Podcast
Questions and Answers
What is the primary role of the frontonasal process in facial development?
What is the primary role of the frontonasal process in facial development?
What structure is formed by the fusion of the maxillary and mandibular swellings?
What structure is formed by the fusion of the maxillary and mandibular swellings?
During which weeks do the palatine shelves fuse with the primary palate?
During which weeks do the palatine shelves fuse with the primary palate?
Which of the following theories suggests that cartilage is the primary determinant for growth in facial structures?
Which of the following theories suggests that cartilage is the primary determinant for growth in facial structures?
Signup and view all the answers
What is the origin of intramembranous ossification?
What is the origin of intramembranous ossification?
Signup and view all the answers
What is a significant consequence of the failure of maxillary swellings to fuse?
What is a significant consequence of the failure of maxillary swellings to fuse?
Signup and view all the answers
What distinguishes the growth response of condylar cartilage from other body cartilage?
What distinguishes the growth response of condylar cartilage from other body cartilage?
Signup and view all the answers
What does the functional matrix theory emphasize regarding craniofacial growth?
What does the functional matrix theory emphasize regarding craniofacial growth?
Signup and view all the answers
Which developmental process initiates the formation of the intermaxillary process?
Which developmental process initiates the formation of the intermaxillary process?
Signup and view all the answers
How does genetic control influence craniofacial growth?
How does genetic control influence craniofacial growth?
Signup and view all the answers
What is the primary role of the periosteal matrix in craniofacial growth?
What is the primary role of the periosteal matrix in craniofacial growth?
Signup and view all the answers
Which of the following statements is true regarding postnatal craniofacial growth?
Which of the following statements is true regarding postnatal craniofacial growth?
Signup and view all the answers
What factor is indicated as having a poor correlation with jaw growth?
What factor is indicated as having a poor correlation with jaw growth?
Signup and view all the answers
What influences the individual differences in phenotype during craniofacial development?
What influences the individual differences in phenotype during craniofacial development?
Signup and view all the answers
How does mandibular growth change after puberty?
How does mandibular growth change after puberty?
Signup and view all the answers
Which matrix is responsible for structures associated with organs?
Which matrix is responsible for structures associated with organs?
Signup and view all the answers
What is the primary mechanism that determines craniofacial structure from a genetic perspective?
What is the primary mechanism that determines craniofacial structure from a genetic perspective?
Signup and view all the answers
During the growth of the maxilla, what role does the dental eruption of teeth play?
During the growth of the maxilla, what role does the dental eruption of teeth play?
Signup and view all the answers
What is indicated as a significant period of growth for the maxillary complex?
What is indicated as a significant period of growth for the maxillary complex?
Signup and view all the answers
What factors primarily influence craniofacial growth in males and females?
What factors primarily influence craniofacial growth in males and females?
Signup and view all the answers
What are the two types of matrices involved in craniofacial growth?
What are the two types of matrices involved in craniofacial growth?
Signup and view all the answers
At what age does the maxillary complex growth significantly slow down?
At what age does the maxillary complex growth significantly slow down?
Signup and view all the answers
What happens to the maxillary swellings as they grow during facial development?
What happens to the maxillary swellings as they grow during facial development?
Signup and view all the answers
Which mechanism primarily influences changes in the width of the posterior mandible?
Which mechanism primarily influences changes in the width of the posterior mandible?
Signup and view all the answers
At which week do the palatine shelves begin to rotate upwards towards the midline?
At which week do the palatine shelves begin to rotate upwards towards the midline?
Signup and view all the answers
Which growth pattern does the maxilla follow until the age of 12?
Which growth pattern does the maxilla follow until the age of 12?
Signup and view all the answers
Which ossification process involves the formation of bone in a membrane?
Which ossification process involves the formation of bone in a membrane?
Signup and view all the answers
Which theory posits that sutures have an innate growth potential?
Which theory posits that sutures have an innate growth potential?
Signup and view all the answers
What is a significant factor in predicting craniofacial growth patterns?
What is a significant factor in predicting craniofacial growth patterns?
Signup and view all the answers
Which factor contributes to the individual differences in craniofacial phenotypes?
Which factor contributes to the individual differences in craniofacial phenotypes?
Signup and view all the answers
What composition is formed by the intermaxillary process during facial development?
What composition is formed by the intermaxillary process during facial development?
Signup and view all the answers
How does the mandibular body change by puberty?
How does the mandibular body change by puberty?
Signup and view all the answers
What is indicated as a response when bone separates at the sutures?
What is indicated as a response when bone separates at the sutures?
Signup and view all the answers
Which component is crucial for the downward growth of the maxilla during development?
Which component is crucial for the downward growth of the maxilla during development?
Signup and view all the answers
Which statement is true about cartilaginous growth according to the cartilaginous theory?
Which statement is true about cartilaginous growth according to the cartilaginous theory?
Signup and view all the answers
What primarily contributes to the genetic control of craniofacial growth?
What primarily contributes to the genetic control of craniofacial growth?
Signup and view all the answers
Study Notes
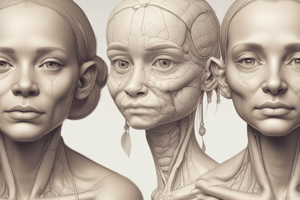
Facial Growth Development
- Facial growth starts at week 4 with the formation of 5 swellings around the primitive mouth (stomodeum)
- The maxillary and mandibular swellings develop from the first pharyngeal arch, located laterally to the stomodeum
- The mandibular swellings form the lower border and the fifth swelling
- The frontonasal process forms the upper border of the stomodeum
- The maxillary swellings form the upper border of the stomodeum
- The maxillary swellings grow forward and move closer together, fusing at the midline
- The nasal placode forms as two thickenings on the frontonasal process
- Failure of the maxillary swelling fusion leads to unilateral or bilateral cleft lip
- The fusion of maxillary and mandibular swellings forms the cheeks, reducing the width of the mouth
Palate Formation
- The intermaxillary process forms the primary palate, premaxilla, front of the anterior palate, and the four maxillary incisors
- During week 7, thin extensions in the inner wall of the maxillary process form the palatine shelves, initially located on either side of the lateral tongue
- The palatine shelves rotate upwards to the midline as the tongue lowers
- During weeks 8 and 9, the shelves fuse with each other, the primary palate, and the lower border of the nasal septum
Bone Growth and Formation
- Bone formation occurs through intramembranous ossification (bone formation in membrane) and endochondral ossification (bone replacing cartilage)
- Intramembranous ossification occurs in sheets during embryonic development
- Intramembranous ossification is responsible for the formation of the calvarium, facial bones, most of the mandible, and the clavicle
- Bones of the face and skull are joined by sutures
- Bony infill at sutures is a response to the force separating the bones on either side
- Growth causes the mass of bone to move relative to its neighbors (displacement)
- Remodeling and displacement can occur simultaneously on the same bone
- Cartilage in the mandibular condyle is different from the rest of the body
- The condylar cartilage grows in response to other facial structures
Craniofacial Growth Control
- Genetic control has a greater influence on anteroposterior growth compared to vertical growth ### Craniofacial Growth Theories
- Sutural theory (Sicher): Sutures are believed to have innate growth potential, pushing bones apart. This theory has been disproven.
- Cartilaginous theory (Scott): Cartilage is considered the primary determinant of growth. This theory is supported by the fact that transplanted nasal septum cartilage into other tissues shows some growth.
- Functional matrix theory (Moss): Genetic control is expressed in soft tissues, determining the size and shape of bone. Two types of matrices are involved: periosteal (teeth, muscles, blood vessels, nerves) and capsular (organs).
- It's likely that both capsular and functional matrix theories play a role in craniofacial growth. ### Postnatal Craniofacial Growth
- As the face enlarges, it grows forward and downwards.
- The calvarium, cranial base, maxilla, and mandible grow differently, completing growth by 7 years old.
- Facial growth slows down during puberty.
- The maxilla's growth pattern is closer to neural growth, declining at 12 years old.
- Maxillary complex growth is important for positioning upper teeth.
- The maxilla grows downwards and forwards until 7 years old through drift and remodeling.
- Downward growth leads to the drift of hard palate and vertical development of the alveolar process as teeth erupt and roots form
- Lateral growth involves the displacement of the halves of the maxilla and infill at the mid-palatal suture
- The maxillary complex slows at 7 years old and stops at 12 years old
- The mandible follows somatic growth through periosteal activity.
- The alveolar process adds to the vertical height.
- The mandible is displaced forward by the tongue's growth.
- Remodeling leads to increased width of the posterior mandible, length, and a prominent chin
- 2-3mm growth occurs in the mandibular body, which doubles at puberty.
- Mandibular growth slows down at 17 years old for girls and 19 years old for boys
- Facial growth never completely stops.
Growth Prediction
- Bone maturation on hand-wrist radiographs has weak correlation with jaw growth. Cervical vertebrae offer better assessments.
- These assessments reveal different skeletal types and their corresponding general facial patterns.
Epigenetics and Facial Growth
- Epigenetics studies how cells control gene activity without changing the gene sequence.
- It explains stable, heritable traits not caused by changes in DNA.
- Epigenetics leads to individual differences in appearance, physiology, cognition, and behavior, known as the phenotype.
- Genes responsible for craniofacial structures are essentially the same, but every face is unique.
- Mechanisms like histone modification play a part in this process.
- Neural crest cells are responsible for facial structures.
- Environmental signals reach the neural crest cell to activate the chromatin state.
Sexual Dimorphism in Facial Growth
- Males and females have differences in facial features.
- These differences are further influenced by epigenetics and environmental factors.
Facial Development
- Begins at week 4 with five swellings around the stomodeum (primitive mouth)
- Maxillary and mandibular swellings form from the first pharyngeal arch, located laterally on either side of the stomodeum
- Mandibular swellings form the lower border and the fifth arch
- Frontonasal process forms the upper border of the stomodeum
- Maxillary swellings form the upper border of the stomodeum
- Maxillary swellings grow forward and move closer together to fuse at the midline
- Nasal placode develops as two thickenings on the frontonasal process
- Failure of maxillary swelling fusion results in a unilateral or bilateral cleft lip
- Fusion of maxillary and mandibular swellings forms the cheeks, reducing the width of the mouth
Palate Formation
- Intermaxillary process forms the primary palate, premaxilla, the front of the anterior palate (four maxillary incisors), and the nasal septum
- At week 7, thin extensions form in the inner wall of the maxillary process, known as palatine shelves
- Palatine shelves form initially on either side of the lateral tongue
- Palatine shelves rotate upwards to the midline as the tongue lowers
- At weeks 8 and 9, shelves fuse to each other, the primary palate, and the lower border of the nasal septum
Bone Formation and Growth
- Intramembranous ossification forms bone in membrane
- Endochondral ossification replaces cartilage with bone
- Bone can form using both methods
- Intramembranous formation occurs during embryonic development within sheets
- Bones of the skull and face are joined by sutures
- Bony infill at sutures is a response to the force separating bones on either side
- Growth causes a mass of bone to move relative to its neighbors, which is called displacement
- Remodelling and displacement can occur simultaneously on the same bone
- Cartilage in the mandibular condyle differs from the rest of the body
- Condylar cartilage grows in response to other facial structures
Control of Craniofacial Growth
- Genetic control is greater for anteroposterior growth compared to vertical growth
- Sutural theory (Sicher):
- Sutures have innate growth potential
- Sutures push bones apart
- This has been proven untrue as transplanted sutures had no effect
- Stretched sutures result in growth
- Sutures respond with passive deposition
- Cartilaginous theory (Scott):
- Primary determinant for growth is cartilage
- Transplanted nasal septum cartilage to other tissues resulted in some growth
- 75% experienced no impairment in growth after condylar fracture in growing children
- Functional matrix theory (Moss) — capsular + periosteal matrices:
- Genetic control is expressed in soft tissues, which determines the size and shape of bone
- Two types of matrices: periosteal and capsular
- Periosteal: teeth, muscles, blood vessels, and nerves
- Microskeletal unit has its own periosteal matrix
- Capsular matrix: organs
- Congenital absence of the eye leads to a diminutive and rudimentary orbit
- It is likely that both capsular and functional matrix theories play a part in craniofacial growth
Postnatal Craniofacial Growth
- As the face enlarges, it grows forward and downwards
- The calvarium, cranial base, maxilla, and mandible grow differently and finish developing by age 7
- Facial growth slows during puberty
- Maxillary growth pattern more closely resembles neural growth, declining at age 12
- The maxillary complex is important for the position of the upper teeth
- The maxilla grows downward and forward until age 7 by drift and remodelling
- Downward growth: drift of hard palate and vertical development of the alveolar process as teeth erupt and roots form
- Lateral growth: displacement of the halves of the maxilla and infill at the mid-palatal suture
- Maxillary complex slows at age 7 and stops at age 12
- The mandible follows somatic growth due to periosteal activity
- The alveolar process adds to vertical height
- The mandible is displaced forward by tongue growth
- Remodelling increases the width of the posterior mandible, length, and prominence of the chin
- Growth occurs 2-3mm in the mandibular body and doubles at puberty
- Growth slows down at age 17 for girls and at age 19 for boys
- Facial growth never completely stops
Growth Prediction
- Bone maturation on hand-wrist radiographs poorly correlates with jaw growth
- A better method for assessing jaw growth involves using cervical vertebrae
- This allows for the identification of different skeletal types and their corresponding general facial patterns
Epigenetics and Facial Growth
- The study of how cells control gene activity without changing the gene sequence
- Stable, heritable traits not explained by changes in DNA
- Leads to individual differences in appearance, physiology, cognition, and behavior (phenotype)
- Genes responsible for craniofacial structures are essentially the same, but every face is unique
- Mechanisms include histone modification
- Neural crest cells are the origin of facial structures
- Environmental signals reach neural crest cells to activate chromatin state
Facial Differences Between Men and Women
-
Males
- Increased prominence of brow ridges
- More pronounced jawline, prominent chin
- Larger cranium
- More squared facial features
- Greater facial width
-
Females
- Smoother brow ridges
- Rounder jaw, less defined chin
- Smaller cranium
- More rounded facial features
- Greater facial height
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the critical stages of facial growth and palate formation during embryonic development. It explores the formation of various structures such as the maxillary and mandibular swellings, and the consequences of their fusion. Understanding these processes is essential for grasping the complexities of human facial anatomy.