Podcast
Questions and Answers
What is the primary function of antimicrobial therapy in periodontal disease?
What is the primary function of antimicrobial therapy in periodontal disease?
- To sustain the tissues and prevent destruction (correct)
- To eliminate all bacteria from the mouth
- To increase bone loss
- To enhance the biofilm formation
Antibiotics used in periodontal therapy are ineffective against biofilm-forming bacteria.
Antibiotics used in periodontal therapy are ineffective against biofilm-forming bacteria.
False (B)
Which bacterium is commonly associated with periodontal disease and biofilm formation?
Which bacterium is commonly associated with periodontal disease and biofilm formation?
p.gingivalis
The _______ response can indirectly cause more bone destruction in periodontal disease.
The _______ response can indirectly cause more bone destruction in periodontal disease.
Match the following antibiotics to their common side effects:
Match the following antibiotics to their common side effects:
Which of the following factors can influence a host's immune response to periodontal bacteria?
Which of the following factors can influence a host's immune response to periodontal bacteria?
Which combination of antibiotics is effective against A.actinomycetemcomitans?
Which combination of antibiotics is effective against A.actinomycetemcomitans?
Combination therapies are often used to enhance the effectiveness of treatment for periodontitis.
Combination therapies are often used to enhance the effectiveness of treatment for periodontitis.
Antibiotics have a significant effect on the management of periodontal diseases.
Antibiotics have a significant effect on the management of periodontal diseases.
What type of therapy involves placing anti-infective agents directly into the periodontal pocket?
What type of therapy involves placing anti-infective agents directly into the periodontal pocket?
What is required to effectively combat biofilms in periodontal infections?
What is required to effectively combat biofilms in periodontal infections?
The combination of __________ is known to have an additive effect against periodontal pathogens.
The combination of __________ is known to have an additive effect against periodontal pathogens.
Match the following antibiotics with their primary focus in periodontal therapy:
Match the following antibiotics with their primary focus in periodontal therapy:
What is a contraindication for using locally delivered antimicrobial agents?
What is a contraindication for using locally delivered antimicrobial agents?
Single antibiotics are generally effective against all types of periodontal pathogens.
Single antibiotics are generally effective against all types of periodontal pathogens.
What contributes to the complexity of treating periodontal infections?
What contributes to the complexity of treating periodontal infections?
What is one of the benefits of using tetracyclines in the treatment of periodontal diseases?
What is one of the benefits of using tetracyclines in the treatment of periodontal diseases?
Metronidazole is the drug of choice for treating Aggregatibacter actinomycetemcomitans infections.
Metronidazole is the drug of choice for treating Aggregatibacter actinomycetemcomitans infections.
What is a common side effect associated with tetracyclines?
What is a common side effect associated with tetracyclines?
Tetracyclines are classified as ______ antibiotics.
Tetracyclines are classified as ______ antibiotics.
Match the following antibiotics to their primary mechanism or usage:
Match the following antibiotics to their primary mechanism or usage:
Which of the following antibiotics is commonly used in combination therapies for periodontitis?
Which of the following antibiotics is commonly used in combination therapies for periodontitis?
Tetracyclines are effective against gram-negative bacteria more than gram-positive bacteria.
Tetracyclines are effective against gram-negative bacteria more than gram-positive bacteria.
What is a reason for the increased use of combination antibiotics in periodontal therapy?
What is a reason for the increased use of combination antibiotics in periodontal therapy?
Study Notes
Periodontal Lesions
- Periodontal lesions are more prevalent than normal gingiva.
- Antibiotics are effective in enhancing attachment levels and reducing gingival enlargement in patients with aggressive periodontitis.
Antibiotic Therapy
- No single antibiotic is effective against all periodontal pathogens.
- Periodontal infections are complex and often involve a mix of aerobic, microaerophilic, and anaerobic bacteria, both gram negative and gram positive.
- This necessitates combining antibiotics serially or simultaneously.
- Metronidazole and Amoxicillin/Augmentin are effective together in fighting periodontitis.
- Metronidazole and Ciprofloxacin are effective in fighting Aggregatibacter actinomycetemcomitans.
- Systemic antibiotic therapy alongside mechanical treatment effectively addresses recalcitrant periodontal infections and Aggregatibacter actinomycetemcomitans-related LAP infections.
Periodontal Disease
- There's no singular identified microbe or group responsible for these diseases.
- Antibiotics have had a limited impact on managing periodontal diseases.
- Effective periodontal treatments require debridement of root surfaces, immaculate oral hygiene, and frequent maintenance therapy.
- Biofilms require 500 times higher antibiotic concentrations than systemic therapeutic levels to be effective.
- It is essential to physically break down biofilms to provide antibiotics access to periodontal pathogens.
- Locally delivered antimicrobial agents supplement scaling and root planing and aid in controlling bacterial growth.
- Locally delivered agents are contraindicated when multiple sites exist within the same quadrant.
Biofilms
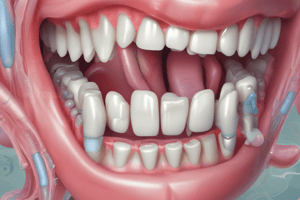
- Biofilms are complex microbial communities attached to tooth surfaces.
- Supragingival Plaque: Biofilm above the gumline
- Subgingival Plaque: Biofilm below the gumline
- Periodontal Pocket: Space between the tooth and gum.
P. gingivalisare found in the pocket.
Host Response & Antibiotic Use
- Host immune response is responsible for tissue destruction.
- Antibiotics sustain tissues and prevent destruction.
- Biofilms offer protection from the host's immune response and antibiotics in the periodontal pocket.
Treatment
- Mechanical removal of local factors and subgingival plaque biofilm disruption are essential.
- Anti-infective therapies include Mechanical, Systemic (oral antibiotics), and Local (direct placement of anti-infective agents into the periodontal pocket).
Chemotherapeutic Agents
- Bacteria and their byproducts cause attachment and bone loss.
- However, the host's immune response to bacterial infection can lead to more bone destruction.
- Chemotherapeutic agents modulate the immune response to bacteria and reduce self-destructive responses.
- A combination of antibiotics may be required to eliminate all pathogens from periodontal pockets.
Tetracyclines
- Tetracyclines are frequently used to treat periodontal diseases, especially refractory periodontitis.
- Concentrate in periodontal tissues and inhibit Aggregatibacter actinomycetemcomitans growth.
- Exhibit an anticollagenase effect inhibiting tissue destruction and supporting bone regeneration.
- Bacteriostatic and more effective against gram-positive bacteria than gram-negative.
- Concentration in the gingival crevice is 2 to 10 times greater than serum.
- Tetracycline, Minocycline, and Doxycycline are commonly used in periodontal therapy.
- Side effects: Gastrointestinal disturbances, Photosensitivity, Hypersensitivity, elevated Blood Urea Nitrogen levels, Blood Dyscrasias, Dizziness, Headaches, tooth discoloration in children under 12.
Metronidazole and Amoxicillin-Clavulanic Acid
- Amoxicillin is degraded by the beta-lactamases enzyme released by bacteria.
- Clavulanic acid combats the beta-lactamases enzyme, protecting amoxicillin.
- Metronidazole is effective against anaerobic gram-negative bacteria, including Aggregatibacter actinomycetemcomitans when used in combination with other antibiotics.
- While tetracyclines were frequently used in the past for localized aggressive periodontitis, combination antibiotics often replace them.
- Localized aggressive periodontitis mainly affects first molars.
- Metronidazole + Amoxicillin-Clavulanic acid is effective for localized aggressive periodontitis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the complex relationship between periodontal lesions and antibiotic therapy. This quiz covers the efficacy of antibiotics in treating aggressive periodontitis and the diversity of bacteria involved in periodontal infections. Test your knowledge on effective treatments for periodontal diseases and the appropriate use of antibiotics.