Podcast
Questions and Answers
A lesion of the Vagus nerve can result in all of the following EXCEPT:
A lesion of the Vagus nerve can result in all of the following EXCEPT:
- Loss of sensation at the external auditory meatus
- Nasal quality of voice and regurgitation of liquids through the nose
- Immobilization of the vocal cord in a 'cadaveric position'
- Weakness of the sternocleidomastoid muscle and upper part of the trapezius (correct)
Which cranial nerve is responsible for supplying the musculature of the tongue?
Which cranial nerve is responsible for supplying the musculature of the tongue?
- Hypoglossal nerve (correct)
- Facial nerve
- Accessory nerve
- Vagus nerve
In Bulbar Palsy syndrome, which group of muscles is NOT typically involved?
In Bulbar Palsy syndrome, which group of muscles is NOT typically involved?
- Muscles of the pharynx and larynx
- Muscles of the tongue
- Sternocleidomastoids and upper trapezius (correct)
- Muscles of the face and jaw
What is the main function of the spinal accessory nerve (CN XI)?
What is the main function of the spinal accessory nerve (CN XI)?
If there is a complete lesion of the Hypoglossal nerve, what would happen when protruding the tongue?
If there is a complete lesion of the Hypoglossal nerve, what would happen when protruding the tongue?
Which symptom is NOT associated with a lesion of both pharyngeal branches of the Vagus nerve?
Which symptom is NOT associated with a lesion of both pharyngeal branches of the Vagus nerve?
Which division of the trigeminal nerve is responsible for sensory input from the cornea and conjunctiva?
Which division of the trigeminal nerve is responsible for sensory input from the cornea and conjunctiva?
What type of sensation is primarily associated with the principal sensory nucleus of the trigeminal nerve?
What type of sensation is primarily associated with the principal sensory nucleus of the trigeminal nerve?
What characterizes the pain experienced in trigeminal neuralgia?
What characterizes the pain experienced in trigeminal neuralgia?
What is the incidence rate of trigeminal neuralgia?
What is the incidence rate of trigeminal neuralgia?
What age group commonly experiences trigeminal neuralgia in its idiopathic form?
What age group commonly experiences trigeminal neuralgia in its idiopathic form?
What type of medication is reported to have a positive response in more than half of the cases of trigeminal neuralgia?
What type of medication is reported to have a positive response in more than half of the cases of trigeminal neuralgia?
What is the underlying mechanism of trigeminal neuralgia?
What is the underlying mechanism of trigeminal neuralgia?
What is the preferred imaging method for evaluating trigeminal neuralgia?
What is the preferred imaging method for evaluating trigeminal neuralgia?
Which is the most common cause of facial nerve palsy?
Which is the most common cause of facial nerve palsy?
What is the primary treatment for hemifacial spasm?
What is the primary treatment for hemifacial spasm?
What is an aberrant effect observed in patients recovering from facial nerve palsy?
What is an aberrant effect observed in patients recovering from facial nerve palsy?
Which disorder is characterized by painless, irregular clonic contractions of facial muscles on one side?
Which disorder is characterized by painless, irregular clonic contractions of facial muscles on one side?
What distinguishes glossopharyngeal neuralgia from trigeminal neuralgia?
What distinguishes glossopharyngeal neuralgia from trigeminal neuralgia?
What symptom is not commonly associated with Bell's Palsy?
What symptom is not commonly associated with Bell's Palsy?
Which treatment has no evidence supporting its effectiveness in Bell's Palsy?
Which treatment has no evidence supporting its effectiveness in Bell's Palsy?
'Glossopharyngeal neuralgia' manifests as stabbing pain in which area?
'Glossopharyngeal neuralgia' manifests as stabbing pain in which area?
In a syndrome of Bulbar Palsy, which of the following muscles is NOT typically involved?
In a syndrome of Bulbar Palsy, which of the following muscles is NOT typically involved?
If a patient has paralysis on one side of the tongue with slight deviation to the healthy side, which cranial nerve is most likely affected?
If a patient has paralysis on one side of the tongue with slight deviation to the healthy side, which cranial nerve is most likely affected?
Which cranial nerve is responsible for weakness of the sternocleidomastoid muscle and upper part of the trapezius when affected?
Which cranial nerve is responsible for weakness of the sternocleidomastoid muscle and upper part of the trapezius when affected?
Which condition is characterized by an aberrant effect where patients experience regurgitation of liquids through the nose during swallowing?
Which condition is characterized by an aberrant effect where patients experience regurgitation of liquids through the nose during swallowing?
When there is complete paralysis of both sides of the face, which condition should be considered?
When there is complete paralysis of both sides of the face, which condition should be considered?
What is the primary treatment for patients suffering from Hemifacial Spasm?
What is the primary treatment for patients suffering from Hemifacial Spasm?
Which condition is characterized by bilateral facial palsy?
Which condition is characterized by bilateral facial palsy?
What is considered a potential cause of secondary trigeminal neuralgia?
What is considered a potential cause of secondary trigeminal neuralgia?
Which condition may present with paroxysmal, brief, unilateral facial pain similar to trigeminal neuralgia?
Which condition may present with paroxysmal, brief, unilateral facial pain similar to trigeminal neuralgia?
What aberrant effect is commonly observed in patients recovering from facial nerve palsy?
What aberrant effect is commonly observed in patients recovering from facial nerve palsy?
Which tumor type could potentially lead to facial nerve palsy?
Which tumor type could potentially lead to facial nerve palsy?
What is a common treatment approach for managing hemifacial spasm?
What is a common treatment approach for managing hemifacial spasm?
What is a possible cause of bilateral facial palsy?
What is a possible cause of bilateral facial palsy?
Which condition may mimic the symptoms of hemifacial spasm?
Which condition may mimic the symptoms of hemifacial spasm?
What is an aberrant effect observed in some patients recovering from facial nerve palsy?
What is an aberrant effect observed in some patients recovering from facial nerve palsy?
Which condition is associated with synkinesis and eyelid closure during jaw movements?
Which condition is associated with synkinesis and eyelid closure during jaw movements?
What may cause painless, irregular clonic contractions of facial muscles on one side?
What may cause painless, irregular clonic contractions of facial muscles on one side?
Which disorder involves involuntary tearing whenever the patient salivates?
Which disorder involves involuntary tearing whenever the patient salivates?
What symptom is NOT commonly associated with hemifacial spasm?
What symptom is NOT commonly associated with hemifacial spasm?
Which condition may result in contracture with diffuse myokymic activity?
Which condition may result in contracture with diffuse myokymic activity?
What is the main pathological process believed to contribute to hemifacial spasm?
What is the main pathological process believed to contribute to hemifacial spasm?
Which condition can lead to a contraction of the eyelid during jaw movements in the affected side?
Which condition can lead to a contraction of the eyelid during jaw movements in the affected side?
Study Notes
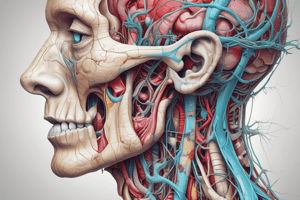
Cranial Nerve Palsies
- Lesion of the Vagus Nerve:
- Soft palate droops on the ipsilateral side and does not rise in phonation
- Uvula often deviates to the normal side on phonation
- Loss of the gag reflex on the affected side and of the curtain movements of the lateral wall of the pharynx
- Voice is hoarse, often nasal
- Lesion of the Hypoglossal Nerve:
- Supplies the musculature of the tongue
- Complete interruption of the nerve results in paralysis on one side of the tongue
- Tongue curves slightly to the healthy side as it lies on the mouth
- Deviates to the affected side on protrusion of the tongue
- Syndrome of Bulbar Palsy:
- Result of weakness or paralysis of muscles that are supplied by the motor nuclei of the lower brainstem (5th, 7th and 9th-12th cranial nerves)
- Involved muscles: face and jaw, sternocleidomastoids and upper part of the trapezii, muscles of the tongue, pharynx, and larynx
Trigeminal Nerve
- Anatomy:
- Mixed sensory and motor
- Sensory: greater part of the head and face, mucous membranes of the nose, mouth and paranasal sinuses, cornea and conjunctiva, dura in the anterior and middle cranial fossa
- Gasserian or semilunar ganglion: cell body; largest sensory ganglion
- 3 sensory nuclei: principal sensory nucleus (tactile and light pressure sensation), mesencephalic nucleus (proprioception), spinal trigeminal nucleus (pain and temperature sensation)
- 3 sensory divisions: ophthalmic division (V1), maxillary division (V2), mandibular division (V3)
- Motor: masseter and pterygoid muscles; motor nucleus in the midpons
- Trigeminal Neuralgia:
- Tic douloureux; incidence rate: 4.3/100,000 persons per year
- Higher in women than men (ratio of 3:2) and elderly
- Mean age of onset: 52-58 years in idiopathic form, 32-35 years in symptomatic form
- Characteristic features:
- Paroxysmal, brief, unilateral facial pain
- Tendency to involve V2 or V3
- Pain intensity makes the patient grimace or wince (tic)
- Presence of a trigger point on the face
- Lack of demonstrable sensory or motor deficit
- Response in more than half of the cases to anti-seizure medications
- Trigeminal Neuropathy:
- Numbness in one or more branches of the trigeminal nerve, sometimes associated with paresthesia or neuropathic pain
- Etiologies: facial and cranial injuries, postherpetic neuralgia, numb chin syndrome, compression by tumors
Facial Nerve
- Anatomy:
- Mainly a motor nerve
- Muscles of facial expression
- Sensory component (small): nervus intermedius of Wrisberg; taste sensation from the anterior two-thirds of the tongue; cutaneous sensation from the anterior wall of the external auditory canal
- Superior salivatory nucleus: secretomotor fibers to the lacrimal gland and sublingual and submaxillary glands
- Bell's Palsy:
- Most common disease of the facial nerve
- Incidence rate: 23 per 100,000 people annually
- Probably more common in diabetic and hypertensive patients
- A viral agent has long been suspected as a causative agent (Herpes simplex virus type I)
- Onset is acute
- One-half of cases attain maximum paralysis within 48 hours and all within 3 or 4 days
- Clinical features:
- Peripheral type of facial paralysis
- Pain behind the ear may precede the paralysis by a day or two
- Taste impairment is present in most patients
- Rarely persists beyond the second week of paralysis
- Hyperacusis (paralysis of the stapedius muscle)
- A report by the patient of fullness or numbness of the face
- Course:
- Fully 70% of patients recover completely within a month or two
- 85% achieve near-normal facial function
- Recovery of taste precedes recovery of motor function
- If taste returns in the first week, it is a good prognostic sign
- Early recovery of some motor function in the first 5-7 days is the most favorable sign
- Recurs in approximately 8%
- Treatment:
- Protection of the eye during sleep
- No evidence that surgical decompression of the facial nerve is effective
- Prednisone (40-60 mg/day) during the first week to 10 days after onset
- Evidence fails to support the use of antiviral drugs
- Other Causes of Palsy:
- Lyme disease
- HIV infection
- Leprosy
- Sarcoidosis
- Ramsay Hunt syndrome
- Herpes zoster of the geniculate ganglion
- Facial palsy + vesicular eruption of the external auditory canal + 8th cranial nerve involvement
- Tumors
- Bilateral facial palsy: Guillain-Barre syndrome, Lyme disease, HIV infection, sarcoidosis, Melkersson-Rosenthal syndrome (triad of recurrent facial paralysis, facial edema, and plication of the tongue)
- Aberrant Effects of Recovery from Facial Nerve Palsy:
- Contracture with diffuse myokymic activity
- Aberrant regeneration of the facial nerve
- Synkinesis
- Eyelid closure during contraction of the orbicularis oris
- Crocodile tears: anomalous tearing whenever the patient salivates
- Jaw-winking phenomenon: jaw movements cause an involuntary closure of the eyelid ipsilateral to the movement
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge on the anatomy and functions of the cranial nerves with a focus on the trigeminal nerve. Explore information about the sensory and motor components as well as key anatomical structures and their functions.