Podcast
Questions and Answers
What anatomical landmark is used to identify the cardio-esophageal junction during an endoscopy?
What anatomical landmark is used to identify the cardio-esophageal junction during an endoscopy?
- The location of the cricopharyngeal sphincter.
- The point where the esophagus passes below the diaphragm.
- The Z-line, representing the change from esophageal to gastric mucosa. (correct)
- The point where the esophagus enters the posterior mediastinum.
At which anatomical location does the esophagus's circular muscles transition into the oblique muscles of the stomach?
At which anatomical location does the esophagus's circular muscles transition into the oblique muscles of the stomach?
- The thoracic vertebra number 11.
- The cricopharyngeal sphincter.
- The Collar of Helvetius. (correct)
- The diaphragmatic hiatus.
A patient undergoing endoscopy experiences a perforation. Which physiological constriction of the esophagus is most likely the location of this injury?
A patient undergoing endoscopy experiences a perforation. Which physiological constriction of the esophagus is most likely the location of this injury?
- Aortic & bronchial constriction. (correct)
- Cardio-esophageal junction.
- Diaphragmatic sphincter.
- Cricopharyngeal constriction.
A surgeon is planning an extensive mobilization of the esophagus. What anatomical feature allows for this procedure to be performed safely without compromising the viability of the esophagus?
A surgeon is planning an extensive mobilization of the esophagus. What anatomical feature allows for this procedure to be performed safely without compromising the viability of the esophagus?
During a surgical resection for esophageal cancer, involvement of which lymph nodes would indicate inoperability?
During a surgical resection for esophageal cancer, involvement of which lymph nodes would indicate inoperability?
Which of the following statements is correct regarding the nerve supply of the esophagus?
Which of the following statements is correct regarding the nerve supply of the esophagus?
Why is a leak more likely after an oesophageal anastomosis, and cancerous cells spread more easily?
Why is a leak more likely after an oesophageal anastomosis, and cancerous cells spread more easily?
Which of the following is the most common type of benign esophageal tumor?
Which of the following is the most common type of benign esophageal tumor?
A patient presents with dysphagia and is suspected of having a benign esophageal tumor. After initial investigations, a CT scan is performed. What is the primary role of the CT scan in this scenario?
A patient presents with dysphagia and is suspected of having a benign esophageal tumor. After initial investigations, a CT scan is performed. What is the primary role of the CT scan in this scenario?
A patient is diagnosed with a small leiomyoma in the esophagus. What is the preferred treatment approach?
A patient is diagnosed with a small leiomyoma in the esophagus. What is the preferred treatment approach?
Which of the following is the most common histological type of esophageal cancer worldwide?
Which of the following is the most common histological type of esophageal cancer worldwide?
Which of the following is the most significant risk factor associated with esophageal adenocarcinoma in Western countries?
Which of the following is the most significant risk factor associated with esophageal adenocarcinoma in Western countries?
A patient with a history of lye ingestion several years ago is now at increased risk for which type of esophageal cancer?
A patient with a history of lye ingestion several years ago is now at increased risk for which type of esophageal cancer?
Which of the following histopathological types of esophageal carcinoma has the best prognosis?
Which of the following histopathological types of esophageal carcinoma has the best prognosis?
What is the primary mechanism by which esophageal cancer leads to a narrowed esophageal lumen?
What is the primary mechanism by which esophageal cancer leads to a narrowed esophageal lumen?
A patient with known esophageal cancer presents with palpable left supraclavicular nodes. What does this clinical finding indicate?
A patient with known esophageal cancer presents with palpable left supraclavicular nodes. What does this clinical finding indicate?
Which of the following is a typical symptom of esophageal cancer?
Which of the following is a typical symptom of esophageal cancer?
A clinician suspects that a patient has esophageal cancer. Which diagnostic test is most crucial for confirming the diagnosis?
A clinician suspects that a patient has esophageal cancer. Which diagnostic test is most crucial for confirming the diagnosis?
What is the primary purpose of using Positron Emission Tomography (PET) in the context of esophageal cancer?
What is the primary purpose of using Positron Emission Tomography (PET) in the context of esophageal cancer?
What is the key advantage of using endoscopic ultrasound (EUS) over CT scans for esophageal cancer staging?
What is the key advantage of using endoscopic ultrasound (EUS) over CT scans for esophageal cancer staging?
According to the staging information, which characteristic would make surgical cure for esophageal cancer unlikely?
According to the staging information, which characteristic would make surgical cure for esophageal cancer unlikely?
According to the TNM staging system, what does a T3 designation indicate for esophageal cancer?
According to the TNM staging system, what does a T3 designation indicate for esophageal cancer?
Which of the following is considered a palliative treatment option for advanced esophageal cancer?
Which of the following is considered a palliative treatment option for advanced esophageal cancer?
What is a key advantage of Metallic self-expandable stents in the palliative management of esophageal cancer?
What is a key advantage of Metallic self-expandable stents in the palliative management of esophageal cancer?
What is the primary goal of surgery in the management of esophageal cancer?
What is the primary goal of surgery in the management of esophageal cancer?
In performing an esophagectomy, what anatomical structure is typically used as a conduit to replace the resected esophagus?
In performing an esophagectomy, what anatomical structure is typically used as a conduit to replace the resected esophagus?
What is a notable advantage of the transhiatal approach (Orringer approach) for esophagectomy?
What is a notable advantage of the transhiatal approach (Orringer approach) for esophagectomy?
A patient is deemed unsuitable for surgery due to comorbidities but requires treatment for esophageal cancer. What is a useful alternative to surgery?
A patient is deemed unsuitable for surgery due to comorbidities but requires treatment for esophageal cancer. What is a useful alternative to surgery?
Which of the following factors contributes to the poor prognosis associated with esophageal cancer?
Which of the following factors contributes to the poor prognosis associated with esophageal cancer?
Considering the arterial supply of the esophagus, a compromise to which artery would least likely affect the overall viability of the esophagus due to the rich anastomotic network?
Considering the arterial supply of the esophagus, a compromise to which artery would least likely affect the overall viability of the esophagus due to the rich anastomotic network?
What is the key implication of the absence of a serosa in the esophageal wall regarding cancer progression and surgical management?
What is the key implication of the absence of a serosa in the esophageal wall regarding cancer progression and surgical management?
Which plexus, critical for esophageal function, is notably absent in the upper third of the esophagus, potentially influencing the presentation and management of motility disorders?
Which plexus, critical for esophageal function, is notably absent in the upper third of the esophagus, potentially influencing the presentation and management of motility disorders?
Given the lymphatic drainage patterns of the esophagus, involvement of which lymph node group would most significantly alter the surgical approach to esophageal cancer, potentially rendering it inoperable?
Given the lymphatic drainage patterns of the esophagus, involvement of which lymph node group would most significantly alter the surgical approach to esophageal cancer, potentially rendering it inoperable?
A patient presents with dysphagia and a history of known esophageal carcinoma. The barium swallow reveals an abrupt change in the esophageal 'axis'. What is the most accurate interpretation of this finding?
A patient presents with dysphagia and a history of known esophageal carcinoma. The barium swallow reveals an abrupt change in the esophageal 'axis'. What is the most accurate interpretation of this finding?
Considering the location of esophageal tumors, which third of the esophagus is most commonly affected by squamous cell carcinomas arising from lye strictures?
Considering the location of esophageal tumors, which third of the esophagus is most commonly affected by squamous cell carcinomas arising from lye strictures?
In the context of esophageal cancer, what is the clinical significance of Troisier's sign?
In the context of esophageal cancer, what is the clinical significance of Troisier's sign?
What is the most critical implication of persistent dysphagia in the context of esophageal cancer?
What is the most critical implication of persistent dysphagia in the context of esophageal cancer?
Which of the following histopathological subtypes of esophageal carcinoma has the most favorable outcome, even though it is considered rare?
Which of the following histopathological subtypes of esophageal carcinoma has the most favorable outcome, even though it is considered rare?
Considering the various diagnostic modalities for esophageal cancer, in which scenario would endoscopic ultrasound (EUS) provide the most critical advantage over computed tomography (CT) in determining the therapeutic approach?
Considering the various diagnostic modalities for esophageal cancer, in which scenario would endoscopic ultrasound (EUS) provide the most critical advantage over computed tomography (CT) in determining the therapeutic approach?
According to the TNM staging system, which of the following scenarios would classify as T4 disease in esophageal cancer?
According to the TNM staging system, which of the following scenarios would classify as T4 disease in esophageal cancer?
In the context of esophageal cancer staging and prognosis, which of the following factors is most indicative of an unlikely surgical cure, even in the absence of distant metastasis?
In the context of esophageal cancer staging and prognosis, which of the following factors is most indicative of an unlikely surgical cure, even in the absence of distant metastasis?
When considering palliative treatment options for advanced esophageal cancer, what is the primary advantage of metallic self-expandable stents over other methods?
When considering palliative treatment options for advanced esophageal cancer, what is the primary advantage of metallic self-expandable stents over other methods?
In the management of esophageal cancer, what is the rationale for performing an esophagectomy with regional lymphadenectomy?
In the management of esophageal cancer, what is the rationale for performing an esophagectomy with regional lymphadenectomy?
What is the main advantage of the transhiatal approach (Orringer approach) for esophagectomy compared to transthoracic approaches?
What is the main advantage of the transhiatal approach (Orringer approach) for esophagectomy compared to transthoracic approaches?
After an esophagectomy, what is the most life-threatening complication linked to the absence of a serosal layer on the anastomosis?
After an esophagectomy, what is the most life-threatening complication linked to the absence of a serosal layer on the anastomosis?
What is the rationale behind performing a feeding jejunostomy as part of an esophagectomy?
What is the rationale behind performing a feeding jejunostomy as part of an esophagectomy?
What is the primary reason oesophageal cancers carry a poor prognosis?
What is the primary reason oesophageal cancers carry a poor prognosis?
Why is it crucial to identify the esophagogastric junction? (Select all that apply)
Why is it crucial to identify the esophagogastric junction? (Select all that apply)
What would be the best options to palliate a patient with advanced esophageal cancer? (Select all that apply)
What would be the best options to palliate a patient with advanced esophageal cancer? (Select all that apply)
What are the most significant identifiable risk factors for esophageal cancer?
What are the most significant identifiable risk factors for esophageal cancer?
In assessing a patient with esophageal cancer, if the endoscopic ultrasound (EUS) identifies more than 5 malignant lymph nodes upon evaluation, which of the following statements is most accurate about considering curative resection?
In assessing a patient with esophageal cancer, if the endoscopic ultrasound (EUS) identifies more than 5 malignant lymph nodes upon evaluation, which of the following statements is most accurate about considering curative resection?
Clinically significant motility disorders affect lower 2/3 (smooth muscle) of esophagus. What is the significance of this information?
Clinically significant motility disorders affect lower 2/3 (smooth muscle) of esophagus. What is the significance of this information?
In the surgical approach to esophageal cancer, preservation of the feeding artery and vein is paramount. What is the most probable reason?
In the surgical approach to esophageal cancer, preservation of the feeding artery and vein is paramount. What is the most probable reason?
While some squamous cell carcinomas are radiosensitive, what can further improve the 5-year survival rate?
While some squamous cell carcinomas are radiosensitive, what can further improve the 5-year survival rate?
Factors responsible for early spread and aggressive behavior of carcinoma oesophagus involves (select all the apply):
Factors responsible for early spread and aggressive behavior of carcinoma oesophagus involves (select all the apply):
The majority of esophageal cancers are found to be in what stage?
The majority of esophageal cancers are found to be in what stage?
If 'endosono' detects which of the following will it be a case for curative resection?
If 'endosono' detects which of the following will it be a case for curative resection?
If you have the opportunity to have surgery on early detection, do you have limited benefits?
If you have the opportunity to have surgery on early detection, do you have limited benefits?
Flashcards
Esophagus Length & Course
Esophagus Length & Course
Extends 25 cm, from the cricopharyngeal sphincter to cardio-esophageal junction, runs in the posterior mediastinum, with 2 cm below the diaphragm.
Collar of Helvetius
Collar of Helvetius
Site where the esophagus's circular muscles transition to oblique stomach muscles.
Cricopharyngeal Constriction
Cricopharyngeal Constriction
Cricopharyngeal constriction at 15 cm has a diameter of 14 mm, possibly causing foreign body lodgement.
Cervical Esophagus Arterial Supply
Cervical Esophagus Arterial Supply
Signup and view all the flashcards
Thoracic Esophagus Venous Drainage
Thoracic Esophagus Venous Drainage
Signup and view all the flashcards
Upper Esophagus Lymphatic Drainage
Upper Esophagus Lymphatic Drainage
Signup and view all the flashcards
Involvement of Coeliac Nodes
Involvement of Coeliac Nodes
Signup and view all the flashcards
Intrinsic Plexus
Intrinsic Plexus
Signup and view all the flashcards
Esophageal Mucosa Significance
Esophageal Mucosa Significance
Signup and view all the flashcards
Upper Esophageal Sphincter
Upper Esophageal Sphincter
Signup and view all the flashcards
Esophageal Lining
Esophageal Lining
Signup and view all the flashcards
Leiomyoma
Leiomyoma
Signup and view all the flashcards
Carcinoma Location
Carcinoma Location
Signup and view all the flashcards
Esophageal Cancer Types
Esophageal Cancer Types
Signup and view all the flashcards
Etiology of Esophagus Cancer
Etiology of Esophagus Cancer
Signup and view all the flashcards
Precancerous Conditions
Precancerous Conditions
Signup and view all the flashcards
Carcinogens That Increase Esophagus Cancer Risks
Carcinogens That Increase Esophagus Cancer Risks
Signup and view all the flashcards
Hovels-Evans syndrome or tylosis
Hovels-Evans syndrome or tylosis
Signup and view all the flashcards
Risk Factor for Adenocarcinoma
Risk Factor for Adenocarcinoma
Signup and view all the flashcards
Epitheliomatous Ulcer
Epitheliomatous Ulcer
Signup and view all the flashcards
Infiltrative (Annular stenosing)
Infiltrative (Annular stenosing)
Signup and view all the flashcards
Better Outcome
Better Outcome
Signup and view all the flashcards
Malignant Dysphagia
Malignant Dysphagia
Signup and view all the flashcards
Backache
Backache
Signup and view all the flashcards
Abdominal Signs
Abdominal Signs
Signup and view all the flashcards
Barium Swallow Test
Barium Swallow Test
Signup and view all the flashcards
Oeseophagoscopy To Take Biopsies
Oeseophagoscopy To Take Biopsies
Signup and view all the flashcards
Highly Accurate Way to Detect.
Highly Accurate Way to Detect.
Signup and view all the flashcards
Detect tumor through high frequency
Detect tumor through high frequency
Signup and view all the flashcards
Patient to Decide Whether To Receive.
Patient to Decide Whether To Receive.
Signup and view all the flashcards
Anatomical Location
Anatomical Location
Signup and view all the flashcards
Z-line Identification
Z-line Identification
Signup and view all the flashcards
Aortic & Bronchial Constriction
Aortic & Bronchial Constriction
Signup and view all the flashcards
Diaphragmatic Sphincter Constriction
Diaphragmatic Sphincter Constriction
Signup and view all the flashcards
Venous Drainage
Venous Drainage
Signup and view all the flashcards
Esophageal Mucosa
Esophageal Mucosa
Signup and view all the flashcards
SCC Location
SCC Location
Signup and view all the flashcards
Adenocarcinoma Location
Adenocarcinoma Location
Signup and view all the flashcards
Esophageal Cancer Risk Factor
Esophageal Cancer Risk Factor
Signup and view all the flashcards
Squamous Cell Factors
Squamous Cell Factors
Signup and view all the flashcards
Esophageal cancer lesions
Esophageal cancer lesions
Signup and view all the flashcards
Liver affect
Liver affect
Signup and view all the flashcards
Signs the patient cannot heal.
Signs the patient cannot heal.
Signup and view all the flashcards
Multiple Biopsies with Oesophagoscopy
Multiple Biopsies with Oesophagoscopy
Signup and view all the flashcards
Structure involvement with Tumor.
Structure involvement with Tumor.
Signup and view all the flashcards
Management of Cancer
Management of Cancer
Signup and view all the flashcards
Tubes to help Relieve.
Tubes to help Relieve.
Signup and view all the flashcards
More lymphs vessels.
More lymphs vessels.
Signup and view all the flashcards
Study Notes
Esophageal Cancer
- Esophageal cancer is reviewed, with key information about surgical anatomy, vasculature, and nerve supply
Esophagus Anatomy
- The esophagus is about 25 cm long, extending from the cricopharyngeal sphincter to the cardio-esophageal junction.
- The esophagus runs in the posterior mediastinum as a continuation of the pharynx.
- Approximately 2 cm of the esophagus lies below the diaphragm.
- Anatomically, the cardio-esophageal junction lies to the left of the thoracic vertebra number 11.
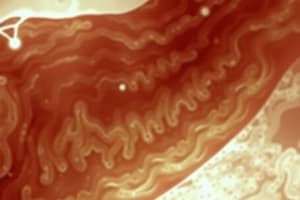
- Endoscopically, the junction is identified by a Z-line, where the esophageal mucosa changes to the gastric mucosa.
- The Collar of Helvetius marks where the esophagus's circular muscles turn into the stomach's oblique muscles at the incisura.
Physiological Constrictions
- The esophagus has 3 constrictions
- The cricopharyngeal constriction is 15 cm from the incisor teeth and has a diameter of 14 mm and can cause foreign body lodgement
- The aortic and bronchial constriction is 25 cm from the incisor teeth and has a diameter of 15-17 mm and this area is prone to perforation during endoscopy
- The diaphragmatic sphincter is 40 cm from the incisor teeth, has a diameter of 16-19 mm and is linked to malignancy
Vasculature and Nerve Supply
- The cervical esophagus is mainly suppliedby branches of the inferior thyroid artery.
- The upper thoracic esophagus is supplied mainly from branches of the inferior thyroid artery, and less consistently from an anterior esophago-tracheal branch from the aorta.
- The mid and lower thoracic esophagus is supplied by bronchial arteries.
- The lower esophagus receives small branches of the left gastric artery.
- Azygos and hemiazygos veins drain the thoracic esophagus.
- Veins accompany arteries
- Rich internal arterial anastomosis is present in the esophagus and the stomach allowing for extensive mobilization of the esophagus without compromising viability.
- Lymphatics:
- The upper esophagus drains into the left and right supraclavicular nodes.
- The middle esophagus drains into the tracheobronchial and paraoesophageal nodes.
- The lower esophagus drains into LNs along the lesser curvature of the stomach and then into coeliac nodes.
- Involvement of coeliac nodes indicates inoperability.
- Parasympathetic supply is from the vagus nerve and includes extrinsic/intrinsic plexuses.
- The intrinsic plexus lacks Meissner's network.
- Auerbach's plexus is only present in the lower two-thirds.
Surgical Anatomy Key Points
- Upper esophageal sphincter: dense cricopharyngeus muscle leads to Zenker's diverticulum through Killian triangle
- Lower esophageal sphincter: high pressure zone at gastro-oesophageal junction. Weakness causes reflux oesophagitis
- Oesophageal mucosa: important in oesophageal anastomosis
- No serosa, no mesentery: mobilization is required and the leak rate is high, so easy spread of carcinoma.
- Helicoidal muscle: helps peristalsis, but it recoils due to elasticity. Post resection, the specimen shortens and anastomosis may become difficult.
- Segmental arterial supply: extensive mobilization can be done without compromising blood supply for transhiatal esophagectomies
- Lower end of oesophagus-veins: rich intercommunicating veins between portal and systemic veins resulting in oesophageal varices occurring
- Azygos vein crossing oesophagus in thorax are prone to injury and bleeding making midoesophageal tumours form
- Mucosal & submucosal lymphatics out number capillaries so Oesophageal tumours extend over a long distance within oesophageal wall, requiring total oesophagectomy, cervical anastomosis, & lymph node clearance.
Histology
- Layers consist of an inner circular layer and outer longitudinal layer.
- Muscle Type:
- Upper 1/3: Striated muscle fibers
- Lower 2/3: Smooth muscle fibers Clinically significant motility disorders affect lower 2/3 (smooth muscle) of esophagus.
- Lining:
- The entire esophagus is lined by squamous epithelium.
- Except last 3 cm which is lined by columnar cells "The columnar cells are similar to gastric mucosa, but oxyntic & peptic cells are absent".
- Mucosa is the toughest coat of esophagus and is transformed into rugal folds.
Oesophageal Tumours
- Benign tumors are rare, occurring in less than 0.5% of cases
- Epithelial: hyperplastic polyps, papilloma, and adenoma.
- Stromal: leiomyoma, granular cell tumor (schwannoma), & lipoma.
- Malignant
- SCC (squamous cell carcinoma) in the upper 2/3
- Adenocarcinoma in the lower 1/3
- Melanoma, Lymphoma, leiomyosarcoma, liposarcoma & special type: GIST
Benign Esophageal Tumors
- Leiomyoma is the most common kind
- Usually arises in the distal third with intact overlying mucosa
- Symptoms: asymptomatic for a long time, until it reaches an enormous size to cause dysphagia
- Diagnosis:
- Barium swallow.
- Endoscopy reveals "smooth submucosal lesion" + biopsy.
- CT chest reveals its exact extent.
- Treatment:
- Small lesions (< 5 cm): Enucleation.
- Larger lesions: Esophagectomy.
Carcinoma of Esophagus: Epidemiology
- Most patients are above 50 years old
- Overall Male:Female is 3:1
- Gender incidence:
- Lesions of cervical region: Females > Males.
- Lesions of Thoracic & abdominal oesophagus: Males > Females.
- Site incidence:
- Lower third of the oesophagus is more common than the upper two thirds
- Worldwide, most esophageal cancers are squamous cell carcinoma.
- In most Western countries, More than 70% are adenocarcinomas.
- Shift is mainly due to smoking, alcohol and Barrett's oesophagus
- Some improvement in diagnosis and treatment
Etiopathogenesis
- The exact etiology is unknown
- Precancerous/predisposing conditions:
- GORD (Gastroesophageal reflux disease)
- Plummer-Vinson syndrome
- Achalasia of cardia
- Familial keratosis palmaris or plantaris (tylosis) which is an autosomal dominant trait and increases esophageal cancer
- Exposure to Carcinogens:
- Tobacco, heavy smoking, and abuse of alcohol increases squamous cell carcinoma and adenocarcinoma by 20-25%
- Human papilloma virus (HPV) infection increases squamous cell carcinoma
- Risk for cervical and oropharyngeal cancers also.
- Dietary carcinogens/squamous cell carcinoma: elevated nitrates, fungi, and baked bread
Factors
- Squamous cell carcinoma:
- Hovels-Evans syndrome or tylosis in 40 to 60% develop cancers and is called familial keratosis plantaris
- Lye strictures up to 30% and forms 40 to 50 years after. Located in the middle third of the esophagus.
- Achalasia, esophageal web, Plummer-Vinson syndrome, short esophagus, peptic esophagitis and patients with celiac disease.
- Adenocarcinoma
- Barrett's esophagus, obesity (7-fold greater risk), reflux esophagitis, low socioeconomic status, and helicobacter pylori infection: inversely associated with the risk of adenocarcinoma
Sites
- 17% of cases occurs in the the upper 1/3 of oesophagus
- 50% of cases occurs in the the middle 1/3 of oesophagus
- 33% of cases occurs in the the lower 1/3 of oesophagus
Histopathological features of esophageal carcinoma
- Squamous cell carcinoma:
- Epitheliomatous ulcer (carcinomatous): raised edges and flat base
- Proliferative growth (Cauliflower): surface ulcer and commonly bleeds
- Infiltrative (Annular stenosing) variety: early dysphagia (circumferential and longitudinal spread)
- Polypoidal lesion: 5 year survival 70%
- Adenocarcinoma: lower end & middle esophagus (Barrett's esophagus)
- Sarcoma (leiomyosarcoma)
- Carcinosarcoma (best prognosis)
- Primary malignant melanoma and lymphoma
- Carcinoid
Macroscopic Features
- Visible lesions are advanced macroscopically/radiologically
- May be Fungating, Ulcerative, or infiltrative
Spread
- Starts as mucosal ulceration that spreads to the submucosa
- Advances, causing fibrosis and narrowing the lumen
- Then spreads to structures nearby
- Local Spreads
- Tracheo-esophageal fistula: develops from carcinoma in the upper 3rd esophagus when trachea is involved.
- Broncho-esophageal fistula: develops from carcinoma in the middle 3rd esophagus when bronchus is involved.
- Esophago-aortic fistula: results in massive bleeding and is a cause of death and contraindications for surgery/radiotherapy.
- Lymphatic spread: better outcome if metastasis to 5 or fewer lymph nodes
- Blood spread:
- Secondaries in the liver that appear nodular
- Ascites and rectovesical deposits occur later
- Lung metastasis
- Palpable left supraclavicular nodes indicates advanced disease and this sign is called Troisier's sign.
Aggressive Behaviour Factors
- Lack of serosal layer
- Proximity of vital structures
- Extensive mediastinal lymphatic drainage
- Late presentation
Complications
- Neurological complications
- Recurrent laryngeal nerve paralysis
- Phrenic nerve paralysis → Hiccough & diaphragmatic paralysis
- Respiratory complications
- Pneumonia, Mediastinitis, Empyema, and Purulent pericarditis
- Erosion of the aorta (rare) → massive bleeding
Features of Unresected Cancer
- Death
- Obstruction, malnutrition, dehydration, anemia, cachexia
Diagnosis
- Age & sex is men > 60 years
- Progressive development takes place over 18 months
- Affects solids
- 60% of the circumference of the lumen must be involved for growth
- Dysphagia is a late symptom
- Dysphagia
- Short duration
- Solid food but progressively worsens
- Progressive
- Other symptoms
- Regurgitation & loss of appetite, weight loss/cachexia
- Haematemesis is rare
- Melaena is rare
- Pain
- Backache indicates enlarged (coeliac) lymph nodes.
- Other system affection
- Aspiration Pneumonitis & fetor hepaticus
- Hoarseness, and cervical lymph nodes enlargement
Investigations
- CBC: Hb% is low due to generalized weakness.
- Liver function test (LFT) shows if secondary liver problems occurs (increased ALP).
- Take tumor markers
Radiological Testing
- Done to rule out:
- Liver and peritoneal secondaries.
- Lymph nodes in the porta hepatis, coeliac nodes, etc
- Uses fungating or ulcerating irregular persistent intrinsic filling defects and identifies if they deviate
- Barium swallow demonstrates
- Also look for abnormal 'axis', deviation or angulation to demonstrate fistulas
- Detect local infiltration, tumor and liver spread and involvement in the tracheobronchial tree
- Assesses vital structures. and fat
- PET scans are computerized tomography scans that are based on the principle of active tumor cells, is used on lymph nodes, and shows them differentiating, if cancerious or noncancerious and it's response to radio therapy or chemotherap
Oesohagoscopy
- It confirms the diagnosis in more than %90 and confirm cancer
- The addition of brush cytology specimens and seven biopsies
- Is addition of 100% if the lesions thought the addition of lesions thought to seven were the biopsy's
PET Scan Uses
- Finds 'endosono' when more than 5 lymph nodes are not a case for curative resection. Is also a high frequency and good transducer
- Bronchoscopy is used to find if that the tumour is local
Important to Decide in Investigations:
- To resect or not
- Is it worth the resecting
- Can the patient tolerate the procedure
- If the absent of systemic spread
Staging
- Factors deciding the choice of therapy
- General health of patient
- Co-morbid conditions and fitness.
1. General Features In Staging
- Operative risk, spread
- Multiple nodes on CT scan
- Tumor length greater than 20%
TNM Staging
- TO is no evidence of tumor
- Tls is carcinoma and tumor with lamina pro.
- Tis means no primary tumor
- Nx. Lymph cannot be assessed
- No. Lyph
Treatment
- Is main maintenance treatment and ongoing consequence with nutritional status
- Upper and lower tumours are also to be removed to cure
Principle Management:
- Metastatic and locally enavsive disease
- Neoadjuvant followed by esophagectomy. And manage nodes and A and B Lesions
Radiotherapy and Surgery:
- For the primary tumour, the resection that is done has to have 10cm proximally and 5 distal to the tumour.
Standard Esophagectomy:
- Midline laparotomy, followed by distal oesophagus mobilisation and a resection
- Stomach mobilisation
- Thoracotomy
mobilises thoracic oeosphagus and mediastinal nodes,
- Left thoracotomy, the proximal is below
- Right thoracotomy approaches, Ivor Lewis approach where aortic arches are used to reach proximal
Other approaches:
- Additional cervical incisions are preformed so an oesophagogastric anastomosis
- A transhiatal approach which mobilizes by brunt dissection from the hiatus and at the cervical incision
- Minimally invasive robotic surgery
- Oesophageal replacement replaces the stomach via gastric pull up
- Mobilizes both right gastropeploic vessel the segment segments as a connector
- Oesophageal jeyunal flaps separate segments using a microvascular technique
- Then used like radiotherapy and surgery
- Useful at surgeries
- Mainly for the cells that are squamous c and other cancerous cells
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.