Podcast
Questions and Answers
What is the primary function of the gastric alkaline barrier?
What is the primary function of the gastric alkaline barrier?
What is the role of carbonic anhydrase in HCl production?
What is the role of carbonic anhydrase in HCl production?
What is the source of H+ ions that are transported to the lumen of the stomach?
What is the source of H+ ions that are transported to the lumen of the stomach?
What is the primary component of the gastric alkaline barrier?
What is the primary component of the gastric alkaline barrier?
Signup and view all the answers
What is the effect of feeding on the gastric alkaline barrier?
What is the effect of feeding on the gastric alkaline barrier?
Signup and view all the answers
What is the primary goal of digestion in the human body?
What is the primary goal of digestion in the human body?
Signup and view all the answers
Which enzyme is responsible for breaking down polysaccharides into dextrins?
Which enzyme is responsible for breaking down polysaccharides into dextrins?
Signup and view all the answers
What happens to digested food molecules after digestion?
What happens to digested food molecules after digestion?
Signup and view all the answers
Which condition indicates a failure of absorption?
Which condition indicates a failure of absorption?
Signup and view all the answers
What type of carbohydrates must be broken down further during digestion?
What type of carbohydrates must be broken down further during digestion?
Signup and view all the answers
What is the main source of complex carbohydrates in the human diet?
What is the main source of complex carbohydrates in the human diet?
Signup and view all the answers
What is the term for the movement of digested food molecules through the intestinal walls?
What is the term for the movement of digested food molecules through the intestinal walls?
Signup and view all the answers
What role does salivary amylase play in the digestive process?
What role does salivary amylase play in the digestive process?
Signup and view all the answers
Which of the following statements describes the difference between the Gastric Phase and the Intestinal Phase of gastric acid secretion?
Which of the following statements describes the difference between the Gastric Phase and the Intestinal Phase of gastric acid secretion?
Signup and view all the answers
What is the primary role of the 'Reverse Enterogastric Reflex' in the context of gastric acid secretion?
What is the primary role of the 'Reverse Enterogastric Reflex' in the context of gastric acid secretion?
Signup and view all the answers
Which of the following hormones is NOT involved in inhibiting gastric acid secretion?
Which of the following hormones is NOT involved in inhibiting gastric acid secretion?
Signup and view all the answers
What is the primary role of enterokinase in protein digestion?
What is the primary role of enterokinase in protein digestion?
Signup and view all the answers
What is the primary function of pancreatic amylase in carbohydrate digestion?
What is the primary function of pancreatic amylase in carbohydrate digestion?
Signup and view all the answers
How does the secretion of bicarbonate ions (HCO3-) by pancreatic duct cells contribute to digestion?
How does the secretion of bicarbonate ions (HCO3-) by pancreatic duct cells contribute to digestion?
Signup and view all the answers
Which of the following statements BEST describes the relationship between HCl production and the 'Reverse Enterogastric Reflex'?
Which of the following statements BEST describes the relationship between HCl production and the 'Reverse Enterogastric Reflex'?
Signup and view all the answers
Which of the following scenarios would most likely activate the 'Reverse Enterogastric Reflex' and lead to a slowing down of gastric emptying?
Which of the following scenarios would most likely activate the 'Reverse Enterogastric Reflex' and lead to a slowing down of gastric emptying?
Signup and view all the answers
Which of the following cells are responsible for producing histamine, which in turn stimulates parietal cells to produce HCl?
Which of the following cells are responsible for producing histamine, which in turn stimulates parietal cells to produce HCl?
Signup and view all the answers
What is the function of 'Procarboxypeptidase', one of the pancreatic enzymes involved in protein digestion?
What is the function of 'Procarboxypeptidase', one of the pancreatic enzymes involved in protein digestion?
Signup and view all the answers
Which of the following statements accurately describes the 'Interdigestive' or 'Fasting' period in gastric secretion?
Which of the following statements accurately describes the 'Interdigestive' or 'Fasting' period in gastric secretion?
Signup and view all the answers
What is the significance of cellulose/fiber in the context of digestion?
What is the significance of cellulose/fiber in the context of digestion?
Signup and view all the answers
Which of the following enzymes is primarily responsible for breaking down fats into fatty acids and monoglycerides?
Which of the following enzymes is primarily responsible for breaking down fats into fatty acids and monoglycerides?
Signup and view all the answers
What is the primary role of 'Cholesterol esterase' in fat digestion?
What is the primary role of 'Cholesterol esterase' in fat digestion?
Signup and view all the answers
Which of the following statements BEST describes the relationship between the exocrine and endocrine functions of the pancreas?
Which of the following statements BEST describes the relationship between the exocrine and endocrine functions of the pancreas?
Signup and view all the answers
Which of the following stimuli would NOT likely trigger the release of pepsinogen and HCl in the stomach, even during the 'Interdigestive' period?
Which of the following stimuli would NOT likely trigger the release of pepsinogen and HCl in the stomach, even during the 'Interdigestive' period?
Signup and view all the answers
What role do bile salts play in the small intestine?
What role do bile salts play in the small intestine?
Signup and view all the answers
What is steatorrhea?
What is steatorrhea?
Signup and view all the answers
How are short-chain fatty acids absorbed in the body?
How are short-chain fatty acids absorbed in the body?
Signup and view all the answers
What occurs to long-chain fatty acids and monoglycerides once they enter enterocytes?
What occurs to long-chain fatty acids and monoglycerides once they enter enterocytes?
Signup and view all the answers
What effect does the drug orlistat have on lipid digestion?
What effect does the drug orlistat have on lipid digestion?
Signup and view all the answers
Where does the majority of lipid absorption take place in the digestive system?
Where does the majority of lipid absorption take place in the digestive system?
Signup and view all the answers
How do bile salts aid in lipid absorption?
How do bile salts aid in lipid absorption?
Signup and view all the answers
What is the primary cause of steatorrhea?
What is the primary cause of steatorrhea?
Signup and view all the answers
What is the primary enzyme responsible for breaking down dextrins in the small intestine?
What is the primary enzyme responsible for breaking down dextrins in the small intestine?
Signup and view all the answers
Which of the following products are formed from the digestion of sucrose?
Which of the following products are formed from the digestion of sucrose?
Signup and view all the answers
Where does the action of salivary amylase occur?
Where does the action of salivary amylase occur?
Signup and view all the answers
Which monosaccharides are produced from the digestion of lactose?
Which monosaccharides are produced from the digestion of lactose?
Signup and view all the answers
What is the role of disaccharidases at the brush border of enterocytes?
What is the role of disaccharidases at the brush border of enterocytes?
Signup and view all the answers
What happens to carbohydrates in the stomach?
What happens to carbohydrates in the stomach?
Signup and view all the answers
What are the final products absorbed in the GI tract from carbohydrate digestion?
What are the final products absorbed in the GI tract from carbohydrate digestion?
Signup and view all the answers
Which of the following enzymes is NOT a disaccharidase?
Which of the following enzymes is NOT a disaccharidase?
Signup and view all the answers
What type of molecules are dextrins composed of?
What type of molecules are dextrins composed of?
Signup and view all the answers
Which enzyme digests maltose into its monomer units?
Which enzyme digests maltose into its monomer units?
Signup and view all the answers
How do chloride ions primarily enter the bloodstream in the upper part of the small intestine?
How do chloride ions primarily enter the bloodstream in the upper part of the small intestine?
Signup and view all the answers
What role does bicarbonate play in the absorption of chloride in the large intestine?
What role does bicarbonate play in the absorption of chloride in the large intestine?
Signup and view all the answers
Which ions are absorbed actively through the intestinal mucosa?
Which ions are absorbed actively through the intestinal mucosa?
Signup and view all the answers
What determines the degree of iron absorption in the small intestine?
What determines the degree of iron absorption in the small intestine?
Signup and view all the answers
What mechanism do chloride ions use to exit the cells in the basal side of the intestinal wall?
What mechanism do chloride ions use to exit the cells in the basal side of the intestinal wall?
Signup and view all the answers
What happens to the electrical charge balance when chloride ions are absorbed?
What happens to the electrical charge balance when chloride ions are absorbed?
Signup and view all the answers
Which transporter is involved in chloride absorption in the ileum?
Which transporter is involved in chloride absorption in the ileum?
Signup and view all the answers
What is a characteristic of monovalent ions compared to bivalent ions in absorption?
What is a characteristic of monovalent ions compared to bivalent ions in absorption?
Signup and view all the answers
Which ion absorption in the small intestine is predominantly active?
Which ion absorption in the small intestine is predominantly active?
Signup and view all the answers
What is the primary method of chloride absorption in the upper part of the small intestine?
What is the primary method of chloride absorption in the upper part of the small intestine?
Signup and view all the answers
Flashcards
HCl production process
HCl production process
The process by which H2O in parietal cells dissociates into H+ and OH-, with H+ transported to the stomach lumen.
Gastric alkaline barrier
Gastric alkaline barrier
A protective barrier formed by mucus and bicarbonate in the stomach, maintaining a less acidic environment for the epithelial cells.
pH of stomach lumen
pH of stomach lumen
The acidity level of the stomach, which is approximately 2.0 due to the presence of HCl.
Active transport of H+
Active transport of H+
Signup and view all the flashcards
Hypokalemia
Hypokalemia
Signup and view all the flashcards
Digestion
Digestion
Signup and view all the flashcards
Absorption
Absorption
Signup and view all the flashcards
Cellulose digestion in humans
Cellulose digestion in humans
Signup and view all the flashcards
Polysaccharides
Polysaccharides
Signup and view all the flashcards
Salivary amylase
Salivary amylase
Signup and view all the flashcards
Monosaccharides
Monosaccharides
Signup and view all the flashcards
Main source of complex carbohydrates
Main source of complex carbohydrates
Signup and view all the flashcards
Dextrins
Dextrins
Signup and view all the flashcards
Gastric Phase
Gastric Phase
Signup and view all the flashcards
HCl Production
HCl Production
Signup and view all the flashcards
Parietal Cells
Parietal Cells
Signup and view all the flashcards
Peptic Cells
Peptic Cells
Signup and view all the flashcards
Gastrin
Gastrin
Signup and view all the flashcards
Enterogastric Reflex
Enterogastric Reflex
Signup and view all the flashcards
Secretin
Secretin
Signup and view all the flashcards
Glucose-dependent Insulinotropic Peptide (GIP)
Glucose-dependent Insulinotropic Peptide (GIP)
Signup and view all the flashcards
Vasoactive Intestinal Polypeptide (VIP)
Vasoactive Intestinal Polypeptide (VIP)
Signup and view all the flashcards
Somatostatin
Somatostatin
Signup and view all the flashcards
Pancreatic Enzymes
Pancreatic Enzymes
Signup and view all the flashcards
Amylase
Amylase
Signup and view all the flashcards
Lipase
Lipase
Signup and view all the flashcards
Active Enzymes
Active Enzymes
Signup and view all the flashcards
Pancreatic Amylase
Pancreatic Amylase
Signup and view all the flashcards
Disaccharidases
Disaccharidases
Signup and view all the flashcards
Maltose
Maltose
Signup and view all the flashcards
Sucrose
Sucrose
Signup and view all the flashcards
Lactose
Lactose
Signup and view all the flashcards
Brush Border
Brush Border
Signup and view all the flashcards
Carbohydrate Digestion Sites
Carbohydrate Digestion Sites
Signup and view all the flashcards
Enterocytes
Enterocytes
Signup and view all the flashcards
Bile Salts
Bile Salts
Signup and view all the flashcards
Micelles
Micelles
Signup and view all the flashcards
Steatorrhea
Steatorrhea
Signup and view all the flashcards
Short and Medium-Chain Fatty Acids
Short and Medium-Chain Fatty Acids
Signup and view all the flashcards
Long-Chain Fatty Acids
Long-Chain Fatty Acids
Signup and view all the flashcards
Lipase Inhibition
Lipase Inhibition
Signup and view all the flashcards
Orlistat
Orlistat
Signup and view all the flashcards
Chloride Ion Absorption
Chloride Ion Absorption
Signup and view all the flashcards
Role of Parathyroid Hormone
Role of Parathyroid Hormone
Signup and view all the flashcards
Cl–HCO3– Exchanger
Cl–HCO3– Exchanger
Signup and view all the flashcards
Chloride Diffusion Mechanism
Chloride Diffusion Mechanism
Signup and view all the flashcards
Bacterial Fermentation in Colon
Bacterial Fermentation in Colon
Signup and view all the flashcards
Ion Charge Neutrality
Ion Charge Neutrality
Signup and view all the flashcards
Calcium Absorption
Calcium Absorption
Signup and view all the flashcards
Iron Absorption
Iron Absorption
Signup and view all the flashcards
Potassium and Magnesium Absorption
Potassium and Magnesium Absorption
Signup and view all the flashcards
Monovalent vs. Bivalent Ions
Monovalent vs. Bivalent Ions
Signup and view all the flashcards
Study Notes
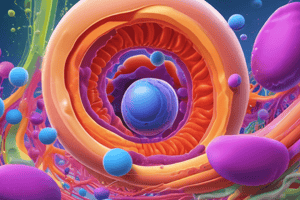
Gastrointestinal Secretions, Digestion & Absorption
- Gastrointestinal Secretions: Alimentary glands are primarily exocrine, with ducts releasing secretions into a space. Endocrine glands, in contrast, release hormones into the bloodstream. Different gland types exist, including mucous glands (goblet cells), specialized secretory cells (like in Crypts of Lieberkühn), deep tubular glands (e.g., oxyntic glands), and complex compound acinous glands (pancreas, liver, and salivary glands).
Saliva
-
Saliva Secretion: Occurs in two stages: acinar (with isotonic plasma-like levels of ions and containing ptyalin and mucus) and salivary duct (with decreased tonicity due to ion transport).
-
Salivary Glands: Varied in type and function, including parotid (mostly serous), sublingual (mixed), submandibular (mixed), and buccal (mucus only) glands.
-
Stimuli for Secretion: Tactile stimuli (food touching the pharynx), chemical irritation, gut wall distension, and autonomic/hormonal stimulation.
Stomach
-
Stomach Glands: The stomach contains glands, primarily oxyntic and pyloric, producing substances like mucus, HCl, intrinsic factor, and pepsinogen.
-
Oxyntic Glands: Located in the body and fundus, primarily responsible for producing HCl through active transport, producing intrinsic factor, and secreting pepsinogen.
-
Pyloric Glands: Located in the antrum, primarily secreting mucus and gastrin (a hormone).
-
Gastric Secretion: Occurs in three stages: cephalic (brain signals), gastric (food in stomach/local), and intestinal (chyme in small intestine). The initial stages are major stimulators.
-
HCl Production: Parietal cells release H+ ions through a proton pump, combining with Cl- to result in HCl.
-
Gastric Alkaline Barrier: Mucus and bicarbonate protect the stomach lining from autodigestion.
-
Protein Digestion: Pepsin begins protein digestion in the acidic stomach environment.
Pancreas
-
Pancreatic Secretions: Exocrine glands producing various enzymes (e.g., amylase, trypsin, chymotrypsin, lipase, etc.) and bicarbonate/water. These enzymes break down carbohydrates, proteins, and fats.
-
Pancreatic Duct/Ductules: Produce water and bicarbonate for neutralization.
Small Intestines
-
Brunner's Glands: Mucous glands in the duodenum secrete alkaline mucus to protect the intestinal lining.
-
Crypts of Lieberkühn: In the small intestines, these glands secrete digestive enzymes.
-
Brush Border Enzymes: Digestive enzymes on the surface of small intestine cells, breaking down disaccharides and peptides.
Large Intestines
- Large Intestine Secretion: Mucus secretion is regulated locally by tactile stimulation and nervous reflexes.
Digestion & Absorption (General)
-
Digestion: Breakdown of food into absorbable molecules via mechanical and chemical means.
-
Absorption: Movement of digested food molecules from the GI tract into the bloodstream. This often involves transporters, which can be active or passive.
Carbohydrate Absorption
-
Site of Digestion: Mouth (salivary amylase), and the duodenum (pancreatic amylase). Disaccharidases on the brush border finish carbohydrate digestion in the small intestine.
-
Carbohydrate Absorption: Products of digestion (monosaccharides) are transported across the intestinal wall, primarily through SGLT1 (sodium-glucose transporter 1) and GLUT2 (glucose transporter 2). Glucose and galactose use SGLT1 while fructose enters via GLUT5.
Protein Digestion and Absorption
- Protein Digestion: Pepsin in the stomach initiates digestion. Pancreatic proteases break proteins into peptides (and some amino acids) . Brush border enzymes convert the peptides into amino acids, which are transported actively (or sometimes passively) into the cells lining the intestines.
Fat Digestion and Absorption
-
Fat Digestion: Lingual lipase in the stomach begins fat digestion, but the major enzymes are pancreatic lipases. Bile salts aid by emulsifying fats and forming micelles. Micelles facilitate breakdown and absorption of fatty acids and glycerol.
-
Fat Absorption: These fats are absorbed into the epithelial cells via passive and facilitated diffusion. These lipids are combined with proteins to become chylomicrons, which enter the lacteals and eventually the bloodstream.
Other
-
Water Absorption: Absorption of water occurs in the small and large intestines, with large amounts occurring in the small intestine. Water follows the osmotic gradient created by substances like sodium.
-
Ion Absorption: Ions like sodium, chloride, and bicarbonate are absorbed both transcellularly and paracellularly using channels and transporters.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores crucial aspects of human digestion, including the gastric alkaline barrier, the role of enzymes, and nutrient absorption. Learn about the physiological functions that aid in breaking down food and the processes involved in nutrient transport. Test your knowledge on the digestive system's mechanisms and phases.