Podcast
Questions and Answers
Which condition is directly associated with the development of adenocarcinomas in the colon?
Which condition is directly associated with the development of adenocarcinomas in the colon?
Which type of hernia is characterized by the stomach protruding into the thorax but does not typically involve strangulation?
Which type of hernia is characterized by the stomach protruding into the thorax but does not typically involve strangulation?
Which gastrointestinal cancer is most commonly associated with malnutrition and chronic reflux?
Which gastrointestinal cancer is most commonly associated with malnutrition and chronic reflux?
Which dietary habit is a known risk factor for the development of gastric adenocarcinoma?
Which dietary habit is a known risk factor for the development of gastric adenocarcinoma?
Signup and view all the answers
What clinical manifestation might indicate the presence of colorectal cancer?
What clinical manifestation might indicate the presence of colorectal cancer?
Signup and view all the answers
Which of the following disorders is characterized by recurrent abdominal pain with altered bowel habits?
Which of the following disorders is characterized by recurrent abdominal pain with altered bowel habits?
Signup and view all the answers
What mechanism may contribute to constipation-predominant irritable bowel syndrome (IBS-C)?
What mechanism may contribute to constipation-predominant irritable bowel syndrome (IBS-C)?
Signup and view all the answers
Which of the following is NOT a potential cause of secondary constipation?
Which of the following is NOT a potential cause of secondary constipation?
Signup and view all the answers
Which symptom would most likely indicate gastroesophageal reflux disease (GERD)?
Which symptom would most likely indicate gastroesophageal reflux disease (GERD)?
Signup and view all the answers
Which gastrointestinal condition is illustrated by an abnormality in lower esophageal sphincter function?
Which gastrointestinal condition is illustrated by an abnormality in lower esophageal sphincter function?
Signup and view all the answers
Which of the following mechanisms is associated with enhanced sensitivity in the gut in IBS sufferers?
Which of the following mechanisms is associated with enhanced sensitivity in the gut in IBS sufferers?
Signup and view all the answers
Which factor is least likely to contribute to the development of constipation?
Which factor is least likely to contribute to the development of constipation?
Signup and view all the answers
In which gastrointestinal disorder may abnormal GI motility present as rapid colonic transit times?
In which gastrointestinal disorder may abnormal GI motility present as rapid colonic transit times?
Signup and view all the answers
What are the clinical manifestations of chronic pancreatitis?
What are the clinical manifestations of chronic pancreatitis?
Signup and view all the answers
Which condition is characterized by chronic, debilitating inflammation of the gastrointestinal tract?
Which condition is characterized by chronic, debilitating inflammation of the gastrointestinal tract?
Signup and view all the answers
Which of the following is a consequence of cholelithiasis?
Which of the following is a consequence of cholelithiasis?
Signup and view all the answers
What is a major cause of peptic ulcer disease?
What is a major cause of peptic ulcer disease?
Signup and view all the answers
Which factor is not associated with the development of cholelithiasis?
Which factor is not associated with the development of cholelithiasis?
Signup and view all the answers
What characterizes a sliding hiatal hernia?
What characterizes a sliding hiatal hernia?
Signup and view all the answers
Which statement accurately describes Crohn's disease in comparison to Ulcerative Colitis?
Which statement accurately describes Crohn's disease in comparison to Ulcerative Colitis?
Signup and view all the answers
Which of the following symptoms is NOT typically associated with gastritis?
Which of the following symptoms is NOT typically associated with gastritis?
Signup and view all the answers
Which symptom is commonly observed in patients with cholecystitis?
Which symptom is commonly observed in patients with cholecystitis?
Signup and view all the answers
Which medications are often implicated in causing gastritis?
Which medications are often implicated in causing gastritis?
Signup and view all the answers
What is a distinguishing feature of diverticulitis compared to diverticulosis?
What is a distinguishing feature of diverticulitis compared to diverticulosis?
Signup and view all the answers
Which condition can be a complication of untreated cholecystitis?
Which condition can be a complication of untreated cholecystitis?
Signup and view all the answers
In which condition does the mechanism involve an imbalance between gastric mucosal protective and destructive factors?
In which condition does the mechanism involve an imbalance between gastric mucosal protective and destructive factors?
Signup and view all the answers
Which symptom is NOT typically associated with appendicitis?
Which symptom is NOT typically associated with appendicitis?
Signup and view all the answers
Which symptom is commonly associated with lipase overproduction in the case of pancreatitis, contrasting other GI disorders?
Which symptom is commonly associated with lipase overproduction in the case of pancreatitis, contrasting other GI disorders?
Signup and view all the answers
What underlying factor contributes to the inflammation seen in cholecystitis?
What underlying factor contributes to the inflammation seen in cholecystitis?
Signup and view all the answers
During which phase does the clinical course of viral hepatitis begin?
During which phase does the clinical course of viral hepatitis begin?
Signup and view all the answers
Which complication is most closely associated with Ulcerative Colitis?
Which complication is most closely associated with Ulcerative Colitis?
Signup and view all the answers
What is the hallmark symptom of ulcerative colitis?
What is the hallmark symptom of ulcerative colitis?
Signup and view all the answers
What is a primary clinical sign of acute pancreatitis?
What is a primary clinical sign of acute pancreatitis?
Signup and view all the answers
Which of the following symptoms is least likely to be associated with a hiatal hernia?
Which of the following symptoms is least likely to be associated with a hiatal hernia?
Signup and view all the answers
Which of the following is NOT a typical treatment consideration for inflammatory bowel disease?
Which of the following is NOT a typical treatment consideration for inflammatory bowel disease?
Signup and view all the answers
What is the common cause identified for appendicitis?
What is the common cause identified for appendicitis?
Signup and view all the answers
Which of the following statements regarding gallstones is accurate?
Which of the following statements regarding gallstones is accurate?
Signup and view all the answers
Which characteristic is NOT true for Crohn's disease?
Which characteristic is NOT true for Crohn's disease?
Signup and view all the answers
Which condition involves the possibility of developing mucosal atrophy and metaplasia over time?
Which condition involves the possibility of developing mucosal atrophy and metaplasia over time?
Signup and view all the answers
What is a common complication of untreated peptic ulcer disease?
What is a common complication of untreated peptic ulcer disease?
Signup and view all the answers
Which symptom of viral hepatitis typically progresses as the infection develops?
Which symptom of viral hepatitis typically progresses as the infection develops?
Signup and view all the answers
Which of the following symptoms is characteristic of both Crohn's disease and Ulcerative Colitis?
Which of the following symptoms is characteristic of both Crohn's disease and Ulcerative Colitis?
Signup and view all the answers
What generally distinguishes diverticulosis from diverticulitis?
What generally distinguishes diverticulosis from diverticulitis?
Signup and view all the answers
Study Notes
Osmotic Diarrhea
- Occurs when a nonabsorbable substance in the intestines draws excess water into the intestinal lumen, increasing stool weight and volume.
- Results in large-volume diarrhea.
- Causes include:
- Large doses of poorly absorbed ions (magnesium, sulfate, phosphate).
- Excessive ingestion of nonabsorbable sugars.
- Introduction of full-strength tube feeding formulas.
- Dumping syndrome.
- Lactase deficiency.
- Pancreatic enzyme or bile salt deficiency.
- Small intestine bacterial overgrowth.
- Celiac disease.
Secretory Diarrhea
- A form of large-volume diarrhea caused by excessive mucosal secretions of chloride or bicarbonate-rich fluid or the inhibition of sodium absorption.
- Infectious causes include:
- Viruses (e.g., rotavirus).
- Bacterial enterotoxins (e.g., Escherichia coli, Vibrio cholerae).
- Exotoxins (e.g., Clostridioides difficile following antibiotic therapy).
- Small bowel bacterial overgrowth.
- These infections cause the secretion of transmitters from enteroendocrine cells, activation of afferent neurons, and altered sodium and chloride transport.
Constipation
- Difficult or infrequent defecation.
- Defined as a decrease in the number of bowel movements per week, hard stools, straining, abdominal pain, and difficult evacuation.
- Can be primary or secondary.
- Primary (idiopathic) constipation is broadly categorized into three groups.
Secondary Constipation
- Causes include:
- Diet
- Medications
- Neurogenic disorders
- Rectal fissures, strictures, or hemorrhoids
- Endocrine or metabolic disorders
- Pelvic hiatal hernia
- Diverticula
- Irritable bowel syndrome (IBS)
- Pregnancy
- Aging
- Pain or weakness of the abdominal muscles
- Depression
Irritable Bowel Syndrome (IBS)
- A disorder of brain-gut interaction characterized by recurrent abdominal pain with altered bowel habits.
- Mechanisms may include:
- Visceral hypersensitivity (nerves in the gut are more sensitive).
- Abnormal GI motility (rapid or delayed transit times).
- Altered gut microbiota (different bacterial composition).
- Immune activation (immune system may be involved).
- Psychosocial factors (stress and anxiety).
Gastroesophageal Reflux Disease (GERD)
- Reflux of acid, pepsin, or bile salts from the stomach to the esophagus.
- Causes esophagitis and can affect daily functioning.
- Risk factors include:
- Increasing age
- Obesity
- Hiatal hernias
- Drugs (e.g., anticholinergics, nitrates, calcium channel blockers, nicotine)
- Prematurity
- Neurologic impairment
- Esophageal atresia
- Achalasia
- Chronic lung diseases
- Certain genetic disorders (e.g., cystic fibrosis).
Clinical Manifestations of GERD
- Adults: heartburn, acid regurgitation, dysphagia, chest pain, chronic cough, asthma attacks, laryngitis, hoarseness, upper abdominal pain within one hour of eating.
- Infants: irritability, sleep disturbance, excessive regurgitation, vomiting, unexplained crying, back arching, failure to thrive.
- Children: similar to adult manifestations, but may also include decreased food intake, weight loss, abdominal or epigastric pain, heartburn, regurgitation.
Gastritis and Peptic Ulcer Disease (PUD)
- Gastritis: Nonspecific inflammatory disorder of the gastric mucosa (acute or chronic).
- PUD: Ulceration of the lower esophagus, stomach, or duodenum (acute or chronic).
- Causes: medications (NSAIDs), excessive alcohol use, chemotherapy, Helicobacter pylori infections, autoimmune reactions, chronic alcohol use.
- Mechanism: injury to the protective mucosal barrier, chronic inflammation, mucosal atrophy, metaplasia.
- Symptoms: Epigastric discomfort, nausea, vomiting, belching, loss of appetite, acute abdominal pain.
Crohn's Disease and Ulcerative Colitis
- Inflammatory bowel diseases (IBDs) with chronic, debilitating, relapsing, and remitting inflammation of the gastrointestinal tract.
- Crohn's disease: affects any portion of the GI tract from the mouth to the perianal area, typically the terminal ileum and proximal colon, and may manifest as lesions anywhere along the GI tract.
- Ulcerative colitis: lesions are limited to the colon and rectum.
Diverticulitis and Diverticulosis
- Diverticula: sac-like outpouchings of the mucosa and submucosa through the muscle layers of the colon (usually the sigmoid colon).
- Diverticulosis: asymptomatic diverticular disease.
- Diverticulitis: inflammation of the diverticula.
- Appendicitis: inflammation of the vermiform appendix (a projection from the apex of the cecum).
Viral Hepatitis
- Viral infection of the liver, with varying clinical courses, including an incubation phase, prodromal (preicteric) phase, and icteric phase.
- Hepatitis can be transmitted through the faecal-oral route (HAV) and/or through blood-borne pathogens (HBV, HCV, HDV) via contact with contaminated blood, sexual transmission, or blood products.
Acute and Chronic Pancreatitis
- Pancreatitis: inflammation of the pancreas.
- Risk factors: obstructive biliary tract disease, alcoholism, obesity, peptic ulcers, trauma, hyperlipidemia, hypercalcemia, smoking, certain drugs, genetic factors.
- Causes of acute pancreatitis: obstruction of pancreatic digestive enzyme outflow, gallstones, cellular injury from alcohol, drugs, and viral infection..
Cholelithiasis and Cholecystitis
- Cholelithiasis: presence of gallstones in the biliary tract, which can form due to impaired metabolism of cholesterol, bilirubin, and bile acids and can cause inflammation of the gallbladder (cholecystitis).
- Cholecystitis: inflammation of the gallbladder. Causes include impaired metabolism of cholesterol, bilirubin, and bile acids and hypomotility of the gallbladder
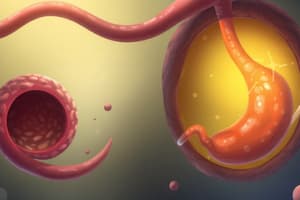
Sliding and Paraesophageal Hiatal Hernias
- Hiatal hernias: protrusion or bulging of an abdominal structure (e.g., stomach) into the thoracic cavity.
- Sliding hiatal hernia (type 1): the proximal stomach moves into the thoracic cavity, through the esophageal hiatus.
- Paraesophageal hiatal hernia (type 2): greater curvature of the stomach herniates through a secondary opening in the diaphragm above the diaphragm.
Gastrointestinal Cancers
- Risk factors, pathophysiological mechanisms, and clinical manifestations of cancers of the colon and rectum, as well as others.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the mechanisms and causes of osmotic and secretory diarrhea. It explores the differences between these types, their clinical implications, and common causes. Perfect for medical students and healthcare professionals looking to test their knowledge on gastrointestinal disorders.