Podcast
Questions and Answers
What characterizes a mature follicle?
What characterizes a mature follicle?
What is the process called that most ovarian follicles undergo?
What is the process called that most ovarian follicles undergo?
How long does it typically take for a follicle to mature from a primordial stage?
How long does it typically take for a follicle to mature from a primordial stage?
Which of the following statements about a mature follicle is false?
Which of the following statements about a mature follicle is false?
Signup and view all the answers
What happens to the majority of ovarian follicles during their development?
What happens to the majority of ovarian follicles during their development?
Signup and view all the answers
What is the process called by which many primary oocytes are lost?
What is the process called by which many primary oocytes are lost?
Signup and view all the answers
Approximately how many oocytes do the ovaries contain at puberty?
Approximately how many oocytes do the ovaries contain at puberty?
Signup and view all the answers
Which of the following best describes the fate of primary oocytes over time?
Which of the following best describes the fate of primary oocytes over time?
Signup and view all the answers
At what stage in life does the decline of primary oocytes through atresia become particularly notable?
At what stage in life does the decline of primary oocytes through atresia become particularly notable?
Signup and view all the answers
Which statement about primary oocytes is true?
Which statement about primary oocytes is true?
Signup and view all the answers
What is the role of the components mentioned in the content with respect to sperm?
What is the role of the components mentioned in the content with respect to sperm?
Signup and view all the answers
How do the components influence sperm functionality?
How do the components influence sperm functionality?
Signup and view all the answers
What process is induced by the binding of the components to sperm proteins?
What process is induced by the binding of the components to sperm proteins?
Signup and view all the answers
Why is acrosomal activation important for sperm?
Why is acrosomal activation important for sperm?
Signup and view all the answers
What could potentially happen if the binding of sperm receptors is disrupted?
What could potentially happen if the binding of sperm receptors is disrupted?
Signup and view all the answers
What is primarily accumulated in the single large antrum of a mature or graafian follicle?
What is primarily accumulated in the single large antrum of a mature or graafian follicle?
Signup and view all the answers
What is the typical diameter of a mature follicle when it is fully expanded?
What is the typical diameter of a mature follicle when it is fully expanded?
Signup and view all the answers
What physical feature does a mature follicle exhibit on the ovary?
What physical feature does a mature follicle exhibit on the ovary?
Signup and view all the answers
During follicle development, what is the significance of the rapid accumulation of follicular fluid?
During follicle development, what is the significance of the rapid accumulation of follicular fluid?
Signup and view all the answers
Which of the following statements about mature follicles is true?
Which of the following statements about mature follicles is true?
Signup and view all the answers
What is the role of leukocytes in the menstrual cycle?
What is the role of leukocytes in the menstrual cycle?
Signup and view all the answers
Which part of the endometrium is primarily affected during menstruation?
Which part of the endometrium is primarily affected during menstruation?
Signup and view all the answers
How does arterial constriction affect menstruation?
How does arterial constriction affect menstruation?
Signup and view all the answers
Which components are typically sloughed away during menstruation?
Which components are typically sloughed away during menstruation?
Signup and view all the answers
What happens at the open ends of venules during menstruation?
What happens at the open ends of venules during menstruation?
Signup and view all the answers
What is the primary function of the endocervical mucosa?
What is the primary function of the endocervical mucosa?
Signup and view all the answers
How does the thickness of the cervix change during the ovarian cycle?
How does the thickness of the cervix change during the ovarian cycle?
Signup and view all the answers
What type of epithelium lines the vagina?
What type of epithelium lines the vagina?
Signup and view all the answers
What significant change occurs to the endometrium at the end of the menstrual phase?
What significant change occurs to the endometrium at the end of the menstrual phase?
Signup and view all the answers
What role does estrogen play regarding the epithelial cells of the vagina?
What role does estrogen play regarding the epithelial cells of the vagina?
Signup and view all the answers
Study Notes
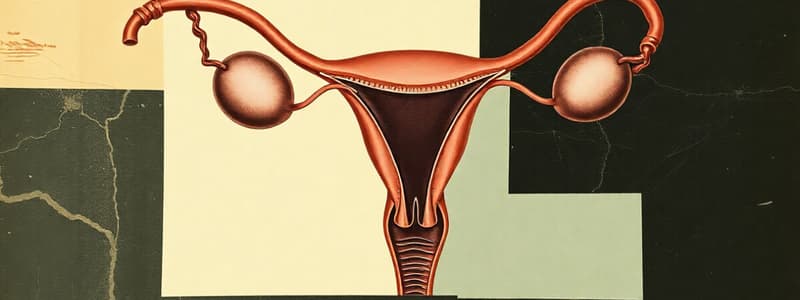
Female Genital Tract
- The female reproductive system consists of paired ovaries, oviducts (uterine tubes), uterus, vagina, and external genitalia, and mammary glands.
- The ovaries produce female gametes (oocytes) and steroidal sex hormones.
- They provide a fertilization environment and support the embryo/fetus.
Ovaries
- Almond-shaped with multiple layers.
- The surface epithelium is a simple cuboidal epithelium, continuous with the mesothelium (outermost layer).
- A layer of dense connective tissue, the tunica albuginea, surrounds the surface.
- The cortex contains highly cellular connective tissue and ovarian follicles of varying sizes.
- Most ovarian follicles degenerate through a process called atresia.
Early Development of the Ovary
- Primordial germ cells migrate from the yolk sac to the gonadal primordia during the first month of embryonic life.
- These cells become oogonia, the precursor to eggs, undergoing mitosis.
- Majority undergo atresia by the time of puberty.
Ovarian Follicles
- Consist of an oocyte surrounded by epithelial cells within a basal lamina.
- Primordial follicles consist of one primary oocyte and a single layer of flattened follicular cells.
- Cells mature into primary, secondary, and Graafian follicles.
Follicular Growth and Development
- Follicle growth starts at puberty with FSH release from the anterior pituitary.
- This involves growth of the oocyte, increasing proliferation/differentiation of follicular cells, and stromal fibroblast proliferation in the surrounding connective tissue.
- Selection of a dominant follicle which will be ovulated is influenced by balanced hormones.
- Follicle-stimulating hormone (FSH) promotes oocyte growth, reaches about 120 um.
Follicular Cells
- Develop into a stratified epithelium.
- Granulosa cells communicate via gap junctions.
- They surround the oocyte, forming the zona pellucida where sperm receptors are located.
- Theca interna and externa layers surround the follicle.
Ovulation
- The release of an oocyte from the ovary.
- Primarily occurs mid-cycle (around day 14 of a 28-day cycle) stimulated by a surge of luteinizing hormone (LH).
- The dominant follicle ruptures, releasing the secondary oocyte and corona radiata.
Corpus Luteum
- Formed from the remains of the follicle after ovulation.
- Secretes progesterone and estrogen.
- If no pregnancy occurs, it degenerates into the corpus albicans.
- If pregnancy does occur, it persists and maintains pregnancy.
Uterine Tubes (Fallopian Tubes)
- Paired tubes connecting the ovaries to the uterus with a folded mucosa and muscular layers.
- Functionally distinct cell (ciliated and secretory ) types.
- Assists in moving the ovum towards the uterus.
Uterus
- Pear-shaped muscular organ.
- Divided into fundus (upper part), body, and cervix (lower part).
- Uterine wall composed of perimetrium (outermost layer), myometrium (muscular middle layer), and endometrium (inner lining).
- The endometrium undergoes cyclical changes during the menstrual cycle.
Menstrual Cycle
- Cyclical changes in the endometrium.
- Four phases: menstrual, proliferative, secretory, and ischemic.
- Driven primarily by estrogen and progesterone levels from the ovary.
Cervix
- Cylindrical part of the uterus.
- Lined with simple columnar epithelium.
- Contains cervical glands secreting mucus.
- Plays a role in regulating sperm transport.
Vagina
- Muscular tube connecting the cervix to the external environment.
- Lined with stratified squamous epithelium.
- Plays a pivotal role in the reproductive process including sexual intercourse, delivery of newborn, and as a protective barrier for the female reproductive system.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the anatomy and early development of the female genital tract, focusing on the ovaries. This quiz covers the structure, function, and cellular composition of the ovaries, including the process of atresia of ovarian follicles. Gain insights into the reproductive system and early embryonic development.