Podcast
Questions and Answers
Which of the following are considered red flags when assessing orthopedic conditions?
Which of the following are considered red flags when assessing orthopedic conditions?
- Muscle weakness
- Fatigue
- Fractures (correct)
- Joint stiffness
What are the '5Ps' associated with compartment syndrome?
What are the '5Ps' associated with compartment syndrome?
- Puffiness, pulsations, paresthesia, pain, paralysis
- Pain, pallor, paresthesia, pulselessness, paralysis (correct)
- Pain, pressure, peripheral pulse, position, paralysis
- Pain, pallor, premium, paralysis, pressure
What indicates a fracture during the orthopedic assessment?
What indicates a fracture during the orthopedic assessment?
- Swelling around the joint
- Pain with squeezing of the bone (correct)
- Increased range of motion
- Decrease in muscle mass
Which test is NOT typically used to screen for fractures?
Which test is NOT typically used to screen for fractures?
What can be a sign of dislocation in an orthopedic assessment?
What can be a sign of dislocation in an orthopedic assessment?
Which hepatitis virus is associated with a primarily parenteral route of transmission?
Which hepatitis virus is associated with a primarily parenteral route of transmission?
What is the average incubation period for Hepatitis C?
What is the average incubation period for Hepatitis C?
Which hepatitis virus is most likely to lead to chronic liver disease?
Which hepatitis virus is most likely to lead to chronic liver disease?
Which diagnostic method is used to confirm Hepatitis B infection?
Which diagnostic method is used to confirm Hepatitis B infection?
What characterizes the symptomatic icteric phase in hepatitis infections?
What characterizes the symptomatic icteric phase in hepatitis infections?
What is the primary mode of transmission for Hepatitis B?
What is the primary mode of transmission for Hepatitis B?
Which condition is characterized by a high risk of cirrhosis and hepatocellular carcinoma with long-term infection?
Which condition is characterized by a high risk of cirrhosis and hepatocellular carcinoma with long-term infection?
What is a common feature of Non-Alcoholic Steatohepatitis (NASH)?
What is a common feature of Non-Alcoholic Steatohepatitis (NASH)?
Which statement about Hepatitis A is true?
Which statement about Hepatitis A is true?
What percentage of individuals with chronic Hepatitis C eventually develop cirrhosis?
What percentage of individuals with chronic Hepatitis C eventually develop cirrhosis?
What are the two main variants of esophageal carcinomas?
What are the two main variants of esophageal carcinomas?
What major risk factor is associated with squamous cell carcinoma of the esophagus?
What major risk factor is associated with squamous cell carcinoma of the esophagus?
Which mutation is commonly present at early stages of esophageal adenocarcinoma?
Which mutation is commonly present at early stages of esophageal adenocarcinoma?
In which part of the esophagus does esophageal adenocarcinoma typically occur?
In which part of the esophagus does esophageal adenocarcinoma typically occur?
Which of the following describes the initial presentation of esophageal adenocarcinoma?
Which of the following describes the initial presentation of esophageal adenocarcinoma?
What is the primary demographic trend associated with gastric adenomas?
What is the primary demographic trend associated with gastric adenomas?
What is the relationship between the size of gastric adenomas and the risk of progression to adenocarcinoma?
What is the relationship between the size of gastric adenomas and the risk of progression to adenocarcinoma?
In which part of the stomach are gastric adenomas most commonly located?
In which part of the stomach are gastric adenomas most commonly located?
Which type of gastric cancer comprises the majority of cases?
Which type of gastric cancer comprises the majority of cases?
Which geographical regions have the highest incidence of gastric adenocarcinoma?
Which geographical regions have the highest incidence of gastric adenocarcinoma?
What is the primary mechanism of action for H2 blockers in reducing stomach acid?
What is the primary mechanism of action for H2 blockers in reducing stomach acid?
Which generic drug names typically indicate the use of H2 blockers?
Which generic drug names typically indicate the use of H2 blockers?
In what condition would H2 blockers be less effective compared to PPIs?
In what condition would H2 blockers be less effective compared to PPIs?
What neurotransmitter primarily activates M3 receptors on parietal cells?
What neurotransmitter primarily activates M3 receptors on parietal cells?
Which of the following is NOT a common therapeutic use for H2 blockers?
Which of the following is NOT a common therapeutic use for H2 blockers?
What is the primary mechanism of action of proton pump inhibitors (PPIs)?
What is the primary mechanism of action of proton pump inhibitors (PPIs)?
What is the most common therapeutic use of PGE1 analogues?
What is the most common therapeutic use of PGE1 analogues?
Which of the following specific agents is classified as a proton pump inhibitor?
Which of the following specific agents is classified as a proton pump inhibitor?
What physiological effects do prostaglandins (PGs) have in the gastrointestinal tract?
What physiological effects do prostaglandins (PGs) have in the gastrointestinal tract?
Why are PGE1 analogues contraindicated in pregnant women?
Why are PGE1 analogues contraindicated in pregnant women?
Study Notes
Learning Objectives
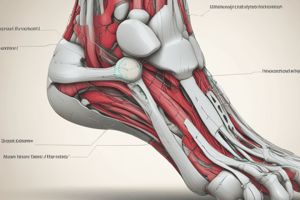
- Identify red flags and yellow flags in orthopedic assessments.
- Understand pain sensation and its impact on specific tissues.
- Describe the stages of injury and healing, and their respective treatment goals.
- Compare normal and pathological end feels.
- Define muscle spasm and guarding.
Red Flags
- Include fractures, dislocations, infections, and compartment syndrome.
- Fracture indicators: significant trauma history, age over 55, dark bruising, pain in a four-step test, inability to move the area.
- Dislocations require a neurovascular screening and may need emergency intervention.
- Compartment syndrome symptoms: pain, pallor, paresthesia, pulselessness, paralysis (the 5Ps).
Pain Sensitivity to Tissue
- Most sensitive: Skin, Periosteum, and Fibrous Capsule.
- Least sensitive: Fibrocartilage and Articular Cartilage.
- Muscle injuries demonstrate dull ache and sharp pain, particularly upon movement or contraction.
Pain Assessment by Condition
- Muscle Injury (Strain or Tendinopathy): Decreased Active Range of Motion (AROM), normal Passive Range of Motion (PROM), tenderness during resisted contraction.
- Fascial Strain: Reduced AROM and PROM, potential subcutaneous adhesion.
- Ligament Injury (Sprain): Painful end ROM, tenderness with palpation, may show instability.
- Capsulitis: Pain with capsule palpation, limited motion in one direction, indicates muscular or tendon damage.
- Joint Injury (Arthropathy): Mild loss of ROM, possible crepitus during motion.
- Bone Injury (Fracture): Limited AROM and PROM with sharp pain, requires fracture assessment.
- Nerve Injury: Reduced nerve functionality shows numbness and muscle weakness.
Stages of Healing
- Acute Phase (1-5 days): Focus on pain reduction; employ massage, aquatic therapy, and pain-free exercises.
- Functional Stage (2 weeks - 6 months): Goals include maintaining activity level and preventing recurrence; incorporate fast walking and sport-specific exercises.
- Remodeling Phase (3 weeks - 12+ months): Focus on maintaining ability and reducing scar tissue; introduce strengthening exercises and ensure proper warm-up/stretching.
Treatment Guidelines Summary
- Acute Phase: 2-3 days; apply PRICE/METH protocols and manage psychosocial factors.
- Post-Acute Phase: 2 days - 6 weeks; aims include pain reduction and tissue alignment.
- Chronic Phase: 2 weeks - 12+ months; emphasizes loading properly to enhance scar tissue elasticity and treat psychosocial issues.
Yellow Flags
- Indicate risks for developing chronic pain; assess psychosocial factors if recovery is stagnant after 4-6 weeks.
- Physical factors: inactivity, deconditioning; Psychological factors: depression, anxiety; Social context: work-related issues or poor support structures.
End Feel Types
- Normal End Feel: RM Tissue Stretch, Soft Tissue Approximation, Ligamentous, and Bone to Bone identifiable by hard and painless resistance.
- Pathological End Feel: Painful or restricted end feels like Muscle Spasm, Capsular, Springy Block, and Empty, indicating potential instability or injury.
Muscle Spasm and Guarding
- Protective mechanisms causing involuntary contraction post-injury to reduce motion and pain.
- Increased muscle tone may indicate upper motor neuron lesions.
Hepatitis Overview
- Types of Hepatitis: A, B, C, D, and E, each with distinct genomic structures and transmission routes.
- Transmission:
- Hepatitis A and E: Fecal-oral route.
- Hepatitis B, C, and D: Parenteral or sexual transmission.
- Incubation Period: Ranges from 2-26 weeks, depending on the type.
- Chronic Liver Disease:
- Hepatitis A: Never leads to chronic disease.
- Hepatitis B: 5-10% chronicity.
- Hepatitis C: Over 80% chronicity.
- Hepatitis D: Can worsen chronic hepatitis B.
- Hepatitis E: Rarely causes chronic liver disease.
Syndromes of Hepatitis Infection
- Acute Symptomatic: Characterized by incubation, preicteric, icteric (jaundice), and convalescence phases.
- Chronic Hepatitis: May present as a carrier state.
- Fulminant Hepatic Failure: Rare but severe condition.
Hepatitis A
- Common in areas with poor hygiene, with 30-50,000 new cases yearly in the US.
- Almost always self-limited, with rare fulminant hepatic failure.
- Clinical features include fatigue, nausea, and jaundice.
Hepatitis B
- Most prevalent globally, often acquired at birth.
- Can progress to cirrhosis or hepatocellular carcinoma.
- Acute infections may show nonspecific symptoms, jaundice, and upper right quadrant pain.
Hepatitis C
- Affects 1.6% of the population with chronic infection, primarily through blood-to-blood contact.
- Hallmarked by persistent infection and chronic hepatitis, often asymptomatic.
- Modern treatments provide significant cures, especially for genotypes 1a and 1b.
Hepatitis D & E
- Hepatitis D: Requires coinfection with hepatitis B; can lead to acute severe hepatitis or chronic infections.
- Hepatitis E: Zoonotic and self-limited; high mortality in pregnant women (up to 20%).
Alcoholic Liver Disease
- Forms: Hepatitis, hepatic steatosis (reversible), and steatofibrosis (potentially leading to cirrhosis).
- Clinical Features: Non-specific symptoms, including malaise and tender hepatomegaly; alcoholic hepatitis appears after heavy drinking.
- Prognosis: Better outcome if detoxified; survival rates drop significantly with continued alcohol consumption.
Non-Alcoholic Fatty Liver Disease (NAFLD)
- Most common liver disease in the US; encompasses non-alcoholic steatohepatitis (NASH).
- NASH may progress to cirrhosis and increase liver cancer risk.
- Clinical features often asymptomatic until late-stage liver failure occurs.
Drug and Toxin-Induced Liver Disease
- Most common cause of fulminant hepatitis; categorized into predictable and unpredictable hepatotoxins.
- Acetaminophen is a leading cause of acute liver failure necessitating transplantation.
Cirrhosis and Portal Hypertension
- Caused by obstructed bile flow, leading to increased pressure and collateral circulation, resulting in esophageal varices.
- Varices are prone to rupture, causing severe bleeding and high mortality rates.
Intrahepatic Biliary Tract Disease
- Includes conditions like primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC).
- Both conditions lead to liver damage and cirrhosis, with different initial symptoms and risk profiles.
Clinical Implications
- Awareness of liver pathology and related diseases is crucial for diagnosis and treatment.
- Persistent symptoms and risk factors should prompt further investigation into liver health.
Esophageal Carcinomas
- Two main types: adenocarcinoma and squamous cell carcinoma.
- Common yet highly fatal; 15,560 diagnoses and 13,940 deaths in the U.S. in 2007.
- Risk factors for squamous cell carcinoma include tobacco/alcohol use, poverty, caustic injury, achalasia, and very hot beverages.
- Adenocarcinoma risks are linked to long-standing GERD, Barrett’s esophagus, and tobacco; diets rich in fruits and vegetables provide protection.
Esophageal Adenocarcinoma - Etiology & Pathogenesis
- Mutations accumulate in epithelial clones of Barrett's metaplasia leading to dysplasia and invasive carcinoma.
- Early mutation or overexpression of p53 is common.
- Additional genetic changes include amplification of c-ERB-B2, cyclin D1, and cyclin E genes, as well as RB mutations.
Esophageal Adenocarcinoma - Pathology
- Typically found in the distal esophagus, potentially invading the gastric cardia.
- Initial appearance as flat or raised patches in intact mucosa.
- Large masses (≥ 5 cm) can form, possibly ulcerating or deeply invading.
- Often associated with adjacent Barrett esophagus, resembling intestinal cells.
Gastric Adenoma - Introduction
- Comprises 10% of all gastric polyps; incidence increases with age, predominantly in men aged 50-60.
- Higher malignant potential compared to colonic adenomas.
- Associated with chronic gastritis, gastric atrophy, and intestinal metaplasia.
Gastric Adenoma - Pathology
- Usually solitary lesions < 2 cm, commonly in the stomach antrum.
- Progression risk to adenocarcinoma increases with lesion size; ≥ 2 cm lesions show carcinoma in up to 30%.
- Majority consist of intestinal-type columnar epithelium.
Gastric Adenocarcinoma - Introduction
- Represents 90% of gastric cancers; classified as diffuse or intestinal types based on morphology.
- Highest incidence in Japan, Chile, Costa Rica, and Eastern Europe; 20-fold higher than in North America.
- North America has seen an 85% reduction in incidence since 1930, linked to lower H. pylori rates and reduced consumption of carcinogenic compounds.
Gastric Adenocarcinoma - Pathophysiology
- Develops in chronic inflammatory settings.
- Common mutations include p53 and E-cadherin loss; E-cadherin issues arise from germline mutations or hypermethylation.
- Intestinal type mutations often activate the Wnt signaling pathway.
Gastric Adenocarcinoma - Pathology
- Advanced cancers invade beneath the submucosa; classified into intestinal (glandular structures) and diffuse (mucous cells).
- Both pathways involve stepwise mutation accumulation; BRAF mutations are common.
Colonic Adenocarcinoma - Pathogenesis
- APC/β-catenin pathway accounts for 80% of sporadic colon tumors, initiating with mutations in the APC gene.
- Loss of APC function leads to β-catenin accumulation, promoting cell proliferation.
- Additional mutations arise, including KRAS and p53 mutations associated with chromosomal instability.
Colonic Adenocarcinoma - Microsatellite Instability Pathway
- Due to loss of mismatch repair genes, mutations accumulate in microsatellite repeats.
- Mutations may occur in genes regulating cell growth, including TGF-β receptors and pro-apoptotic proteins.
Hepatic Carcinoma - Clinical Features
- Symptoms include upper abdominal pain, fatigue, weight loss, and possible awareness of an abdominal mass.
- Enlarged liver may be palpable in many cases; prognosis for large tumors is poor, with most patients succumbing within two years.
- Early detection of lesions < 2 cm greatly improves survival rates.
Pancreatic Cancer - Ductal Adenocarcinoma
- Ductal adenocarcinoma is the primary type of pancreatic cancer and the 4th leading cause of cancer-related deaths.
Acid Suppressors
- Mechanism of Action: Target gastric acid production through various pathways including antagonism of receptors such as H2-R and M3-R on parietal cells.
- Adverse Effects: Potential for side effects like gastrointestinal disturbances, headaches, and dizziness; contraindications may include allergy to components or recent intestinal surgery.
- Naming Conventions: Recognizable suffixes include "tidine" for H2 blockers (e.g., Cimetidine, Ranitidine, Famotidine) and "prazole" for proton pump inhibitors (e.g., Omeprazole, Esomeprazole).
H2 Blockers
- Mechanism: Competitive blockade of H2 receptors on parietal cells reduces acid secretion.
- Therapeutic Uses: Effective for peptic ulcers, non-malignant gastric and duodenal ulcers, and Zollinger-Ellison syndrome.
- Associated Infections: Often used with "triple therapy" for H. pylori eradication.
- Comparison with Other Agents: Antacids may provide faster relief for acute scenarios than H2 blockers.
Proton Pump Inhibitors (PPIs)
- Mechanism: Inhibition of H+, K+-ATPase on gastric parietal cells reducing acid secretion.
- Therapeutic Uses: Similar to H2 blockers, indicated for ulcers, gastroesophageal reflux disease (GERD), and Zollinger-Ellison syndrome.
- First-Line Treatment: Commonly preferred in peptic ulcer triple therapy due to stronger acid suppression.
Prostaglandins and Analogs
- Mechanism of Action: Decrease proton pump activity and increase mucous and bicarbonate secretion, therefore providing gastric protection.
- Specific Agents: Misoprostol as a PGE1 analogue, mainly prevents NSAID-induced ulcers or GI bleed.
- Contraindications: Not recommended for use in pregnant women due to risk of uterine contractions.
Motility Agents
- Categories: Agents that decrease motility include Diphenoxylate-atropine and Loperamide; agents that increase motility include laxatives, Metoclopramide, and Domperidone.
Decreased Motility Agents
- Diphenoxylate-atropine: Opioid receptor agonist that inhibits acetylcholine (ACh) release in the enteric system, leading to reduced gut motility.
- Loperamide: Similar mechanism to diphenoxylate but without atropine; does not cross the blood-brain barrier, hence a lower risk of abuse.
Increased Motility Agents: Laxatives
- Types of Laxatives: Include bulking agents (e.g., bran, psyllium), osmotic laxatives (e.g., magnesium sulfate, lactulose), chemical stimulants (e.g., Senna), and stool softeners (e.g., mineral oil, sodium docusate).
Metoclopramide
- Increased Motility Mechanism: Blocks peripheral dopamine receptors boosting stimulative effects of ACh for peristalsis and lower esophageal sphincter tone.
- Antinausea Mechanism: Central blockade of D2 receptors in the medulla for antiemetic action.
- Therapeutic Uses: Effective for GERD, diabetic gastric stasis, and prevention of chemotherapy-induced nausea/vomiting.
General Notes
- Anticholinergics: Include scopolamine and promethazine, used for nausea.
- Dopamine-Receptor Blockers: Metoclopramide and Domperidone act as both motility enhancers and antiemetics.
- Common Anticholinergic Side Effects: Dry mouth, reduced gastrointestinal motility.
Summary Considerations
- Combination Therapy: Understanding interactions between these medications and their mechanisms is crucial for effective treatment of gastrointestinal disorders.
- Patient Awareness: Important for patients to recognize possible side effects and when to seek advice, especially using drugs with abuse potential (e.g., opioids in cyclic usage).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz focuses on important orthopedic conditions and assessment techniques covered in week 14. Students will learn to identify red and yellow flags, discuss pain sensation, and understand stages of injury and healing. Additionally, the quiz will cover normal and pathological end feels, as well as concepts such as muscle spasm and guarding.