Podcast
Questions and Answers
Which molecular event is LEAST likely to be associated with the early pathogenesis of esophageal adenocarcinoma?
Which molecular event is LEAST likely to be associated with the early pathogenesis of esophageal adenocarcinoma?
- Amplification of SOX2 (correct)
- Epigenetic silencing of CDKN2A via hypermethylation
- Loss of function of TP53
- Allelic loss of CDKN2A
A patient with a long history of gastroesophageal reflux disease (GERD) undergoes an endoscopy, and biopsies reveal intestinal metaplasia without dysplasia. While counseling the patient, which factor would LEAST influence the estimated risk of progression to adenocarcinoma?
A patient with a long history of gastroesophageal reflux disease (GERD) undergoes an endoscopy, and biopsies reveal intestinal metaplasia without dysplasia. While counseling the patient, which factor would LEAST influence the estimated risk of progression to adenocarcinoma?
- Patient's age
- Duration of GERD symptoms
- Length of Barrett's mucosa
- Presence of Helicobacter pylori infection (correct)
Which of the following scenarios would MOST strongly suggest a diagnosis of invasive adenocarcinoma over high-grade dysplasia in a biopsy of Barrett's esophagus?
Which of the following scenarios would MOST strongly suggest a diagnosis of invasive adenocarcinoma over high-grade dysplasia in a biopsy of Barrett's esophagus?
- Dysplastic glands exhibiting cytologic atypia and loss of polarity.
- The presence of goblet cells with mucin above the nucleus.
- Angulated glands invading the surrounding tissue with a desmoplastic reaction. (correct)
- Large, dark nuclei with variation in cell size and shape within the glandular epithelium.
A researcher is investigating the relationship between dietary factors and esophageal cancer risk. Which of the following findings would provide the STRONGEST evidence for a protective effect against esophageal adenocarcinoma?
A researcher is investigating the relationship between dietary factors and esophageal cancer risk. Which of the following findings would provide the STRONGEST evidence for a protective effect against esophageal adenocarcinoma?
In comparing the molecular pathogenesis of esophageal adenocarcinoma and squamous cell carcinoma, which of the following statements is MOST accurate?
In comparing the molecular pathogenesis of esophageal adenocarcinoma and squamous cell carcinoma, which of the following statements is MOST accurate?
A pathologist examines a biopsy from an esophageal tumor. Which histological finding would MOST strongly favor a diagnosis of squamous cell carcinoma over adenocarcinoma?
A pathologist examines a biopsy from an esophageal tumor. Which histological finding would MOST strongly favor a diagnosis of squamous cell carcinoma over adenocarcinoma?
A patient is diagnosed with squamous cell carcinoma in the upper third of the esophagus. Based on the typical patterns of metastasis for this cancer, which lymph node group is MOST likely to be involved?
A patient is diagnosed with squamous cell carcinoma in the upper third of the esophagus. Based on the typical patterns of metastasis for this cancer, which lymph node group is MOST likely to be involved?
A patient presents with dysphagia, iron deficiency anemia, and an esophageal web. This clinical presentation is MOST suggestive of which risk factor for squamous cell carcinoma?
A patient presents with dysphagia, iron deficiency anemia, and an esophageal web. This clinical presentation is MOST suggestive of which risk factor for squamous cell carcinoma?
Which of the following best describes the synergistic effect of alcohol and tobacco use on the risk of developing squamous cell carcinoma of the esophagus?
Which of the following best describes the synergistic effect of alcohol and tobacco use on the risk of developing squamous cell carcinoma of the esophagus?
A study reveals that a particular genetic polymorphism is associated with increased expression of CDH1 in esophageal cells. How would this finding MOST likely influence the risk of squamous cell carcinoma development?
A study reveals that a particular genetic polymorphism is associated with increased expression of CDH1 in esophageal cells. How would this finding MOST likely influence the risk of squamous cell carcinoma development?
Flashcards
Barrett Esophagus
Barrett Esophagus
A complication of GERD where stomach acid causes squamous cells in the esophagus to be replaced by intestinal columnar cells.
Dysplasia in Barrett Esophagus
Dysplasia in Barrett Esophagus
Dysplastic glands showing cellular abnormalities, indicating a progression from metaplasia towards cancer.
TP53 and CDKN2A Loss
TP53 and CDKN2A Loss
Loss of function in these genes is commonly seen in early esophageal adenocarcinoma, disrupting cell cycle control and tumor suppression.
Presentation of Esophageal Cancer
Presentation of Esophageal Cancer
Signup and view all the flashcards
Metaplasia
Metaplasia
Signup and view all the flashcards
Invasive Adenocarcinoma
Invasive Adenocarcinoma
Signup and view all the flashcards
Plummer-Vinson Syndrome
Plummer-Vinson Syndrome
Signup and view all the flashcards
Achalasia
Achalasia
Signup and view all the flashcards
SOX2 and Cyclin D1
SOX2 and Cyclin D1
Signup and view all the flashcards
Synergistic Risk Factors
Synergistic Risk Factors
Signup and view all the flashcards
Study Notes
Esophageal Adenocarcinoma and Squamous Cell Carcinoma: Overview
- Esophageal adenocarcinoma and squamous cell carcinoma are compared regarding clinical and pathologic findings, and pathogenesis.
- Esophageal adenocarcinoma and squamous cell carcinoma cases are now about equal, with adenocarcinoma surpassing squamous cell carcinoma in certain regions.
Barrett Esophagus: Precursor to Adenocarcinoma
- Barrett esophagus is a complication of gastroesophageal reflux disease (GERD); stomach acid enters the esophagus.
- About 10% of symptomatic GERD patients have intestinal metaplasia, which is defined as intestinal metaplasia of the esophagus.
- Acid exposure causes squamous cells to be replaced by intestinal columnar cells through transcommitment.
- Metaplasia increases the risk of progression to dysplasia and then to adenocarcinoma.
- 0.2 to 1% of individuals with intestinal metaplasia progress to epithelial dysplasia annually.
- Adenocarcinoma risk is 30-fold higher in patients with Barrett esophagus compared to those without it.
- Increased risk occurs with increased duration of symptoms and patient age.
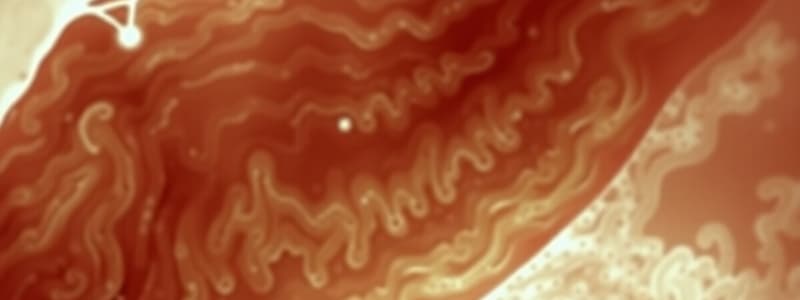
- Endoscopically, Barrett esophagus appears as salmon pink tongues of glandular mucosa extending from the gastroesophageal junction, interspersed with light pink squamous mucosa.
- Microscopically, goblet cells are present (intestinal metaplasia); these cells contain mucin above the nucleus.
Progression to Dysplasia and Adenocarcinoma
- Dysplastic glands with cytologic atypia, variation in cell size/shape, large dark nuclei, and loss of polarity indicate progression.
- Surveillance is essential for patients with Barrett esophagus because of the risk of progression.
- Invasive adenocarcinoma is identified by angulated glands invading the surrounding tissue, which causes a desmoplastic reaction.
- A single specimen can show Barrett esophagus, high-grade dysplasia, and invasive adenocarcinoma.
Esophageal Adenocarcinoma: Key Aspects
- Almost all esophageal adenocarcinoma cases arise in a Barrett esophagus background.
- Adenocarcinoma incidence is rising worldwide.
- Risk factors include obesity, smoking, radiation, and diets low in fresh fruits and vegetables.
- Some Helicobacter pylori serotypes are protective because they decrease gastric acid production.
- Patients present with pain and difficulty swallowing, which progresses to a liquid-only diet, and weight loss.
- Other presentations include hematemesis, chest pain, and vomiting.
- Early metastases to lymph nodes occur due to the location of lymphatics in the lamina propria.
- Tumors are typically advanced at diagnosis; overall five-year survival is less than 25%.
- Early detection through surveillance endoscopy allows for intramucosal resection and improved patient outcomes.
Pathogenesis of Adenocarcinoma
- Early TP53 and CDKN2A loss of function occurs (allelic loss, mutation, or epigenetic silencing via hypermethylation).
- CDKN2A encodes p16 and ARF proteins.
- P16 inhibits cyclin-dependent kinase 4 and 6, which blocks the RB tumor suppressor protein from entering the G1 phase.
- ARF inhibits MDM2, preventing it from binding to and degrading P53.
- Later mutations occur with disease progression, increasing risk with longer symptom duration, older age, and longer Barrett mucosa.
- Morphologically, lesions are often found in the distal third of the esophagus.
- Early lesions can be flat or raised in a Barrett esophagus background.
- Later lesions can be exophytic or ulcerated masses, showing diffuse infiltration or deep invasion.
- Most adenocarcinomas produce mucin and form glands.
- Metastasis typically occurs to gastric and celiac lymph nodes.
Squamous Cell Carcinoma: Key Aspects
- More common in men (4:1 ratio).
- Presentation is similar to adenocarcinoma.
- Risk factors:
- Alcohol and tobacco use (synergistic effect).
- Poverty and diets low in fresh fruits and vegetables.
- Caustic esophageal injury (e.g., lye ingestion).
- Plummer-Vinson syndrome: triad of dysphagia, iron deficiency anemia, and esophageal web; more common in middle-aged women.
- Achalasia: motility disorder causing loss of peristalsis and inability to relax the lower esophageal sphincter, which leads to upstream dilation.
- Frequent consumption of very hot beverages.
- Radiation exposure.
Pathogenesis and Morphology of Squamous Cell Carcinoma
- Pathogenesis is less clear than adenocarcinoma.
- SOX2 amplification, cyclin D1 overexpression, and loss of function of TP53, CDH1, and NOTCH1 are implicated.
- Tobacco and alcohol have a synergistic effect on risk.
- About 50% occur in the middle third of the esophagus.
- Squamous dysplasia appears as gray-white plaques; invasive carcinoma can be polypoid, ulcerated, or fungating.
- Most tumors are moderately to well-differentiated.
- Early metastasis to lymph nodes occurs, depending on the location in the esophagus:
- Upper third: cervical lymph nodes.
- Middle third: mediastinal, peritracheal, and tracheobronchial lymph nodes.
- Lower third: gastric and celiac nodes.
- Histologically, lesions invade the surrounding soft tissue with a desmoplastic response, forming necrotic cystic structures lacking mucin.
Comparison of Adenocarcinoma and Squamous Cell Carcinoma
- Similarities:
- Both malignancies can metastasize early to lymph nodes.
- Differences:
- Site.
- Main risk factors.
- Precursor lesions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.