Podcast
Questions and Answers
What is a clinical presentation of trochlear palsy?
What is a clinical presentation of trochlear palsy?
- Eye is elevated and adducted (correct)
- Eye is depressed and abducted
- Eye is rotated inward towards the nose
- Eye appears to be drooping and misaligned
Which nerve is responsible for somatic sensory functions in the ophthalmic region?
Which nerve is responsible for somatic sensory functions in the ophthalmic region?
- Trigeminal Nerve V1 (correct)
- Facial Nerve
- Optic Nerve
- Trigeminal Nerve V3
Which foramen does the maxillary division of the trigeminal nerve pass through?
Which foramen does the maxillary division of the trigeminal nerve pass through?
- Jugular foramen
- Foramen rotundum (correct)
- Superior orbital fissure
- Foramen ovale
What is the primary function of the mandibular division of the trigeminal nerve?
What is the primary function of the mandibular division of the trigeminal nerve?
Which area of the brain is associated with the trigeminal sensory ganglion?
Which area of the brain is associated with the trigeminal sensory ganglion?
Which sensory modality is primarily responsible for general sensation from the skin?
Which sensory modality is primarily responsible for general sensation from the skin?
Which cranial nerve pair is primarily responsible for the sense of smell?
Which cranial nerve pair is primarily responsible for the sense of smell?
What type of motor function do skeletal muscles fall under?
What type of motor function do skeletal muscles fall under?
Cranial Nerve II is primarily associated with which function?
Cranial Nerve II is primarily associated with which function?
Which modality refers to the general sensory functions from the viscera?
Which modality refers to the general sensory functions from the viscera?
Which cranial nerves originate from the pharyngeal arches?
Which cranial nerves originate from the pharyngeal arches?
What type of sensory function do specialized sensory modalities like sight and sound fall under?
What type of sensory function do specialized sensory modalities like sight and sound fall under?
What is the significance of understanding cranial fossae and foramina for cranial nerves?
What is the significance of understanding cranial fossae and foramina for cranial nerves?
What is the primary function of the Olfactory Nerve (CN I)?
What is the primary function of the Olfactory Nerve (CN I)?
Where do the fibers of the Olfactory Nerve (CN I) synapse?
Where do the fibers of the Olfactory Nerve (CN I) synapse?
In which cranial fossa do the Olfactory Nerve (CN I) fibers pass through the cribriform plate?
In which cranial fossa do the Olfactory Nerve (CN I) fibers pass through the cribriform plate?
What clinical relevance does the cribriform plate hold?
What clinical relevance does the cribriform plate hold?
Which sensory function is associated with the Optic Nerve (CN II)?
Which sensory function is associated with the Optic Nerve (CN II)?
Where do retinal ganglion cell axons from the Optic Nerve (CN II) pass through?
Where do retinal ganglion cell axons from the Optic Nerve (CN II) pass through?
After the optic chiasm, where do the axons of the Optic Nerve (CN II) continue?
After the optic chiasm, where do the axons of the Optic Nerve (CN II) continue?
What structure do the optic radiations project to?
What structure do the optic radiations project to?
What is the primary motor function of the Facial Nerve (CN VII)?
What is the primary motor function of the Facial Nerve (CN VII)?
Which ganglion is associated with the sensory function of the Facial Nerve?
Which ganglion is associated with the sensory function of the Facial Nerve?
What is a common clinical presentation associated with Bell's Palsy?
What is a common clinical presentation associated with Bell's Palsy?
What is the usual duration for self-resolution of Bell's Palsy?
What is the usual duration for self-resolution of Bell's Palsy?
Which foramen does the Facial Nerve NOT pass through?
Which foramen does the Facial Nerve NOT pass through?
Which symptom is associated with a lesion of the Vestibulocochlear Nerve (CN VIII)?
Which symptom is associated with a lesion of the Vestibulocochlear Nerve (CN VIII)?
The cochlear ganglia are involved in which type of sensory function?
The cochlear ganglia are involved in which type of sensory function?
What type of nerve is the Vestibulocochlear Nerve (CN VIII)?
What type of nerve is the Vestibulocochlear Nerve (CN VIII)?
What condition can result from optic nerve damage due to trauma or increased intraocular pressure?
What condition can result from optic nerve damage due to trauma or increased intraocular pressure?
Which muscle is innervated by the oculomotor nerve?
Which muscle is innervated by the oculomotor nerve?
What is the primary function of the trochlear nerve?
What is the primary function of the trochlear nerve?
What structure does the oculomotor nerve pass through to enter the orbit?
What structure does the oculomotor nerve pass through to enter the orbit?
Which action is NOT associated with the superior oblique muscle innervated by the trochlear nerve?
Which action is NOT associated with the superior oblique muscle innervated by the trochlear nerve?
What does a sudden onset of CN III palsy typically indicate?
What does a sudden onset of CN III palsy typically indicate?
Which intraocular muscles receive parasympathetic innervation from the oculomotor nerve?
Which intraocular muscles receive parasympathetic innervation from the oculomotor nerve?
Where does the trochlear nerve originate?
Where does the trochlear nerve originate?
Which muscle is innervated by the spinal accessory nerve (CN XI)?
Which muscle is innervated by the spinal accessory nerve (CN XI)?
What is the effect of a complete lesion of the vagus nerve (CN X)?
What is the effect of a complete lesion of the vagus nerve (CN X)?
Which of the following statements regarding CN XII lesions is true?
Which of the following statements regarding CN XII lesions is true?
Which cranial nerve is responsible for the somatic efferent innervation to tongue muscles?
Which cranial nerve is responsible for the somatic efferent innervation to tongue muscles?
Where is the hypoglossal nucleus located?
Where is the hypoglossal nucleus located?
Which cranial nerve provides motor commands from the frontal lobe for neck and shoulder movement?
Which cranial nerve provides motor commands from the frontal lobe for neck and shoulder movement?
What would likely result from a lesion superior to the hypoglossal nucleus?
What would likely result from a lesion superior to the hypoglossal nucleus?
Which of the following pharmacotherapeutics take advantage of the effects of the vagus nerve?
Which of the following pharmacotherapeutics take advantage of the effects of the vagus nerve?
Flashcards
CN I, Olfactory Nerve
CN I, Olfactory Nerve
The first cranial nerve (CN I), also known as the olfactory nerve, transmits information about smell. It carries special visceral sensory (SVS) information, responsible for the sense of smell.
CN II, Optic Nerve
CN II, Optic Nerve
The second cranial nerve (CN II), also known as the optic nerve, carries special somatic sensory (SSS) information, responsible for vision. It transmits information about sight from the retina of the eye to the brain.
CN III, Oculomotor Nerve
CN III, Oculomotor Nerve
The third cranial nerve (CN III), also known as the oculomotor nerve, controls most of the eye's movements. It is responsible for four of the six extraocular muscles that move the eye, raising the upper eyelid, and controlling pupil constriction and lens accommodation.
CN IV, Trochlear Nerve
CN IV, Trochlear Nerve
Signup and view all the flashcards
CN V, Trigeminal Nerve
CN V, Trigeminal Nerve
Signup and view all the flashcards
CN VI, Abducens Nerve
CN VI, Abducens Nerve
Signup and view all the flashcards
CN VII, Facial Nerve
CN VII, Facial Nerve
Signup and view all the flashcards
CN VIII, Vestibulocochlear Nerve
CN VIII, Vestibulocochlear Nerve
Signup and view all the flashcards
Olfactory Nerve (CN I)
Olfactory Nerve (CN I)
Signup and view all the flashcards
Clinical Relevance of Olfactory Nerve Trauma
Clinical Relevance of Olfactory Nerve Trauma
Signup and view all the flashcards
Optic Nerve (CN II)
Optic Nerve (CN II)
Signup and view all the flashcards
Optic Chiasm
Optic Chiasm
Signup and view all the flashcards
Lateral Geniculate Nucleus (LGN)
Lateral Geniculate Nucleus (LGN)
Signup and view all the flashcards
Optic Radiations
Optic Radiations
Signup and view all the flashcards
Optic Tract
Optic Tract
Signup and view all the flashcards
Visual Cortex
Visual Cortex
Signup and view all the flashcards
Optic Nerve Damage - Clinical Relevance
Optic Nerve Damage - Clinical Relevance
Signup and view all the flashcards
Oculomotor Nerve - Muscles Innervated
Oculomotor Nerve - Muscles Innervated
Signup and view all the flashcards
Oculomotor Nerve Palsy - Clinical Significance
Oculomotor Nerve Palsy - Clinical Significance
Signup and view all the flashcards
Trochlear Nerve - Muscle Innervated & Actions
Trochlear Nerve - Muscle Innervated & Actions
Signup and view all the flashcards
Oculomotor Nerve Palsy - Clinical Significance
Oculomotor Nerve Palsy - Clinical Significance
Signup and view all the flashcards
Trochlear Nerve - Size
Trochlear Nerve - Size
Signup and view all the flashcards
Trochlear Nerve - Origin & Pathway
Trochlear Nerve - Origin & Pathway
Signup and view all the flashcards
Trochlear Nerve - Nucleus Location
Trochlear Nerve - Nucleus Location
Signup and view all the flashcards
Trochlear Palsy
Trochlear Palsy
Signup and view all the flashcards
Trigeminal Nerve Divisions
Trigeminal Nerve Divisions
Signup and view all the flashcards
Ophthalmic Division (V1)
Ophthalmic Division (V1)
Signup and view all the flashcards
Maxillary Division (V2)
Maxillary Division (V2)
Signup and view all the flashcards
Mandibular Division (V3)
Mandibular Division (V3)
Signup and view all the flashcards
What is the function of the Facial Nerve (CN VII)?
What is the function of the Facial Nerve (CN VII)?
Signup and view all the flashcards
What is Bell's Palsy?
What is Bell's Palsy?
Signup and view all the flashcards
How is Bell's Palsy treated?
How is Bell's Palsy treated?
Signup and view all the flashcards
What is the function of the Vestibulocochlear Nerve (CN VIII)?
What is the function of the Vestibulocochlear Nerve (CN VIII)?
Signup and view all the flashcards
What can happen if the Vestibulocochlear Nerve (CN VIII) is damaged?
What can happen if the Vestibulocochlear Nerve (CN VIII) is damaged?
Signup and view all the flashcards
Where does the Vestibulocochlear Nerve (CN VIII) originate and exit the skull?
Where does the Vestibulocochlear Nerve (CN VIII) originate and exit the skull?
Signup and view all the flashcards
What are the two branches of the Vestibulocochlear Nerve (CN VIII)?
What are the two branches of the Vestibulocochlear Nerve (CN VIII)?
Signup and view all the flashcards
How does the Vestibulocochlear Nerve transmit information?
How does the Vestibulocochlear Nerve transmit information?
Signup and view all the flashcards
Vagus Nerve (CN X) - Clinical Considerations
Vagus Nerve (CN X) - Clinical Considerations
Signup and view all the flashcards
Spinal Accessory Nerve (CN XI)
Spinal Accessory Nerve (CN XI)
Signup and view all the flashcards
CNXI - Motor Only
CNXI - Motor Only
Signup and view all the flashcards
CN XI - Muscle Innervation
CN XI - Muscle Innervation
Signup and view all the flashcards
Hypoglossal Nerve (CN XII)
Hypoglossal Nerve (CN XII)
Signup and view all the flashcards
CN XII - Motor Only
CN XII - Motor Only
Signup and view all the flashcards
UMN (CBT) vs. LMN (CN XII) Lesions
UMN (CBT) vs. LMN (CN XII) Lesions
Signup and view all the flashcards
Genioglossus Muscle - CN XII Relation
Genioglossus Muscle - CN XII Relation
Signup and view all the flashcards
Study Notes
Disclosures
- The presenter has no relationships with companies whose products or services relate to medicine, medical education, or research.
Suggested Reading
- Neuroscience for Dentistry by O'Kane and Barritt, 2022, Chapter 9
- Teach Me Anatomy articles on the Cranial Nerves, including the Summary of the Cranial Nerves by Katherine Sanders
Nervous System Modalities
- Sensory (afferent):
- General somatic sensory (GSS): general sensation from skin
- General visceral sensory (GVS): general sensation from internal organs
- Special somatic sensory (SSS): senses from ectoderm (sight, sound, balance)
- Special visceral sensory (SVS): senses from endoderm (taste, smell)
- Motor (efferent):
- General somatic motor (GSM): skeletal muscles
- General visceral motor (GVM): smooth muscles of the gut and autonomic motor
- Special visceral motor (SVM): muscles derived from pharyngeal arches
Learning Objectives
- Correlate cranial nerve (CN) numbers with their names.
- Explain the basic sensory and/or motor functions of each CN.
- Identify the origin of each CN in the central nervous system.
- Identify the cranial fossae and foramina each CN travels through.
- Describe the location of ganglia and nuclei for each CN.
- Identify the cortical region for each CN (origin or destination of signal).
- Predict signs and symptoms if a CN is lesioned.
Cranial Nerve I (Olfactory)
- Sensory only, specifically for olfaction (smell).
- Originates from the forebrain.
- Fibers pass through foramina of the cribriform plate (ethmoid bone).
- Located in the anterior cranial fossa.
- Synapse in olfactory glomeruli of the olfactory bulb (continuous with olfactory tract).
- Projects to the olfactory cortex of the temporal lobe.
Clinical Relevance of CN I
- The cribriform plate is a weak spot in the anterior cranial fossa.
- Trauma or fracture to this area can cause anosmia (loss of smell).
Cranial Nerve II (Optic)
- Sensory only, for vision.
- Originates from the forebrain (retinal ganglion cell axons).
- Passes through the optic canal.
- The optic chiasm is located in the middle cranial fossa.
- Axons continue in the optic tract.
- Lateral Geniculate Nucleus (LGN) in the thalamus processes signals.
- Optic radiations project to the occipital lobe.
Clinical Relevance of CN II
- Optic nerve transection (trauma) or other damage (increased intraocular pressure, tumor) results in anopsia (unilateral blindness).
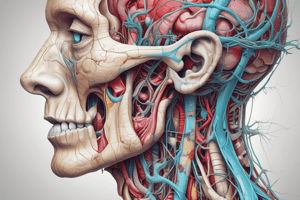
Cranial Nerve III (Oculomotor)
- Motor only, controlling extraocular muscles.
- Innervates superior rectus, medial rectus, inferior rectus, inferior oblique, and levator palpebrae superioris muscles.
- Contains parasympathetic innervation for intraocular muscles (pupillary constrictor and ciliary muscle).
- Originates from the midbrain.
- Passes into the orbit through the superior orbital fissure.
- Located in the middle cranial fossa.
Clinical Presentation of CN III Palsy
- Isolated CN III palsy suggests possible trauma, aneurysm, or brain herniation.
- Symptoms include ptosis (drooping eyelid), mydriasis (pupil dilation), and down and out deviation of the eye.
Cranial Nerve IV (Trochlear)
- Motor only, controlling the superior oblique muscle.
- Actions include intorsion, depression, and abduction.
- Originates from the dorsal midbrain.
- Passes into the orbit through the superior orbital fissure.
- Located in the middle cranial fossa.
- Trochlear nucleus is located within the midbrain.
Cranial Nerve V (Trigeminal)
- Mixed nerve (sensory and motor).
- Three divisions: ophthalmic (V1), maxillary (V2), and mandibular (V3).
- Sensory functions include sensation from the face, nasal cavity, and mouth.
- Motor functions control muscles of mastication (chewing).
- Sensory and motor nuclei are located in the pons.
- Foramina include the superior orbital fissure, foramen rotundum, and foramen ovale.
Cranial Nerve VI (Abducens)
- Motor only, controlling the lateral rectus muscle (for abduction).
- Originates from the pontomedullary junction.
- Passes into the orbit through the superior orbital fissure.
- Located in the middle cranial fossa.
- Contains the abducens ganglion in the pons.
- Cortex is located in the frontal lobe.
Cranial Nerve VII (Facial)
- Mixed nerve (sensory and motor).
- Motor functions innervate muscles of facial expression.
- Sensory functions provide taste from the anterior two-thirds of the tongue, and general sensation from skin behind the ear.
- Important parasympathetic functions include salivation and lacrimation.
- Contains various branches for different functions.
- Originates from the pontomedullary junction, passes through the internal acoustic meatus and stylomastoid foramen.
Clinical Considerations for CN VII
- Bell's palsy, cause: idiopathic, Treatment: Corticosteroids,Typically self-resolving within ~6 months, Protect the affected eye, Prevent
Cranial Nerve VIII (Vestibulocochlear)
- Sensory only, for hearing and balance.
- Has cochlear (hearing) and vestibular (balance) components.
- Originates from the pontomedullary junction.
- Passes through the internal acoustic meatus.
- Lesions may result in unilateral hearing loss or vertigo.
Clinical Considerations for CN VIII
- Labyrinthitis: inflammation of the membranous labyrinth causing damage to vestibular and cochlear branches; symptoms include hearing loss, tinnitus.
Cranial Nerve IX (Glossopharyngeal)
- Mixed nerve (sensory and motor).
- Sensory: General sensation from the posterior tongue, oropharynx, middle ear, and Eustachian tube; taste from the posterior tongue.
- Motor: controlling the stylopharyngeus muscle, and parasympathetic functions affecting the parotid gland.
- Originates in the medulla.
- Passes through the posterior cranial fossa to exit the jugular foramen.
- Nuclei located within the medulla.
- Tongue taste registers in the insular cortex
Cranial Nerve X (Vagus)
- Mixed nerve (sensory and motor).
- Sensory: larynx, pharynx, thoracic and abdominal organs
- Taste from the epiglottis
- Motor: larynx, pharynx, and soft palate, parasympathetic functions influencing the trachea, bronchi, gastrointestinal tract, and heart rhythm.
- Originates in the medulla.
- Passes through posterior cranial fossa to exit the jugular foramen.
- Nuclei located within medulla.
- Taste registers within the insular cortex
Clinical Considerations for CN X
- Complete CN X lesions are rare.
- Some branches are susceptible to compression (like the recurrent laryngeal nerve).
Cranial Nerve XI (Spinal Accessory)
- Motor only, innervating the sternocleidomastoid and trapezius muscles.
- Originates in the medulla and upper cervical spinal cord.
- Passes through posterior cranial fossa and jugular foramen (spinal part passes through the foramen magnum).
- Nuclei located within the medulla and upper cervical spinal cord.
- Cortex responsible for motor commands is in the frontal lobe.
- Iatrogenic trauma (such as surgery) is a common cause of damage.
Clinical Considerations for CN XI
- Damage often presents as muscle wasting and partial paralysis in the sternocleidomastoid and trapezius muscles.
Cranial Nerve XII (Hypoglossal)
- Motor only, controls muscles of the tongue.
- Innervates genioglossus, hyoglossus, and styloglossus muscles.
- Originates in the medulla.
- Passes through the posterior cranial fossa exiting via the hypoglossal canal.
- Nuclei located in the medulla.
- Cortex responsible for motor commands is in the frontal lobe.
UMN (Central) vs. LMN (Peripheral) Lesions
- UMN lesions (superior to the hypoglossal nucleus) result in contralateral tongue deviation.
- LMN lesions (inferior to the hypoglossal nucleus) result in ipsilateral tongue deviation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.