Podcast
Questions and Answers
What is the main cause of periodontal disease?
What is the main cause of periodontal disease?
- Genetic and environmental factors (correct)
- Poor oral hygiene
- Presence of periodontopathogens
- Increased plaque accumulation
What is the role of periodontal epithelium in the host defense?
What is the role of periodontal epithelium in the host defense?
- Stimulating plaque accumulation
- Inducing bacterial proliferation
- Altering tissue homeostasis
- Physical barrier to infection (correct)
According to the text, what did the work of Löe and colleagues confirm about periodontal disease?
According to the text, what did the work of Löe and colleagues confirm about periodontal disease?
- Individuals with poor oral hygiene don't develop the disease
- There are variations in disease progression despite oral hygiene (correct)
- Poor oral hygiene is the primary cause
- Environmental factors are the main contributors
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is unique about the causative role of plaque bacteria in periodontal disease?
What is unique about the causative role of plaque bacteria in periodontal disease?
What structural defense mechanism helps prevent overt clinical signs of gingivitis from developing?
What structural defense mechanism helps prevent overt clinical signs of gingivitis from developing?
What is the primary cause of periodontal disease?
What is the primary cause of periodontal disease?
What distinguishes periodontitis from gingivitis?
What distinguishes periodontitis from gingivitis?
What is generally accepted to precede periodontitis?
What is generally accepted to precede periodontitis?
What is the net result of the inflammatory changes in periodontal disease?
What is the net result of the inflammatory changes in periodontal disease?
Which component of the periodontium is affected in gingivitis?
Which component of the periodontium is affected in gingivitis?
What additional tissues are affected in periodontitis compared to gingivitis?
What additional tissues are affected in periodontitis compared to gingivitis?
What is the main role of extracellular DNA (eDNA) in the development and structure of the biofilms formed by oral bacteria?
What is the main role of extracellular DNA (eDNA) in the development and structure of the biofilms formed by oral bacteria?
Which is a paradoxical aspect of tissue damage in periodontal disease?
Which is a paradoxical aspect of tissue damage in periodontal disease?
What is the initiating factor for the destructive inflammatory events in periodontitis?
What is the initiating factor for the destructive inflammatory events in periodontitis?
What role do prostaglandins (PGs) play in inflammation?
What role do prostaglandins (PGs) play in inflammation?
What is a characteristic of Matrix Metalloproteinases (MMPs)?
What is a characteristic of Matrix Metalloproteinases (MMPs)?
Which interleukin plays a key role in inflammation and immunity?
Which interleukin plays a key role in inflammation and immunity?
Which of the following is NOT a microbial virulence factor discussed in the text?
Which of the following is NOT a microbial virulence factor discussed in the text?
Which cell surface receptors recognize microbe-associated molecular patterns (MAMPs)?
Which cell surface receptors recognize microbe-associated molecular patterns (MAMPs)?
What do short-chain carboxylic acids such as butyric acid and propionic acid do?
What do short-chain carboxylic acids such as butyric acid and propionic acid do?
Which periodontal pathogen has an atypical form of lipopolysaccharides recognized by both TLR-2 and TLR-4?
Which periodontal pathogen has an atypical form of lipopolysaccharides recognized by both TLR-2 and TLR-4?
Which molecule stimulates nuclear factor (NF)- κβ and IL-8 in a gingival epithelial cell line via TLR-2?
Which molecule stimulates nuclear factor (NF)- κβ and IL-8 in a gingival epithelial cell line via TLR-2?
What stimulates immune cells via TLR-9, which recognizes hypomethylated CpG regions of the DNA?
What stimulates immune cells via TLR-9, which recognizes hypomethylated CpG regions of the DNA?
What histopathological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What histopathological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What characterizes the low-grade inflammation evident in clinically healthy gingival tissues?
What characterizes the low-grade inflammation evident in clinically healthy gingival tissues?
What is the predominant infiltrating cell type in the early lesion?
What is the predominant infiltrating cell type in the early lesion?
What is the defining histologic feature of the established lesion?
What is the defining histologic feature of the established lesion?
What marks the transition from gingivitis to periodontitis at a histologic level?
What marks the transition from gingivitis to periodontitis at a histologic level?
What facilitates the migration of neutrophils from the capillaries into the connective tissues in gingivitis?
What facilitates the migration of neutrophils from the capillaries into the connective tissues in gingivitis?
Which cytokine has the ability to induce either Th1 or Th2 differentiation, and is likely to play an important role in periodontal disease pathogenesis?
Which cytokine has the ability to induce either Th1 or Th2 differentiation, and is likely to play an important role in periodontal disease pathogenesis?
Which cytokine stimulates bone resorption and the development of osteoclasts, and is elevated in the cells, tissues, and GCF of patients with periodontal disease?
Which cytokine stimulates bone resorption and the development of osteoclasts, and is elevated in the cells, tissues, and GCF of patients with periodontal disease?
Which cytokine plays a fundamental role in immune responses, increases neutrophil activity, and mediates cell and tissue turnover in periodontal disease?
Which cytokine plays a fundamental role in immune responses, increases neutrophil activity, and mediates cell and tissue turnover in periodontal disease?
Which cytokine is primarily responsible for PGE2 production in the periodontium, induces the secretion of MMPs, and contributes significantly to the alveolar bone loss seen with periodontitis?
Which cytokine is primarily responsible for PGE2 production in the periodontium, induces the secretion of MMPs, and contributes significantly to the alveolar bone loss seen with periodontitis?
Which cytokine shares many of the cellular actions of IL-1β, stimulates the development of osteoclasts, and limits tissue repair via the induction of apoptosis in fibroblasts?
Which cytokine shares many of the cellular actions of IL-1β, stimulates the development of osteoclasts, and limits tissue repair via the induction of apoptosis in fibroblasts?
Which cytokine can induce either Th1 or Th2 response based on whether IL-12 is absent or present?
Which cytokine can induce either Th1 or Th2 response based on whether IL-12 is absent or present?
Which cytokine is secreted by activated macrophages as well as by other cell types, particularly in response to bacterial LPS, and its proinflammatory effects include the stimulation of endothelial cells to express selectins that facilitate leukocyte recruitment?
Which cytokine is secreted by activated macrophages as well as by other cell types, particularly in response to bacterial LPS, and its proinflammatory effects include the stimulation of endothelial cells to express selectins that facilitate leukocyte recruitment?
Which cytokine is a potential antagonist and acts as a transcriptional modulator by reducing the production of LPS-stimulated proinflammatory cytokines, supporting an anti-inflammatory role for this cytokine?
Which cytokine is a potential antagonist and acts as a transcriptional modulator by reducing the production of LPS-stimulated proinflammatory cytokines, supporting an anti-inflammatory role for this cytokine?
Which cytokine stimulates IL-4 and a Th2 response in the absence of IL-12?
Which cytokine stimulates IL-4 and a Th2 response in the absence of IL-12?
Which cytokine is less potent than IL-1β but increases as gingival inflammation develops, with higher levels found in individuals with periodontitis?
Which cytokine is less potent than IL-1β but increases as gingival inflammation develops, with higher levels found in individuals with periodontitis?
What role does extracellular DNA (eDNA) likely play in the development and structure of oral bacterial biofilms?
What role does extracellular DNA (eDNA) likely play in the development and structure of oral bacterial biofilms?
What is the paradoxical nature of tissue damage in periodontal disease?
What is the paradoxical nature of tissue damage in periodontal disease?
How do cytokines primarily act in the tissues in which they are produced?
How do cytokines primarily act in the tissues in which they are produced?
What is the main source of prostaglandin E2 (PGE2) in the periodontium?
What is the main source of prostaglandin E2 (PGE2) in the periodontium?
What is the significant role of Matrix Metalloproteinases (MMPs) in periodontal disease?
What is the significant role of Matrix Metalloproteinases (MMPs) in periodontal disease?
Which cytokine is closely linked to the innate immune response and stimulates the synthesis of other mediators contributing to inflammatory changes and tissue damage?
Which cytokine is closely linked to the innate immune response and stimulates the synthesis of other mediators contributing to inflammatory changes and tissue damage?
What are the major determinants of susceptibility to periodontal disease?
What are the major determinants of susceptibility to periodontal disease?
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is the unique characteristic of the causative role of plaque bacteria in periodontal disease?
What is the unique characteristic of the causative role of plaque bacteria in periodontal disease?
What additional tissues are affected in periodontitis compared to gingivitis?
What additional tissues are affected in periodontitis compared to gingivitis?
What is the role of periodontal epithelium in the host defense?
What is the role of periodontal epithelium in the host defense?
What marks the transition from gingivitis to periodontitis at a histologic level?
What marks the transition from gingivitis to periodontitis at a histologic level?
What are the histologic stages of gingivitis?
What are the histologic stages of gingivitis?
What is the defining feature of the transition from gingivitis to periodontitis at a histologic level?
What is the defining feature of the transition from gingivitis to periodontitis at a histologic level?
What is the process of alveolar bone destruction in periodontal diseases?
What is the process of alveolar bone destruction in periodontal diseases?
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is the paradoxical nature of the immune–inflammatory responses in periodontal disease?
What is the primary cause of periodontal disease?
What is the primary cause of periodontal disease?
What distinguishes periodontitis from gingivitis?
What distinguishes periodontitis from gingivitis?
What are the predominant infiltrating cell types in the established lesion?
What are the predominant infiltrating cell types in the established lesion?
What histological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What histological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What is the defining histological feature of the advanced lesion?
What is the defining histological feature of the advanced lesion?
What is the role of the junctional epithelium in the advanced lesion?
What is the role of the junctional epithelium in the advanced lesion?
What factors contribute to the transition from gingivitis to periodontitis?
What factors contribute to the transition from gingivitis to periodontitis?
What is the characteristic of the low-grade inflammation evident in clinically healthy gingival tissues?
What is the characteristic of the low-grade inflammation evident in clinically healthy gingival tissues?
What is the role of lipopolysaccharides (LPSs) in periodontal pathogenesis?
What is the role of lipopolysaccharides (LPSs) in periodontal pathogenesis?
How do short-chain carboxylic acids contribute to periodontal disease?
How do short-chain carboxylic acids contribute to periodontal disease?
What is the significance of Porphyromonas gingivalis' atypical form of lipopolysaccharides (LPSs)?
What is the significance of Porphyromonas gingivalis' atypical form of lipopolysaccharides (LPSs)?
How do bacterial fimbriae, particularly P. gingivalis fimbriae, impact the periodontium?
How do bacterial fimbriae, particularly P. gingivalis fimbriae, impact the periodontium?
What is the role of bacterial deoxyribonucleic acid (DNA) in periodontal disease?
What is the role of bacterial deoxyribonucleic acid (DNA) in periodontal disease?
How do plaque bacteria contribute directly to tissue damage in periodontal disease?
How do plaque bacteria contribute directly to tissue damage in periodontal disease?
What is the significance of IL-18 in periodontal disease pathogenesis?
What is the significance of IL-18 in periodontal disease pathogenesis?
How does TNF-α contribute to periodontal disease?
How does TNF-α contribute to periodontal disease?
What role does IL-6 play in periodontal pathogenesis?
What role does IL-6 play in periodontal pathogenesis?
How does prostaglandin E2 (PGE2) contribute to periodontal disease?
How does prostaglandin E2 (PGE2) contribute to periodontal disease?
What are the potential agonists and antagonists among the IL-1F cytokines?
What are the potential agonists and antagonists among the IL-1F cytokines?
How do IL-1F7 and IL-1F7b contribute to periodontal disease?
How do IL-1F7 and IL-1F7b contribute to periodontal disease?
What are the common signaling pathways shared by IL-6, IL-11, LIF, and oncostatin M?
What are the common signaling pathways shared by IL-6, IL-11, LIF, and oncostatin M?
What is the relationship between IL-18 and IL-12 in inducing T-helper cell responses?
What is the relationship between IL-18 and IL-12 in inducing T-helper cell responses?
What is the primary cause of periodontal disease?
What is the primary cause of periodontal disease?
What is the net result of the inflammatory changes in periodontal disease?
What is the net result of the inflammatory changes in periodontal disease?
Periodontal disease results from a complex interplay between the subgingival biofilm and the host immune–inflammatory events that develop in the gingival and periodontal tissues in response to the challenge presented by the ______.
Periodontal disease results from a complex interplay between the subgingival biofilm and the host immune–inflammatory events that develop in the gingival and periodontal tissues in response to the challenge presented by the ______.
It is generally accepted that gingivitis precedes ______, but it is clear that not all cases of gingivitis progress to periodontitis.
It is generally accepted that gingivitis precedes ______, but it is clear that not all cases of gingivitis progress to periodontitis.
With gingivitis, the inflammatory lesion is confined to the ______; however, with periodontitis, the inflammatory processes extend to additionally affect the periodontal ligament and the alveolar bone.
With gingivitis, the inflammatory lesion is confined to the ______; however, with periodontitis, the inflammatory processes extend to additionally affect the periodontal ligament and the alveolar bone.
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
Will be able to explain bacterial microbial virulence factors in the pathogenesis of ______ diseases.
Will be able to explain bacterial microbial virulence factors in the pathogenesis of ______ diseases.
Will be able to explain host-derived inflammatory mediators in the pathogenesis of ______ diseases.
Will be able to explain host-derived inflammatory mediators in the pathogenesis of ______ diseases.
The initial lesion typically develops within ______ days of the accumulation of plaque at a site that was otherwise free of plaque.
The initial lesion typically develops within ______ days of the accumulation of plaque at a site that was otherwise free of plaque.
The early lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of ______.
The early lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of ______.
The advanced lesion marks the transition from gingivitis to periodontitis. This transition is determined by many factors, the relative importance of which is currently unknown but which includes the bacterial challenge, the host inflammatory response, and susceptibility factors, including environmental and genetic risk factors. Histologic examination reveals continued evidence of ______ destruction that extends into the periodontal ligament and the alveolar bone.
The advanced lesion marks the transition from gingivitis to periodontitis. This transition is determined by many factors, the relative importance of which is currently unknown but which includes the bacterial challenge, the host inflammatory response, and susceptibility factors, including environmental and genetic risk factors. Histologic examination reveals continued evidence of ______ destruction that extends into the periodontal ligament and the alveolar bone.
The established lesion roughly corresponds with what clinicians would refer to as “chronic gingivitis.” The progression from the early lesion to the established lesion depends on many factors, including the plaque challenge, host susceptibility factors, and risk factors. In the initial work by Page and Schroeder, the established lesion was defined as being dominated by ______ cells.
The established lesion roughly corresponds with what clinicians would refer to as “chronic gingivitis.” The progression from the early lesion to the established lesion depends on many factors, including the plaque challenge, host susceptibility factors, and risk factors. In the initial work by Page and Schroeder, the established lesion was defined as being dominated by ______ cells.
The low-grade inflammation evident in clinically healthy gingival tissues is characterized by dilation of the vascular network and increased vascular permeability, thus permitting the neutrophils and monocytes from the gingival vasculature to migrate through the connective tissues toward the source of the chemotactic stimulus: the bacterial products in the gingival sulcus. The upregulation of adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1) and E-selectin in the gingival vasculature facilitates the migration of neutrophils from the capillaries into the connective tissues. The increased leakage of fluid from the vessels increases the hydrostatic pressure in the local microcirculation, and, as a result, GCF flow increases. Increased GCF flow has the effect of diluting bacterial products, and it also potentially has a flushing action to remove bacteria and their products from the crevice. However, given the nature of the bacterial biofilm, it is likely that only planktonic (free-floating) bacteria are removed in this way. The Early Lesion. The early lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of ______.
The low-grade inflammation evident in clinically healthy gingival tissues is characterized by dilation of the vascular network and increased vascular permeability, thus permitting the neutrophils and monocytes from the gingival vasculature to migrate through the connective tissues toward the source of the chemotactic stimulus: the bacterial products in the gingival sulcus. The upregulation of adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1) and E-selectin in the gingival vasculature facilitates the migration of neutrophils from the capillaries into the connective tissues. The increased leakage of fluid from the vessels increases the hydrostatic pressure in the local microcirculation, and, as a result, GCF flow increases. Increased GCF flow has the effect of diluting bacterial products, and it also potentially has a flushing action to remove bacteria and their products from the crevice. However, given the nature of the bacterial biofilm, it is likely that only planktonic (free-floating) bacteria are removed in this way. The Early Lesion. The early lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of ______.
The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. This marks the transition from gingivitis to periodontitis at a ______ level.
The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. This marks the transition from gingivitis to periodontitis at a ______ level.
Lipopolysaccharides (LPSs) are large molecules composed of a lipid component (lipid A) and a polysaccharide component. They are found in the outer membrane of __________ bacteria
Lipopolysaccharides (LPSs) are large molecules composed of a lipid component (lipid A) and a polysaccharide component. They are found in the outer membrane of __________ bacteria
TLRs are cell surface receptors that recognize __________ (MAMPs), which are conserved molecular structures located on diverse pathogens
TLRs are cell surface receptors that recognize __________ (MAMPs), which are conserved molecular structures located on diverse pathogens
TLR-4 recognizes LPSs from __________ bacteria and functions as part of a complex of cell surface molecules, including CD14 and MD-2
TLR-4 recognizes LPSs from __________ bacteria and functions as part of a complex of cell surface molecules, including CD14 and MD-2
Bacterial deoxyribonucleic acid (DNA) stimulates immune cells via ______, which recognizes hypomethylated CpG regions of the DNA. CpG sites are regions of DNA at which a cytosine nucleotide is found next to a guanine nucleotide (separated by a phosphate molecule, which links the C and G nucleotides together, hence “CpG”)
Bacterial deoxyribonucleic acid (DNA) stimulates immune cells via ______, which recognizes hypomethylated CpG regions of the DNA. CpG sites are regions of DNA at which a cytosine nucleotide is found next to a guanine nucleotide (separated by a phosphate molecule, which links the C and G nucleotides together, hence “CpG”)
Periodontal pathogens such as P. gingivalis and Aggregatibacter actinomycetemcomitans have been reported to invade the gingival tissues,including the __________ tissues
Periodontal pathogens such as P. gingivalis and Aggregatibacter actinomycetemcomitans have been reported to invade the gingival tissues,including the __________ tissues
P. gingivalis fimbriae stimulate immune responses, such as IL-6 secretion, and the major fimbrial structural component of P. gingivalis, FimA, has been shown to stimulate nuclear factor (NF)- κβ and IL-8 in a gingival epithelial cell line via __________
P. gingivalis fimbriae stimulate immune responses, such as IL-6 secretion, and the major fimbrial structural component of P. gingivalis, FimA, has been shown to stimulate nuclear factor (NF)- κβ and IL-8 in a gingival epithelial cell line via __________
IL-18 induces ______ and a Th2 response in the absence of IL-12
IL-18 induces ______ and a Th2 response in the absence of IL-12
TNF-α stimulates the development of ______ and limits tissue repair via the induction of apoptosis in fibroblasts
TNF-α stimulates the development of ______ and limits tissue repair via the induction of apoptosis in fibroblasts
IL-6 is elevated in the cells, tissues, and GCF of patients with periodontal disease and may have an influence on monocyte differentiation into ______ and a role in bone resorption
IL-6 is elevated in the cells, tissues, and GCF of patients with periodontal disease and may have an influence on monocyte differentiation into ______ and a role in bone resorption
PGE2 levels are increased in the tissues and the GCF at sites undergoing periodontal attachment loss. PGE2 induces the secretion of ______ as well as osteoclastic bone resorption
PGE2 levels are increased in the tissues and the GCF at sites undergoing periodontal attachment loss. PGE2 induces the secretion of ______ as well as osteoclastic bone resorption
IL-1F7b translocates to the nucleus of macrophages and may act as a transcriptional modulator by reducing the production of ______-stimulated proinflammatory cytokines
IL-1F7b translocates to the nucleus of macrophages and may act as a transcriptional modulator by reducing the production of ______-stimulated proinflammatory cytokines
IL-1F5 and IL-1F10 are potential ______
IL-1F5 and IL-1F10 are potential ______
TNF-α shares many of the cellular actions of IL-1β, stimulates the development of ______, and limits tissue repair via the induction of apoptosis in fibroblasts
TNF-α shares many of the cellular actions of IL-1β, stimulates the development of ______, and limits tissue repair via the induction of apoptosis in fibroblasts
IL-6 also has a key role in regulating the proliferation and differentiation of B cells and T cells, particularly the ______ subset
IL-6 also has a key role in regulating the proliferation and differentiation of B cells and T cells, particularly the ______ subset
IL-18 has the ability to induce either Th1 or Th2 differentiation, and it is likely to play an important role in periodontal disease pathogenesis due to its ability to induce either Th1 or ______ differentiation
IL-18 has the ability to induce either Th1 or Th2 differentiation, and it is likely to play an important role in periodontal disease pathogenesis due to its ability to induce either Th1 or ______ differentiation
TNF-α—although it possesses similar activity to IL-1β—has a less potent effect on ______
TNF-α—although it possesses similar activity to IL-1β—has a less potent effect on ______
Extracellular DNA (eDNA) likely plays a role in the development and structure of the biofilms formed by oral bacteria, and it has been identified as an important component of the matrix in a number of bacterial biofilms. Host-Derived Inflammatory Mediators The inflammatory and immune processes that develop in the periodontal tissues in response to the long-term presence of the subgingival biofilm are protective by intent but result in considerable ______ damage.
Extracellular DNA (eDNA) likely plays a role in the development and structure of the biofilms formed by oral bacteria, and it has been identified as an important component of the matrix in a number of bacterial biofilms. Host-Derived Inflammatory Mediators The inflammatory and immune processes that develop in the periodontal tissues in response to the long-term presence of the subgingival biofilm are protective by intent but result in considerable ______ damage.
It is paradoxical that the host response causes most of the tissue damage, although this is by no means unique to periodontal disease. For example, the tissue damage that occurs in the joints in patients with rheumatoid arthritis results from prolonged and excessive inflammatory responses, and it is characterized by the increased production of many of the cytokines that are known to be important in periodontal pathogenesis. In the case of rheumatoid arthritis, the initiating factor is an autoimmune response to structural components of the joint; in periodontitis, the initiating factor is the subgingival ______.
It is paradoxical that the host response causes most of the tissue damage, although this is by no means unique to periodontal disease. For example, the tissue damage that occurs in the joints in patients with rheumatoid arthritis results from prolonged and excessive inflammatory responses, and it is characterized by the increased production of many of the cytokines that are known to be important in periodontal pathogenesis. In the case of rheumatoid arthritis, the initiating factor is an autoimmune response to structural components of the joint; in periodontitis, the initiating factor is the subgingival ______.
Cytokines play a fundamental role in inflammation, and they are key inflammatory mediators in periodontal disease. They are soluble proteins, and they act as messengers to transmit signals from one cell to another. Cytokines bind to specific receptors on target cells, and they initiate intracellular signaling cascades that result in phenotypic changes in the cell via altered gene regulation. Cytokines are effective in very low concentrations, they are produced transiently in the tissues, and they primarily act locally in the tissues in which they are produced. Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
Cytokines play a fundamental role in inflammation, and they are key inflammatory mediators in periodontal disease. They are soluble proteins, and they act as messengers to transmit signals from one cell to another. Cytokines bind to specific receptors on target cells, and they initiate intracellular signaling cascades that result in phenotypic changes in the cell via altered gene regulation. Cytokines are effective in very low concentrations, they are produced transiently in the tissues, and they primarily act locally in the tissues in which they are produced. Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
MMPs are a family of proteolytic enzymes that degrade extracellular matrix molecules such as collagen, gelatin, and elastin. They are produced by a variety of cell types, including neutrophils, macrophages, fibroblasts, epithelial cells, osteoblasts, and osteoclasts. The nomenclature of MMPs has been based on the perception that each enzyme has its own specific substrate; for example, MMP-8 and MMP-1 are bot collagenases (i.e., they break down collagen). However, it is now appreciated that MMPs usually degrade multiple substrates, with significant substrate overlap between individual MMPs. The substrate-based classification is still used, however, and MMPs can be divided into collagenases, gelatinases/type IV collagenases, stromelysins, matrilysins, membrane-type metalloproteinases, and others. Role of Specific Inflammatory Mediators in Periodontal Disease Interleukin-1 Family Cytokines. The IL-1 family of cytokines comprises at least 11 members, including IL-1α, IL-1β, IL-1 receptor antagonist (IL-1Ra), IL-18, and IL-33.IL-1β plays a key role in inflammation and immunity; it is closely linked to the innate immune response, and it induces the synthesis and secretion of other mediators that contribute to inflammatory changes and ______ damage.
MMPs are a family of proteolytic enzymes that degrade extracellular matrix molecules such as collagen, gelatin, and elastin. They are produced by a variety of cell types, including neutrophils, macrophages, fibroblasts, epithelial cells, osteoblasts, and osteoclasts. The nomenclature of MMPs has been based on the perception that each enzyme has its own specific substrate; for example, MMP-8 and MMP-1 are bot collagenases (i.e., they break down collagen). However, it is now appreciated that MMPs usually degrade multiple substrates, with significant substrate overlap between individual MMPs. The substrate-based classification is still used, however, and MMPs can be divided into collagenases, gelatinases/type IV collagenases, stromelysins, matrilysins, membrane-type metalloproteinases, and others. Role of Specific Inflammatory Mediators in Periodontal Disease Interleukin-1 Family Cytokines. The IL-1 family of cytokines comprises at least 11 members, including IL-1α, IL-1β, IL-1 receptor antagonist (IL-1Ra), IL-18, and IL-33.IL-1β plays a key role in inflammation and immunity; it is closely linked to the innate immune response, and it induces the synthesis and secretion of other mediators that contribute to inflammatory changes and ______ damage.
IL-1β increases the expression of ICAM-1 on endothelial cells and stimulates the secretion of the chemokine CXCL8 (which is IL-8), thereby stimulating and facilitating the infiltration of neutrophils into the affected tissues. IL-1β also synergizes with other proinflammatory cytokines and PGE2 to induce ______ resorption. IL-1β has a role in adaptive immunity; it regulates the development of antigen-presenting cells (APCs) (e.g., dendritic cells), stimulates IL-6 secretion by macrophages (which in turn activates B cells), and has been shown to enhance the antigen-mediated stimulation of T cells.IL-18 interacts with IL-1β and shares many of the proinflammatory effects of IL-1β.It is mainly produced by stimulated monocytes and macrophages. There is increasing evidence to suggest that IL-18 plays a significant role in inflammation and immunity. IL-18 results in pro-inflammatory responses, including the activation of neutrophils.
IL-1β increases the expression of ICAM-1 on endothelial cells and stimulates the secretion of the chemokine CXCL8 (which is IL-8), thereby stimulating and facilitating the infiltration of neutrophils into the affected tissues. IL-1β also synergizes with other proinflammatory cytokines and PGE2 to induce ______ resorption. IL-1β has a role in adaptive immunity; it regulates the development of antigen-presenting cells (APCs) (e.g., dendritic cells), stimulates IL-6 secretion by macrophages (which in turn activates B cells), and has been shown to enhance the antigen-mediated stimulation of T cells.IL-18 interacts with IL-1β and shares many of the proinflammatory effects of IL-1β.It is mainly produced by stimulated monocytes and macrophages. There is increasing evidence to suggest that IL-18 plays a significant role in inflammation and immunity. IL-18 results in pro-inflammatory responses, including the activation of neutrophils.
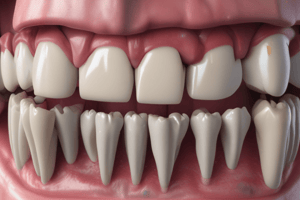
Periodontal disease is a chronic bacterial infection that affects the gingiva and bone that supports the teeth. This chronic inflammatory disease results from the host response to bacteria of dental biofilm. In addition to the presence of periodontopathogens; such as Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia; genetic and environmental factors seem to increase the susceptibility of some individuals in developing this severe inflammatory disease. Periodontal epithelium provides a physical barrier to infection and has an active role in the innate host defense. The epithelium can participate in the infection by signaling further innate and acquired immune responses. Epithelial cells may also respond to bacteria by increasing their proliferation, by altering their cell signaling events, and by changing the cell differentiation and cell death and altering tissue homeostasis. Langerhans cells and dendritic cells are located within the epithelium. They are a connecting link with acquired immunity. During the 1970s and 1980s, bacterial plaque was generally considered to be preeminent as the cause of periodontitis. At that time, it was accepted that poor oral hygiene resulted in increased plaque accumulation, which in turn resulted in periodontal disease. However, this model failed to take into account observations such as the fact that there are many individuals with poor oral hygiene who do not develop advanced periodontal disease and, conversely, that there are unfortunate individuals who, despite good oral hygiene and compliance with periodontal treatment protocols, continue to experience progressive periodontal breakdown and who would be considered to have aggressive periodontitis. These findings were confirmed by the work of Löe and colleagues, who studied Sri Lankan tea laborers who had no access to dental care and who could be divided into three main categories: 1.individuals (≈8% of the population studied) who had a rapid progression of periodontal disease; 2.those (≈81%) who had a moderate progression of such disease; and 3.those (≈11%) who demonstrated no progression of periodontal disease beyond gingivitis All patients in this population displayed abundant plaque and calculus deposits.
Periodontal disease is a chronic bacterial infection that affects the gingiva and bone that supports the teeth. This chronic inflammatory disease results from the host response to bacteria of dental biofilm. In addition to the presence of periodontopathogens; such as Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythia; genetic and environmental factors seem to increase the susceptibility of some individuals in developing this severe inflammatory disease. Periodontal epithelium provides a physical barrier to infection and has an active role in the innate host defense. The epithelium can participate in the infection by signaling further innate and acquired immune responses. Epithelial cells may also respond to bacteria by increasing their proliferation, by altering their cell signaling events, and by changing the cell differentiation and cell death and altering tissue homeostasis. Langerhans cells and dendritic cells are located within the epithelium. They are a connecting link with acquired immunity. During the 1970s and 1980s, bacterial plaque was generally considered to be preeminent as the cause of periodontitis. At that time, it was accepted that poor oral hygiene resulted in increased plaque accumulation, which in turn resulted in periodontal disease. However, this model failed to take into account observations such as the fact that there are many individuals with poor oral hygiene who do not develop advanced periodontal disease and, conversely, that there are unfortunate individuals who, despite good oral hygiene and compliance with periodontal treatment protocols, continue to experience progressive periodontal breakdown and who would be considered to have aggressive periodontitis. These findings were confirmed by the work of Löe and colleagues, who studied Sri Lankan tea laborers who had no access to dental care and who could be divided into three main categories: 1.individuals (≈8% of the population studied) who had a rapid progression of periodontal disease; 2.those (≈81%) who had a moderate progression of such disease; and 3.those (≈11%) who demonstrated no progression of periodontal disease beyond gingivitis All patients in this population displayed abundant plaque and calculus deposits.
The causative role of plaque bacteria is clear in that the bacteria initiate and perpetuate the inflammatory responses that develop in the gingival tissues. However, the major determinant of susceptibility to disease is the nature of the ______ responses themselves. It is paradoxical that these defensive processes, which are protective by intent (i.e., to prevent the ingress of the bacteria and their products into the tissues), result in the majority of tissue damage that leads to the clinical manifestations of disease. Periodontal disease is therefore a unique clinical entity. It is not an infection in the classic sense of the word. With most infections, a single infective organism causes the disease , and the identification of that organism provides the basis for the diagnosis. With periodontal disease, a large number of species are identifiable in the periodontal pocket, and many more are as yet unknown because they have not been cultured. It is impossible to conclude that a single species or even a group of species causes periodontal disease. Many of the species that are considered important in periodontal pathogenesis may simply reside in deep pockets because the pocket is a favorable environment in which they can survive.
The causative role of plaque bacteria is clear in that the bacteria initiate and perpetuate the inflammatory responses that develop in the gingival tissues. However, the major determinant of susceptibility to disease is the nature of the ______ responses themselves. It is paradoxical that these defensive processes, which are protective by intent (i.e., to prevent the ingress of the bacteria and their products into the tissues), result in the majority of tissue damage that leads to the clinical manifestations of disease. Periodontal disease is therefore a unique clinical entity. It is not an infection in the classic sense of the word. With most infections, a single infective organism causes the disease , and the identification of that organism provides the basis for the diagnosis. With periodontal disease, a large number of species are identifiable in the periodontal pocket, and many more are as yet unknown because they have not been cultured. It is impossible to conclude that a single species or even a group of species causes periodontal disease. Many of the species that are considered important in periodontal pathogenesis may simply reside in deep pockets because the pocket is a favorable environment in which they can survive.
Even in clinically healthy gingiva, the gingival connective tissue contains at least some inflammatory cells, particularly ______. Neutrophils continually migrate through the connective tissues and pass through the junctional epithelium to enter the sulcus or pocket. This low-grade inflammation occurs in response to the continued presence of bacteria and their products in the gingival crevice. The connective tissue component of the dentogingival unit contains densely packed collagen fiber bundles (a mixture of type I and III collagen fibers) that are arranged in distinct patterns that maintain the functional integrity of the tissues and the tight adaptation of the soft tissues to the teeth.
Even in clinically healthy gingiva, the gingival connective tissue contains at least some inflammatory cells, particularly ______. Neutrophils continually migrate through the connective tissues and pass through the junctional epithelium to enter the sulcus or pocket. This low-grade inflammation occurs in response to the continued presence of bacteria and their products in the gingival crevice. The connective tissue component of the dentogingival unit contains densely packed collagen fiber bundles (a mixture of type I and III collagen fibers) that are arranged in distinct patterns that maintain the functional integrity of the tissues and the tight adaptation of the soft tissues to the teeth.
Overt clinical signs of gingivitis (i.e., redness, swelling, and bleeding on probing) do not develop because of ______, including the following: The maintenance of an intact epithelial barrier (the junctional and sulcular epithelium) The outflow of GCF from the sulcus (dilution effect and flushing action) The sloughing (slafing) of surface epithelial cells of the junctional and sulcular epithelium The presence of neutrophils and macrophages in the sulcus that phagocytose bacteria The presence of antibodies in the GCF (although it is not clear whether these are effective) However, if plaque accumulation increases so that these defense mechanisms are overwhelmed, then inflammation and the classic clinical signs of gingivitis will develop.
Overt clinical signs of gingivitis (i.e., redness, swelling, and bleeding on probing) do not develop because of ______, including the following: The maintenance of an intact epithelial barrier (the junctional and sulcular epithelium) The outflow of GCF from the sulcus (dilution effect and flushing action) The sloughing (slafing) of surface epithelial cells of the junctional and sulcular epithelium The presence of neutrophils and macrophages in the sulcus that phagocytose bacteria The presence of antibodies in the GCF (although it is not clear whether these are effective) However, if plaque accumulation increases so that these defense mechanisms are overwhelmed, then inflammation and the classic clinical signs of gingivitis will develop.
The maintenance of an intact epithelial barrier (the junctional and sulcular epithelium) The outflow of GCF from the sulcus (dilution effect and flushing action) The sloughing (slafing) of surface epithelial cells of the junctional and sulcular epithelium The presence of neutrophils and macrophages in the sulcus that phagocytose bacteria The presence of antibodies in the GCF (although it is not clear whether these are effective) However, if plaque accumulation increases so that these defense mechanisms are overwhelmed, then inflammation and the classic clinical signs of gingivitis will develop.
The maintenance of an intact epithelial barrier (the junctional and sulcular epithelium) The outflow of GCF from the sulcus (dilution effect and flushing action) The sloughing (slafing) of surface epithelial cells of the junctional and sulcular epithelium The presence of neutrophils and macrophages in the sulcus that phagocytose bacteria The presence of antibodies in the GCF (although it is not clear whether these are effective) However, if plaque accumulation increases so that these defense mechanisms are overwhelmed, then inflammation and the classic clinical signs of gingivitis will develop.
The connective tissue component of the dentogingival unit contains densely packed collagen fiber bundles (a mixture of type I and III collagen fibers) that are arranged in distinct patterns that maintain the functional integrity of the tissues and the tight adaptation of the soft tissues to the teeth. These include the following: Dentogingival fibers (extend from the cementum into the free and attached gingiva) Alveologingival fibers (extend from the alveolar crest into the free and attached gingiva) Circular fibers (wrap around the tooth, maintain the close adaptation of the free gingiva to the tooth, and interweave with other collagen fiber bundles) Dentoperiosteal fibers (run from the cementum over the alveolar crest and insert into the alveolar process) Transseptal fibers (run interdentally from the cementum just apical to the junctional epithelium and over the alveolar crest, where they insert into the cementum of the neighboring tooth).
The connective tissue component of the dentogingival unit contains densely packed collagen fiber bundles (a mixture of type I and III collagen fibers) that are arranged in distinct patterns that maintain the functional integrity of the tissues and the tight adaptation of the soft tissues to the teeth. These include the following: Dentogingival fibers (extend from the cementum into the free and attached gingiva) Alveologingival fibers (extend from the alveolar crest into the free and attached gingiva) Circular fibers (wrap around the tooth, maintain the close adaptation of the free gingiva to the tooth, and interweave with other collagen fiber bundles) Dentoperiosteal fibers (run from the cementum over the alveolar crest and insert into the alveolar process) Transseptal fibers (run interdentally from the cementum just apical to the junctional epithelium and over the alveolar crest, where they insert into the cementum of the neighboring tooth).
TLR-4 recognizes LPSs from ______ bacteria and functions as part of a complex of cell surface molecules, including CD14 and MD-2
TLR-4 recognizes LPSs from ______ bacteria and functions as part of a complex of cell surface molecules, including CD14 and MD-2
The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. This marks the transition from gingivitis to periodontitis at a ______ level.
The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. This marks the transition from gingivitis to periodontitis at a ______ level.
Which cytokine stimulates bone resorption and the development of osteoclasts, and is elevated in the cells, tissues, and GCF of patients with periodontal disease?
Which cytokine stimulates bone resorption and the development of osteoclasts, and is elevated in the cells, tissues, and GCF of patients with periodontal disease?
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
What marks the transition from gingivitis to periodontitis at a histologic level?
What marks the transition from gingivitis to periodontitis at a histologic level?
Even in clinically healthy gingiva, the gingival connective tissue contains at least some inflammatory cells, particularly ______.
Even in clinically healthy gingiva, the gingival connective tissue contains at least some inflammatory cells, particularly ______.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
Cytokines play a fundamental role in inflammation, and they are key inflammatory mediators in periodontal disease. They are soluble proteins, and they act as messengers to transmit signals from one cell to another. Cytokines bind to specific receptors on target cells, and they initiate intracellular signaling cascades that result in phenotypic changes in the cell via altered gene regulation. Cytokines are effective in very low concentrations, they are produced transiently in the tissues, and they primarily act locally in the tissues in which they are produced. Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
Cytokines play a fundamental role in inflammation, and they are key inflammatory mediators in periodontal disease. They are soluble proteins, and they act as messengers to transmit signals from one cell to another. Cytokines bind to specific receptors on target cells, and they initiate intracellular signaling cascades that result in phenotypic changes in the cell via altered gene regulation. Cytokines are effective in very low concentrations, they are produced transiently in the tissues, and they primarily act locally in the tissues in which they are produced. Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
TNF-α stimulates the development of ______ and limits tissue repair via the induction of apoptosis in fibroblasts
TNF-α stimulates the development of ______ and limits tissue repair via the induction of apoptosis in fibroblasts
What histological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What histological change is observed in the tissues as a result of the accumulation of defense cells and their extracellular release of destructive enzymes?
What are the predominant infiltrating cell types in the established lesion?
What are the predominant infiltrating cell types in the established lesion?
What is the paradoxical aspect of tissue damage in periodontal disease?
What is the paradoxical aspect of tissue damage in periodontal disease?
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
The net result of these inflammatory changes is the breakdown of the fibers of the periodontal ligament, resulting in clinical loss of attachment together with resorption of the ______.
It is generally accepted that gingivitis precedes ______, but it is clear that not all cases of gingivitis progress to periodontitis.
It is generally accepted that gingivitis precedes ______, but it is clear that not all cases of gingivitis progress to periodontitis.
What additional tissues are affected in periodontitis compared to gingivitis?
What additional tissues are affected in periodontitis compared to gingivitis?
What is the process of alveolar bone destruction in periodontal diseases?
What is the process of alveolar bone destruction in periodontal diseases?
What marks the transition from gingivitis to periodontitis at a histologic level?
What marks the transition from gingivitis to periodontitis at a histologic level?
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
Extracellular DNA (eDNA) likely plays a role in the development and structure of the biofilms formed by oral bacteria, and it has been identified as an important component of the ______ in a number of bacterial biofilms.
Extracellular DNA (eDNA) likely plays a role in the development and structure of the biofilms formed by oral bacteria, and it has been identified as an important component of the ______ in a number of bacterial biofilms.
Host-Derived Inflammatory Mediators The inflammatory and immune processes that develop in the periodontal tissues in response to the long-term presence of the subgingival biofilm are protective by intent but result in considerable ______ damage.
Host-Derived Inflammatory Mediators The inflammatory and immune processes that develop in the periodontal tissues in response to the long-term presence of the subgingival biofilm are protective by intent but result in considerable ______ damage.
Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
Cytokines are able to induce their own expression in either an ______ or paracrine fashion, and they have pleiotropic effects (i.e., multiple biologic activities) on a large number of cell types.
PGE2 induces the secretion of ______ as well as osteoclastic bone resorption.
PGE2 induces the secretion of ______ as well as osteoclastic bone resorption.
TLRs are cell surface receptors that recognize ______ (MAMPs), which are conserved molecular structures located on diverse pathogens.
TLRs are cell surface receptors that recognize ______ (MAMPs), which are conserved molecular structures located on diverse pathogens.
What additional tissues are affected in periodontitis compared to gingivitis?
What additional tissues are affected in periodontitis compared to gingivitis?
The development of gingivitis is observed from a clinical perspective, with infiltration of the connective tissues by numerous defense cells, particularly neutrophils, macrophages, plasma cells, and lymphocytes. As a result of the accumulation of these defense cells and the extracellular release of their destructive enzymes, there is disruption of the normal anatomy of the connective tissues that results in collagen depletion and subsequent proliferation of the junctional epithelium. Vasodilation and increased vascular permeability lead to increased leakage of fluid out of the vessels and facilitate the passage of defense cells from the vasculature into the tissues, resulting in enlargement of the tissues, which appear erythematous and edematous. These changes are all reversible if the bacterial challenge is substantially reduced by improved oral hygiene. The described changes correspond to the ______ lesion of gingivitis.
The development of gingivitis is observed from a clinical perspective, with infiltration of the connective tissues by numerous defense cells, particularly neutrophils, macrophages, plasma cells, and lymphocytes. As a result of the accumulation of these defense cells and the extracellular release of their destructive enzymes, there is disruption of the normal anatomy of the connective tissues that results in collagen depletion and subsequent proliferation of the junctional epithelium. Vasodilation and increased vascular permeability lead to increased leakage of fluid out of the vessels and facilitate the passage of defense cells from the vasculature into the tissues, resulting in enlargement of the tissues, which appear erythematous and edematous. These changes are all reversible if the bacterial challenge is substantially reduced by improved oral hygiene. The described changes correspond to the ______ lesion of gingivitis.
The ______ lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of capillaries, the opening up of microvascular beds, and continued vasodilation. Increasing vascular permeability leads to increased GCF flow, and transmigrating neutrophils increase significantly in number. The predominant infiltrating cell types are neutrophils and lymphocytes (primarily thymic lymphocytes [T cells]), and the neutrophils migrate through the tissues to the sulcus and phagocytose bacteria. Fibroblasts degenerate, primarily via apoptosis (programmed cell death), which increases the space available for infiltrating leukocytes. The described changes correspond to the ______ lesion of gingivitis.
The ______ lesion develops after about 1 week of continued plaque accumulation and corresponds with the early clinical signs of gingivitis. The gingiva are erythematous in appearance as a result of the proliferation of capillaries, the opening up of microvascular beds, and continued vasodilation. Increasing vascular permeability leads to increased GCF flow, and transmigrating neutrophils increase significantly in number. The predominant infiltrating cell types are neutrophils and lymphocytes (primarily thymic lymphocytes [T cells]), and the neutrophils migrate through the tissues to the sulcus and phagocytose bacteria. Fibroblasts degenerate, primarily via apoptosis (programmed cell death), which increases the space available for infiltrating leukocytes. The described changes correspond to the ______ lesion of gingivitis.
The progression from the early lesion to the established lesion depends on many factors, including the plaque challenge (the composition and quantity of the biofilm), host susceptibility factors, and risk factors. In the initial work by Page and Schroeder, the established lesion was defined as being dominated by plasma cells. In human studies, reports have suggested that plasma cells predominate in established gingivitis in older subjects, whereas lymphocytes predominate in younger individuals. What is clear from all of the studies is that there is a significant inflammatory cell infiltrate in established gingivitis that occupies a considerable volume of the inflamed connective tissues. Large numbers of infiltrating cells can be identified adjacent and lateral to the junctional and sulcular epithelium, around blood vessels, and between collagen fiber bundles. The described changes correspond to the ______ lesion of gingivitis.
The progression from the early lesion to the established lesion depends on many factors, including the plaque challenge (the composition and quantity of the biofilm), host susceptibility factors, and risk factors. In the initial work by Page and Schroeder, the established lesion was defined as being dominated by plasma cells. In human studies, reports have suggested that plasma cells predominate in established gingivitis in older subjects, whereas lymphocytes predominate in younger individuals. What is clear from all of the studies is that there is a significant inflammatory cell infiltrate in established gingivitis that occupies a considerable volume of the inflamed connective tissues. Large numbers of infiltrating cells can be identified adjacent and lateral to the junctional and sulcular epithelium, around blood vessels, and between collagen fiber bundles. The described changes correspond to the ______ lesion of gingivitis.
The advanced lesion marks the transition from gingivitis to periodontitis, and is determined by factors such as the bacterial challenge, the host inflammatory response, and susceptibility factors, including environmental and genetic risk factors. Histologic examination reveals continued evidence of collagen destruction that extends into the periodontal ligament and the alveolar bone. Neutrophils predominate in the pocket epithelium and the periodontal pocket, and plasma cells dominate in the connective tissues. The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. The described changes correspond to the ______ lesion of gingivitis.
The advanced lesion marks the transition from gingivitis to periodontitis, and is determined by factors such as the bacterial challenge, the host inflammatory response, and susceptibility factors, including environmental and genetic risk factors. Histologic examination reveals continued evidence of collagen destruction that extends into the periodontal ligament and the alveolar bone. Neutrophils predominate in the pocket epithelium and the periodontal pocket, and plasma cells dominate in the connective tissues. The junctional epithelium migrates apically along the root surface into the collagen-depleted areas to maintain an intact epithelial barrier. The described changes correspond to the ______ lesion of gingivitis.
Periodontal pathogens such as P. gingivalis and Aggregatibacter actinomycetemcomitans have been reported to invade the gingival tissues, including the ______ tissues
Periodontal pathogens such as P. gingivalis and Aggregatibacter actinomycetemcomitans have been reported to invade the gingival tissues, including the ______ tissues
The prostaglandins (PGs) are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
The prostaglandins (PGs) are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
IL-18 has the ability to induce either Th1 or Th2 differentiation, and it is likely to play an important role in periodontal disease pathogenesis. Other Interleukin-1 Family Cytokines. Six new members of the IL-1 family (IL-1F) of cytokines have been identified on the basis of their sequence homology, structure, gene location, and receptor binding. Several of these cytokines were identified b different groups, who gave them a variety of names, and proposals were suggested for renaming all of the IL-1F cytokines in a more consistent manner, as indicated. Our knowledge of the role of these cytokines in inflammation and immunity is very limited at present, and some of these cytokines may be evolution arily redundant. IL-1F6, IL-1F8, and IL-1F are potential agonists (stimulating proinflammatory responses),19,182 whereas IL-1F5 and IL-1F10 are potential antagonists. IL-1F7 appears to have anti-inflammatory action. It has five splice variants and one isoform, IL-1F7b, which is highly expressed by monocytes and upregulated by LPS. An intracellular mode of action has been suggested for IL-1F7b; it translocates to the nucleus of macrophages, and it may act as a transcriptional modulator by reducing the production of LPS-stimulated proinflammatory cytokines, thus supporting an anti-inflammatory role for this cytokine Tumor Necrosis Factor-α. TNF-α is a key inflammatory mediator in periodontal disease, and it shares many of the cellular actions of IL-1β. It plays a fundamental role in immune responses, it increases neutrophil activity, and it mediates cell and tissue turnover by inducing MMP secretion. TNF-α stimulates the development of osteoclasts and limits tissue repair via the induction of apoptosis in fibroblasts. TNF-α is secreted by activated macrophages as well as by other cell types, particularly in response to bacterial LPS. The proinflammatory effects of TNF-α include the stimulation of endothelial cells to express selectins that facilitate leukocyte recruitment, the activation of macrophage IL-1β production, and the induction of PGE2 by macrophages and gingival fibroblasts.134 TNF-α—although it possesses similar activity to IL-1β—has a less potent effect on osteoclasts, and it is present at lower levels in inflamed gingival tissues than IL-1β.GCF levels of TNF-α increase as gingival inflammation develops, and higher levels are found in individuals with periodontitis. The importance of TNF-α (and IL-1β) in periodontal pathogenesis is unquestioned, and it has particularly been highlighted by studies showing that the application of antagonists to IL-1β and TNF-α resulted in an 80% reduction in recruitment of inflammatory cells in proximity to the alveolar bone and a 60% reduction in bone loss. Interleukin-6 and Related Cytokines. The cytokines in this group—which include IL-6, IL-11, leukemia-inhibitory factor (LIF), and oncostatin M—share common signaling pathways via signal transducers glycoprotein (gp) 130.74 IL-6 is the most extensively studied of this group, and it has pleiotropic proinflammatory properties.IL-6 secretion is stimulated by cytokines such as IL-1β and TNF-α, and it is produced by a range of immune cells (e.g., T cells, B cells, macrophages, dendritic cells) as well as resident cells (e.g., keratinocytes, endothelial cells, fibroblasts).IL-6 is also secreted by osteoblasts, and it stimulates bone resorption and the development of osteoclasts.81,94 IL-6 is elevated in the cells, tissues, and GCF of patients with periodontal disease., IL-6 may have an influence on monocyte differentiation into osteoclasts and a role in bone resorption in patients with periodontal disease.IL-6 also has a key role in regulating the proliferation and differentiation of B cells and T cells, particularly the Th17 subset.IL-6 therefore has an important role in periodontal pathogenesis, although it is less than that of IL-1β or TNF-α. Prostaglandin E2. The cells primarily responsible for PGE2 production in the periodontium are macrophages and fibroblasts. PGE2 levels are increased in the tissues and the GCF at sites undergoing periodontal attachment loss. PGE2 induces the secretion of MMPs as well as osteoclastic bone resorption, and it contributes significantly to the alveolar bone loss seen with periodontitis. PGE2 release from monocytes from patients with severe or aggressive periodontitis is greater than that from monocytes from patients who are periodontally healthy. A large body of evidence has demonstrated the importance of PGE2 in periodontal pathogenesis, and, given that prostaglandins are inhibited by nonsteroidal anti-inflammatory drugs (NSAIDs).
IL-18 has the ability to induce either Th1 or Th2 differentiation, and it is likely to play an important role in periodontal disease pathogenesis. Other Interleukin-1 Family Cytokines. Six new members of the IL-1 family (IL-1F) of cytokines have been identified on the basis of their sequence homology, structure, gene location, and receptor binding. Several of these cytokines were identified b different groups, who gave them a variety of names, and proposals were suggested for renaming all of the IL-1F cytokines in a more consistent manner, as indicated. Our knowledge of the role of these cytokines in inflammation and immunity is very limited at present, and some of these cytokines may be evolution arily redundant. IL-1F6, IL-1F8, and IL-1F are potential agonists (stimulating proinflammatory responses),19,182 whereas IL-1F5 and IL-1F10 are potential antagonists. IL-1F7 appears to have anti-inflammatory action. It has five splice variants and one isoform, IL-1F7b, which is highly expressed by monocytes and upregulated by LPS. An intracellular mode of action has been suggested for IL-1F7b; it translocates to the nucleus of macrophages, and it may act as a transcriptional modulator by reducing the production of LPS-stimulated proinflammatory cytokines, thus supporting an anti-inflammatory role for this cytokine Tumor Necrosis Factor-α. TNF-α is a key inflammatory mediator in periodontal disease, and it shares many of the cellular actions of IL-1β. It plays a fundamental role in immune responses, it increases neutrophil activity, and it mediates cell and tissue turnover by inducing MMP secretion. TNF-α stimulates the development of osteoclasts and limits tissue repair via the induction of apoptosis in fibroblasts. TNF-α is secreted by activated macrophages as well as by other cell types, particularly in response to bacterial LPS. The proinflammatory effects of TNF-α include the stimulation of endothelial cells to express selectins that facilitate leukocyte recruitment, the activation of macrophage IL-1β production, and the induction of PGE2 by macrophages and gingival fibroblasts.134 TNF-α—although it possesses similar activity to IL-1β—has a less potent effect on osteoclasts, and it is present at lower levels in inflamed gingival tissues than IL-1β.GCF levels of TNF-α increase as gingival inflammation develops, and higher levels are found in individuals with periodontitis. The importance of TNF-α (and IL-1β) in periodontal pathogenesis is unquestioned, and it has particularly been highlighted by studies showing that the application of antagonists to IL-1β and TNF-α resulted in an 80% reduction in recruitment of inflammatory cells in proximity to the alveolar bone and a 60% reduction in bone loss. Interleukin-6 and Related Cytokines. The cytokines in this group—which include IL-6, IL-11, leukemia-inhibitory factor (LIF), and oncostatin M—share common signaling pathways via signal transducers glycoprotein (gp) 130.74 IL-6 is the most extensively studied of this group, and it has pleiotropic proinflammatory properties.IL-6 secretion is stimulated by cytokines such as IL-1β and TNF-α, and it is produced by a range of immune cells (e.g., T cells, B cells, macrophages, dendritic cells) as well as resident cells (e.g., keratinocytes, endothelial cells, fibroblasts).IL-6 is also secreted by osteoblasts, and it stimulates bone resorption and the development of osteoclasts.81,94 IL-6 is elevated in the cells, tissues, and GCF of patients with periodontal disease., IL-6 may have an influence on monocyte differentiation into osteoclasts and a role in bone resorption in patients with periodontal disease.IL-6 also has a key role in regulating the proliferation and differentiation of B cells and T cells, particularly the Th17 subset.IL-6 therefore has an important role in periodontal pathogenesis, although it is less than that of IL-1β or TNF-α. Prostaglandin E2. The cells primarily responsible for PGE2 production in the periodontium are macrophages and fibroblasts. PGE2 levels are increased in the tissues and the GCF at sites undergoing periodontal attachment loss. PGE2 induces the secretion of MMPs as well as osteoclastic bone resorption, and it contributes significantly to the alveolar bone loss seen with periodontitis. PGE2 release from monocytes from patients with severe or aggressive periodontitis is greater than that from monocytes from patients who are periodontally healthy. A large body of evidence has demonstrated the importance of PGE2 in periodontal pathogenesis, and, given that prostaglandins are inhibited by nonsteroidal anti-inflammatory drugs (NSAIDs).
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.
The prostaglandins (PGs) are a group of lipid compounds derived from arachidonic acid, a polyunsaturated fatty acid found in the plasma membrane of most cells. Arachidonic acid is metabolized by cyclooxygenase-1 and -2 (COX-1 and COX-2) to generate a series of related compounds called the prostanoids, which includes the PGs, the thromboxanes, and the prostacyclins. PGs are important mediators of inflammation, particularly prostaglandin E2 (PGE2), which results in vasodilation and induces cytokine production by a variety of cell types. COX-2 is upregulated by IL-1β, TNF-α, and bacterial LPS, resulting in increased production of PGE2 in inflamed tissues. PGE2 is produced by various types of cells and most significantly in the periodontium by macrophages and fibroblasts. PGE2 results in the induction of MMPs and osteoclastic bone resorption, and it has a major role in contributing to the ______ damage that characterizes periodontitis.