-
Techniques:
- Postural Drainage
- Chest percussion/vibration
- High frequency chest wall oscillation
Pulmonary Rehabilitation
- Goal: Reduce symptoms, optimize function status, increase participation, and reduce healthcare costs.
- Conditions: COPD, asthma, pulmonary HTN, cystic fibrosis, transplant (before and after).
- Common Testing: Exercise stress test, Pulmonary function testing (PFT), Six-minute walk test.
-
Common Components:
- Breathing techniques
- Education on disease process
- Social activity
- Psychological counseling
- Nutritional counseling
- Smoking cessation
- Advanced care planning
Health Equity Concerns
- Inaccurate estimates of lung function can result in misclassification of disease severity and impact treatment decisions.
- The American Thoracic Society (ATS) recommends replacing race and ethnicity-specific equations with race-neutral average reference equations.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz focuses on Pulmonary Function Tests (PFTs), including their indications, types, and specific measurements used to evaluate lung function. It covers critical aspects such as spirometry, lung volume determination, and diffusion capacity. Whether you're a student or a healthcare professional, this quiz will enhance your understanding of PFTs.