Podcast
Questions and Answers
What is the meaning of the term 'erythematosus' in systemic lupus erythematosus (SLE)?
What is the meaning of the term 'erythematosus' in systemic lupus erythematosus (SLE)?
- Denotes the age group primarily affected.
- Indicates the typical red facial rash associated with the condition. (correct)
- Describes the autoimmune nature of the disease.
- Refers to the systemic involvement of the disorder.
Which of the following is a significant complication associated with systemic lupus erythematosus?
Which of the following is a significant complication associated with systemic lupus erythematosus?
- Gastrointestinal bleeding
- Gallbladder disease
- Cardiovascular disease (correct)
- Chronic fatigue syndrome
Which laboratory finding is most specific for systemic lupus erythematosus?
Which laboratory finding is most specific for systemic lupus erythematosus?
- Elevated CRP levels
- Anti-double stranded DNA (anti-dsDNA) antibodies (correct)
- Anti-nuclear antibodies (ANA)
- Low platelet count
What is the typical shape of the rash seen in systemic lupus erythematosus?
What is the typical shape of the rash seen in systemic lupus erythematosus?
In the context of systemic lupus erythematosus, which symptom is generally NOT considered a typical manifestation?
In the context of systemic lupus erythematosus, which symptom is generally NOT considered a typical manifestation?
Which of the following populations is most affected by systemic lupus erythematosus?
Which of the following populations is most affected by systemic lupus erythematosus?
What would a renal biopsy typically investigate in patients suspected of having systemic lupus erythematosus?
What would a renal biopsy typically investigate in patients suspected of having systemic lupus erythematosus?
Which of the following symptoms is associated with Raynaud's phenomenon in systemic lupus erythematosus?
Which of the following symptoms is associated with Raynaud's phenomenon in systemic lupus erythematosus?
Which antibody is highly specific to systemic lupus erythematosus (SLE) but not very sensitive?
Which antibody is highly specific to systemic lupus erythematosus (SLE) but not very sensitive?
What is the most common complication associated with systemic lupus erythematosus (SLE)?
What is the most common complication associated with systemic lupus erythematosus (SLE)?
Which of the following is most associated with limited cutaneous systemic sclerosis?
Which of the following is most associated with limited cutaneous systemic sclerosis?
What management option is considered first-line for systemic lupus erythematosus (SLE)?
What management option is considered first-line for systemic lupus erythematosus (SLE)?
Which of the following options represents a common hematological complication of SLE?
Which of the following options represents a common hematological complication of SLE?
Which symptom is primarily caused by inflammation of the lining of the lungs in SLE patients?
Which symptom is primarily caused by inflammation of the lining of the lungs in SLE patients?
Which drug is considered a biologic therapy for severe systemic lupus erythematosus (SLE)?
Which drug is considered a biologic therapy for severe systemic lupus erythematosus (SLE)?
What is the significance of antiphospholipid antibodies in patients with SLE?
What is the significance of antiphospholipid antibodies in patients with SLE?
Which of the following is primarily evaluated using a renal biopsy in SLE patients?
Which of the following is primarily evaluated using a renal biopsy in SLE patients?
Which symptom is an indication of optic neuritis in SLE?
Which symptom is an indication of optic neuritis in SLE?
Study Notes
Overview of Systemic Lupus Erythematosus (SLE)
- SLE is an inflammatory autoimmune disorder affecting multiple organs.
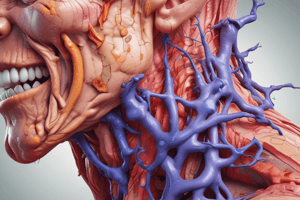
- Characterized by a red malar rash across the face, often referred to as a “butterfly” rash.
- Primarily affects women and people of Asian, African, Caribbean, and Hispanic descent, typically in their young to middle adulthood.
Course and Complications
- SLE follows a relapsing-remitting pattern with alternating flare-ups and symptom-free periods.
- Chronic inflammation can lead to reduced life expectancy, mainly due to cardiovascular disease and infections.
Pathophysiology
- Marked by the presence of anti-nuclear antibodies (ANA), which target proteins in the cell nucleus, inciting ongoing inflammation.
Symptoms and Presentation
- Common symptoms include fatigue, weight loss, joint and muscle pain (arthralgia, myalgia), fever, and a photosensitive malar rash.
- Additional symptoms can encompass lymphadenopathy, splenomegaly, respiratory issues, mouth ulcers, hair loss, Raynaud’s phenomenon, and edema from nephritis.
Investigations and Diagnostic Markers
- Diagnosis involves identifying autoantibodies, abnormal full blood counts, raised inflammatory markers (CRP, ESR), and reduced complement levels (C3, C4).
- Proteinuria indicates lupus nephritis, with renal biopsy used to assess kidney involvement.
Autoantibodies
- Approximately 85% of SLE patients test positive for ANA, though positive results can also occur in healthy individuals or other diseases.
- Anti-double stranded DNA (anti-dsDNA) antibodies are highly specific to SLE, with about 50% prevalence in patients and useful for monitoring disease activity.
- Extractable nuclear antigen panel identifies antibodies related to various connective tissue disorders such as Anti-Sm, anti-centromere, anti-Ro, anti-La, anti-Scl-70, and anti-Jo-1.
Antiphospholipid Antibodies and Syndrome
- Antiphospholipid antibodies occur in 40% of SLE patients, increasing the risk of venous thromboembolism.
Diagnostic Criteria
- The EULAR/ACR criteria from 2019 evaluate clinical features and autoantibodies for SLE diagnosis.
Complications Associated with SLE
- Leading causes of death include cardiovascular disease due to chronic inflammation in blood vessels.
- Increased risk of infections attributed to the disease itself and immunosuppressant therapy.
- Anaemia may arise from various causes: chronic disease, autoimmune processes, or medication impact.
- Potential cardiovascular issues include pericarditis and pleuritis, as well as interstitial lung disease and lupus nephritis, which may lead to renal failure.
- Neuropsychiatric symptoms may occur due to CNS inflammation, manifesting as optic neuritis and psychosis.
- Women with SLE are at heightened risk for obstetric complications, including recurrent miscarriage and pre-eclampsia.
Management Strategies
- Primary treatment focuses on symptom control and reducing complications, emphasizing minimal medication use to limit side effects.
- Essential measures include sun protection to manage photosensitivity.
- First-line treatments include hydroxychloroquine, non-steroidal anti-inflammatory drugs (NSAIDs), and steroids (e.g. prednisolone).
- For severe or resistant cases, disease-modifying antirheumatic drugs (DMARDs) like methotrexate and biologic therapies such as Rituximab and Belimumab are utilized.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz explores Systemic Lupus Erythematosus (SLE), an autoimmune disorder with various impacts on health. It details its characteristics, complications, and common symptoms. Understand the pathophysiology and demographics affected by this condition.