Podcast
Questions and Answers
What is the main function of the oblique fiber group?
What is the main function of the oblique fiber group?
Which fiber bundles resist vertical force at the apical region of the root?
Which fiber bundles resist vertical force at the apical region of the root?
What is the primary role of accessory fibers?
What is the primary role of accessory fibers?
Oxytalan fibers are primarily associated with which of the following functions?
Oxytalan fibers are primarily associated with which of the following functions?
Signup and view all the answers
Which fiber group is responsible for resisting both vertical and lateral forces at the furcation of multirooted teeth?
Which fiber group is responsible for resisting both vertical and lateral forces at the furcation of multirooted teeth?
Signup and view all the answers
What characteristic differentiates oxytalan fibers from other types of fibers?
What characteristic differentiates oxytalan fibers from other types of fibers?
Signup and view all the answers
Which of the following statements accurately describes the horizontal fiber group?
Which of the following statements accurately describes the horizontal fiber group?
Signup and view all the answers
Which component runs tangentially to the long axis of the tooth and is meant to prevent rotation?
Which component runs tangentially to the long axis of the tooth and is meant to prevent rotation?
Signup and view all the answers
What is the primary function of the periodontal ligament?
What is the primary function of the periodontal ligament?
Signup and view all the answers
Which of the following statements about the width of the periodontal ligament is correct?
Which of the following statements about the width of the periodontal ligament is correct?
Signup and view all the answers
Which tissue type is NOT a component of the periodontium?
Which tissue type is NOT a component of the periodontium?
Signup and view all the answers
What feature of the periodontal ligament resembles that of immature connective tissues?
What feature of the periodontal ligament resembles that of immature connective tissues?
Signup and view all the answers
The width of the periodontal ligament is increased in which of these conditions?
The width of the periodontal ligament is increased in which of these conditions?
Signup and view all the answers
What factor can lead to inflammation affecting the periodontal ligament?
What factor can lead to inflammation affecting the periodontal ligament?
Signup and view all the answers
Which of the following is NOT considered a hard tissue of the periodontium?
Which of the following is NOT considered a hard tissue of the periodontium?
Signup and view all the answers
Which of the following best describes the periodontal ligament's structural features?
Which of the following best describes the periodontal ligament's structural features?
Signup and view all the answers
What are the main components of the periodontal ligament?
What are the main components of the periodontal ligament?
Signup and view all the answers
Which type of collagen fibers are primarily responsible for preventing intrusive apical tooth movements?
Which type of collagen fibers are primarily responsible for preventing intrusive apical tooth movements?
Signup and view all the answers
What is the primary function of gingival fibers in the periodontal ligament?
What is the primary function of gingival fibers in the periodontal ligament?
Signup and view all the answers
What are the five subgroups of the alveolodental ligament?
What are the five subgroups of the alveolodental ligament?
Signup and view all the answers
How do oxytalan fibers function within the periodontal ligament?
How do oxytalan fibers function within the periodontal ligament?
Signup and view all the answers
What is the primary role of the trans-septal ligament?
What is the primary role of the trans-septal ligament?
Signup and view all the answers
Which of the following groups resists vertical and intrusive forces?
Which of the following groups resists vertical and intrusive forces?
Signup and view all the answers
Where are elastic fibers predominantly found in the periodontal ligament?
Where are elastic fibers predominantly found in the periodontal ligament?
Signup and view all the answers
What is the primary function of the interstitial tissues within the periodontal ligament?
What is the primary function of the interstitial tissues within the periodontal ligament?
Signup and view all the answers
Which of the following statements best explains the effect of masticatory force on collagen fibers?
Which of the following statements best explains the effect of masticatory force on collagen fibers?
Signup and view all the answers
What is the critical timeframe for successful re-implantation of a knocked-out tooth?
What is the critical timeframe for successful re-implantation of a knocked-out tooth?
Signup and view all the answers
Which component is NOT involved in the supportive and protective functions of the periodontal ligament during masticatory forces?
Which component is NOT involved in the supportive and protective functions of the periodontal ligament during masticatory forces?
Signup and view all the answers
What happens to the periodontal ligament when masticatory pressure is transmitted rather than tension?
What happens to the periodontal ligament when masticatory pressure is transmitted rather than tension?
Signup and view all the answers
How do blood vessels in the periodontal ligament contribute to its functions?
How do blood vessels in the periodontal ligament contribute to its functions?
Signup and view all the answers
What percentage chance does a tooth have of successful re-implantation if replaced within half an hour?
What percentage chance does a tooth have of successful re-implantation if replaced within half an hour?
Signup and view all the answers
Which feature of the capillaries in the periodontal ligament contributes to its nutritive supply?
Which feature of the capillaries in the periodontal ligament contributes to its nutritive supply?
Signup and view all the answers
Which type of cells in the periodontal ligament are primarily responsible for the synthesis of collagen?
Which type of cells in the periodontal ligament are primarily responsible for the synthesis of collagen?
Signup and view all the answers
What role do cementoclasts play in the periodontal ligament?
What role do cementoclasts play in the periodontal ligament?
Signup and view all the answers
Which cell type can perform both synthetic and resorptive activities within the periodontal ligament?
Which cell type can perform both synthetic and resorptive activities within the periodontal ligament?
Signup and view all the answers
What makes osteoclasts unique in their functional role in the periodontal ligament?
What makes osteoclasts unique in their functional role in the periodontal ligament?
Signup and view all the answers
Which of the following components is NOT found in the intercellular substances of the periodontal ligament?
Which of the following components is NOT found in the intercellular substances of the periodontal ligament?
Signup and view all the answers
What type of cells include lymphocytes and macrophages in the periodontal ligament?
What type of cells include lymphocytes and macrophages in the periodontal ligament?
Signup and view all the answers
Which of the following cell types is known for extensive contractile properties in the periodontal ligament?
Which of the following cell types is known for extensive contractile properties in the periodontal ligament?
Signup and view all the answers
Which cells are responsible for generating alkaline phosphatase activity within the periodontal ligament?
Which cells are responsible for generating alkaline phosphatase activity within the periodontal ligament?
Signup and view all the answers
What is the primary protective function of the periodontal ligament (PDL) on the compressive side during mesiodistal orthodontic tooth movement?
What is the primary protective function of the periodontal ligament (PDL) on the compressive side during mesiodistal orthodontic tooth movement?
Signup and view all the answers
During orthodontic tooth movement, what role do osteoblasts play on the tension side of the periodontal ligament?
During orthodontic tooth movement, what role do osteoblasts play on the tension side of the periodontal ligament?
Signup and view all the answers
What sensory function do PDL mechanoreceptors provide?
What sensory function do PDL mechanoreceptors provide?
Signup and view all the answers
What happens in response to sudden overload as detected by the PDL mechanoreceptors?
What happens in response to sudden overload as detected by the PDL mechanoreceptors?
Signup and view all the answers
What is the primary role of fibroblasts in the periodontal ligament?
What is the primary role of fibroblasts in the periodontal ligament?
Signup and view all the answers
What impact does aging have on the periodontal ligament?
What impact does aging have on the periodontal ligament?
Signup and view all the answers
What are cementicles, and how are they formed in the context of the periodontal ligament?
What are cementicles, and how are they formed in the context of the periodontal ligament?
Signup and view all the answers
Which cells are essential for building up cementum and bone in the periodontal ligament?
Which cells are essential for building up cementum and bone in the periodontal ligament?
Signup and view all the answers
Study Notes
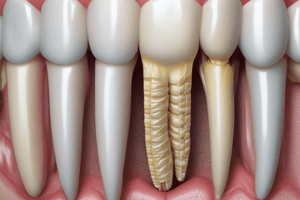
Periodontal Ligament Structure
- The periodontal ligament (PDL) is the investing and supporting attachment system of the teeth.
- It consists of two soft tissues and two hard tissues.
- The soft tissues include:
- Gingiva: Covers the neck of the tooth and part of the alveolar bone.
- Periodontal ligament (PDL): A strong ligament attaching the tooth to the alveolar bone.
- The hard tissues include:
- Cementum: Covers the anatomical root of the tooth.
- Alveolar bone: The bone of the jaw surrounding the root of the tooth.
Periodontal Ligament Definition
- The periodontal ligament is dense fibrous connective tissue filling the space between the root and the alveolus.
Periodontal Ligament Inflammation
- Inflammation from the dental pulp and gingiva can spread to the PDL and other apical supporting tissues.
Periodontal Ligament Width
- The PDL ranges from 0.15-0.21 mm in width.
- The narrowest area is at the middle of the root (fulcrum).
- The widest area is at the alveolar crest, followed by the apical region.
- Width is reduced in non-functioning and unerupted teeth.
- Width is increased in teeth subjected to occlusal stress (within physiological limits), and in deciduous teeth.
Periodontal Ligament Features
- The periodontal ligament resembles immature, fetal-like connective tissue in:
- High rate of turnover.
- Large volume of ground substance.
- Presence of oxytalan fibers.
- High cellularity.
- Similar biomechanical properties.
Periodontal Ligament Development
- Dense fibrous and cellular tissues immediately encapsulate the developing tooth (cementum)
- Mesenchymal tissue, away from the tooth, forms the PDL and alveolar bone.
Periodontal Ligament Tissue Structure
- The PDL is formed of cells, fibers, and intercellular substances.
- Cells: Synthetic, resorptive, progenitor, and defensive.
- Fibers: Collagen, oxytalan, and elastic.
- Intercellular substances: Ground substances, blood vessels, nerves, and lymphatics.
Collagen Fibers (Type 1)
- Embedded in both cementum and bone (Sharpey's fibers).
- Principal fibers: Prevent intrusive and lateral tooth movement.
- Accessory fibers: Prevent rotatory tooth movement.
Oxytalan Fibers
- (Immature elastic fibers): Maintain blood vessel patency.
Elastic Fibers
- Primarily found in the walls of blood vessels.
Principal Fibers (Groups)
- Gingival fibers form a rigid cuff around the tooth, adding stability to the gingiva and resisting displacement.
- Transseptal or interdental ligament connects adjacent teeth, maintaining mesiodistal width and preventing rotation.
- Alveolodental ligament: Subdivided into crest, horizontal, oblique, apical, and interradicular groups, resisting masticatory forces and vertical/intrusive forces. Horizontal group fibers run parallel to the tooth, preventing tooth extrusion and lateral movement, the oblique are found in the greatest numbers and perform the key role in tooth support during masticatory forces, vertical and intrusive forces, and the apical group runs from the root apex to the surrounding bone, resisting vertical forces, and the interradicular fibers run from the septum between the roots to the furcation, resisting vertical and lateral forces.
Blood Supply
- Derived from three sources:
- Gingival vessels
- Intra-alveolar vessels (main supply)
- Apical vessels supplying the dental pulp.
- Perforating arteries are more abundant in the PDL of posterior teeth compared to anterior.
- Coiled fenestrated capillaries are found in the cervical region.
- Numerous arteriovenous anastomoses occur in the PDL.
- Venous blood flows from the gingival region to the apical area and bone.
Nerve Supply
- Derived from inferior or superior dental nerves.
- Bundles of nerve fibers run from the apical region of the root towards the gingival margin.
- Nerves enter the ligament horizontally through multiple foramina in the bone.
- Nerve fibers can be large or small:
- Small myelinated/unmyelinated fibers: Responsible for pain sensation.
- Large myelinated fibers (mechanoreceptors): Responsible for touch and pressure.
- Stimulation of mechanoreceptors initiates a reflex jaw opening.
Interstitial Tissues
- Found between PDL fibers.
- Contain blood vessels, lymphatics, and nerves.
- Surrounded by loose connective tissue.
- Designed to withstand masticatory forces.
Regeneration
- Regeneration of PDL and cementum is possible.
Knocked-out Tooth
- The length of time before re-implantation (within half an hour) and the approach to transport the tooth (in saline) are critical for successful re-implantation.
- The PDL regenerates and revascularizes rapidly. Success rates are around 90%.
PDL Functions
- Supportive & protective: Achieved by collagen fibers, blood vessels, and nerves/mechanoreceptors.
- Mesiodistal Orthodontic Movement: Achieved by collagen fibers, blood vessels, and ground substances.
Collagen Fiber Function
- The wavy shape of collagen fibers straightens under masticatory forces, acting as inelastic strings.
- This transforms masticatory pressure into tension on the cementum and bone. Allowing healthy bone and cementum cell differentiation.
- If masticatory force is pressure type, osteoclast differentiation and bone resorption will occur.
Blood Vessel Function
- Blood vessels function as hydraulic dampers or shock absorbers as they reduce compressive forces. This allows for internal remodeling.
- Their arrangement includes rich capillary networks and coils that are patent. They are anchored to bone and cementum through oxytalan fibers.
PDL Function During Orthodontic Tooth Movement
- Compressive side: The PDL functions as a cushion, protecting alveolar bone from excessive compressive forces, and allowing internal remodeling rather than direct resorptive effects. Prevents bone loss during movement.
- Tension side: PDL fibers straighten out initiating osteoblastic differentiation that changes tooth position. This side influences the overall bone shaping and allows for teeth movement.
Internal Remodeling & Bone
- Internal remodeling preserves the architecture and thickness of the bone.
Sensory Function of PDL
- The PDL mechanoreceptors allow for touch and pressure sensations on the teeth.
- Sudden overload leads to a proprioceptive reflex.
- The proprioceptive reflex inhibits masticatory muscle activity, opening the mouth, and reducing applied forces
Nutritive Function
- The blood vessels in the PDL deliver nutrients to the ligament cells.
Formative Function
- Fibroblasts form new PDL fibers.
- Cementoblasts and osteoblasts (necessary for maintaining cementum and bone).
Age Changes in PDL
- PDL shows age changes in vasularity, cellularity, and thickness.
- Cementicles may be present.
Cementicles
- Cementicles may occur near the cementum surface: Free, attached, or embedded.
- Formed due to calcific deposits on degenerated cells, areas of hemorrhage, or epithelial rests of Malassez.
- Common with aging, but also may occur in younger individuals after trauma.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the anatomy and functions of the periodontal ligament (PDL), including its composition of soft and hard tissues. It will also cover aspects of PDL inflammation and its clinical significance in dentistry. Test your knowledge on this crucial component of dental health!