Podcast
Questions and Answers
A patient's MRI report indicates 'bulging of the disc beyond the normal annular margin with intact outer rings'. According to the provided information, which stage of disc herniation best describes this finding?
A patient's MRI report indicates 'bulging of the disc beyond the normal annular margin with intact outer rings'. According to the provided information, which stage of disc herniation best describes this finding?
- Prolapse (correct)
- Degeneration
- Sequestration
- Extrusion
Why is a posterolateral disc herniation considered the most common type?
Why is a posterolateral disc herniation considered the most common type?
- Nerve roots are primarily located anteriorly, making posterolateral herniations more symptomatic.
- The ligamentum flavum is thickest posterolaterally, predisposing to herniation.
- The vertebral body is wider posterolaterally, creating more space for disc protrusion.
- The posterior annulus is structurally weaker and thinner than the anterior annulus. (correct)
A patient presents with low back pain radiating down their leg, exacerbated by bending forward and twisting. Which finding would MOST strongly suggest a disc herniation as the source of their pain, according to the provided information?
A patient presents with low back pain radiating down their leg, exacerbated by bending forward and twisting. Which finding would MOST strongly suggest a disc herniation as the source of their pain, according to the provided information?
- Presence of neurological signs such as weakness or numbness. (correct)
- Pain that is worse when standing or walking.
- Increased pain with activities like sitting for prolonged periods.
- Pain relief with rest and lying down.
Which of the following is the MOST appropriate initial treatment approach for a patient diagnosed with a disc herniation and experiencing low back pain with radiating pain, but without progressive neurological deficits?
Which of the following is the MOST appropriate initial treatment approach for a patient diagnosed with a disc herniation and experiencing low back pain with radiating pain, but without progressive neurological deficits?
A patient is concerned about undergoing surgery for a disc herniation. Based on the provided information, what is an important point to emphasize regarding the natural course of disc herniations?
A patient is concerned about undergoing surgery for a disc herniation. Based on the provided information, what is an important point to emphasize regarding the natural course of disc herniations?
A patient presents with lower back pain and an X-ray reveals a 60% anterior slippage of L5 on S1. According to the Meyerding classification, what grade of spondylolisthesis does this represent?
A patient presents with lower back pain and an X-ray reveals a 60% anterior slippage of L5 on S1. According to the Meyerding classification, what grade of spondylolisthesis does this represent?
Which of the following best describes the underlying pathology of a Schmorl's node?
Which of the following best describes the underlying pathology of a Schmorl's node?
A physical therapist is treating a patient with a low-grade spondylolisthesis. Which of the following exercise approaches would be MOST appropriate?
A physical therapist is treating a patient with a low-grade spondylolisthesis. Which of the following exercise approaches would be MOST appropriate?
Which of the following findings would be MOST indicative of facet joint involvement in a patient's lower back pain?
Which of the following findings would be MOST indicative of facet joint involvement in a patient's lower back pain?
A patient's X-ray report indicates the presence of osteophytes and cartilage loss in the lumbar spine. Which of the following conditions BEST aligns with these findings?
A patient's X-ray report indicates the presence of osteophytes and cartilage loss in the lumbar spine. Which of the following conditions BEST aligns with these findings?
A gymnast reports experiencing lower back pain that worsens with hyperextension exercises. An X-ray reveals a 'Scotty Dog' fracture. What condition is MOST likely indicated by these findings?
A gymnast reports experiencing lower back pain that worsens with hyperextension exercises. An X-ray reveals a 'Scotty Dog' fracture. What condition is MOST likely indicated by these findings?
A patient diagnosed with spondylolysis is being treated conservatively. Which intervention would be MOST appropriate?
A patient diagnosed with spondylolysis is being treated conservatively. Which intervention would be MOST appropriate?
What is the PRIMARY difference between spondylolysis and spondylolisthesis?
What is the PRIMARY difference between spondylolysis and spondylolisthesis?
A patient presents with lower back pain. Imaging reveals anterior displacement of L5 over S1. This is MOST consistent with:
A patient presents with lower back pain. Imaging reveals anterior displacement of L5 over S1. This is MOST consistent with:
Which of the following best describes the 'Scotty Dog' sign and its clinical significance?
Which of the following best describes the 'Scotty Dog' sign and its clinical significance?
A patient reports pain and paresthesia radiating down their leg, following the path of the sciatic nerve, but not corresponding to a specific dermatomal pattern. They also exhibit mild weakness in ankle dorsiflexion. Which condition is MOST consistent with these findings?
A patient reports pain and paresthesia radiating down their leg, following the path of the sciatic nerve, but not corresponding to a specific dermatomal pattern. They also exhibit mild weakness in ankle dorsiflexion. Which condition is MOST consistent with these findings?
A patient presents with carpal tunnel syndrome symptoms, and upon further examination, also shows signs of nerve root compression at the C6 level. This scenario BEST illustrates which concept?
A patient presents with carpal tunnel syndrome symptoms, and upon further examination, also shows signs of nerve root compression at the C6 level. This scenario BEST illustrates which concept?
Which treatment strategy would be MOST directly aimed at addressing the 'space' component of nerve health in a patient with femoral nerve mechanosensitivity?
Which treatment strategy would be MOST directly aimed at addressing the 'space' component of nerve health in a patient with femoral nerve mechanosensitivity?
A patient with acute low back pain presents with palpable muscle tightness and guarding in the lumbar paraspinal muscles. This muscle spasm is BEST interpreted as:
A patient with acute low back pain presents with palpable muscle tightness and guarding in the lumbar paraspinal muscles. This muscle spasm is BEST interpreted as:
A patient reports localized, aching low back pain and stiffness that is worsened by prolonged sitting and relieved by gentle stretching. Range of motion in lumbar extension and lateral flexion is limited and painful. These findings are MOST indicative of:
A patient reports localized, aching low back pain and stiffness that is worsened by prolonged sitting and relieved by gentle stretching. Range of motion in lumbar extension and lateral flexion is limited and painful. These findings are MOST indicative of:
Which of the following is the MOST likely cause of radiculopathy in a 45-year-old male?
Which of the following is the MOST likely cause of radiculopathy in a 45-year-old male?
A patient presents with bilateral lower extremity symptoms and neurogenic claudication. Imaging reveals narrowing of the spinal cord space. Which condition is MOST consistent with these findings?
A patient presents with bilateral lower extremity symptoms and neurogenic claudication. Imaging reveals narrowing of the spinal cord space. Which condition is MOST consistent with these findings?
Which of the following characteristics is MOST indicative of foraminal stenosis rather than central stenosis?
Which of the following characteristics is MOST indicative of foraminal stenosis rather than central stenosis?
A patient with suspected nerve entrapment reports pain and paresthesia along the affected nerve's distribution. Which underlying mechanism is MOST likely contributing to these symptoms?
A patient with suspected nerve entrapment reports pain and paresthesia along the affected nerve's distribution. Which underlying mechanism is MOST likely contributing to these symptoms?
What is the MOST likely underlying cause of neurogenic claudication in central stenosis?
What is the MOST likely underlying cause of neurogenic claudication in central stenosis?
Which of the following is a typical sign or symptom associated with radiculopathy?
Which of the following is a typical sign or symptom associated with radiculopathy?
What is the primary mechanism behind the development of foraminal stenosis?
What is the primary mechanism behind the development of foraminal stenosis?
A patient presents with unilateral leg pain, numbness, and weakness. The symptoms worsen with spinal extension and improve with flexion. Which condition is MOST likely?
A patient presents with unilateral leg pain, numbness, and weakness. The symptoms worsen with spinal extension and improve with flexion. Which condition is MOST likely?
An older adult patient presents with back pain that worsens with extension and rotation. Based on the provided information, which of the following conservative treatments would be MOST appropriate as an initial approach?
An older adult patient presents with back pain that worsens with extension and rotation. Based on the provided information, which of the following conservative treatments would be MOST appropriate as an initial approach?
A 35-year-old female patient who recently gave birth reports low back pain. She describes the pain as sharp and occasionally tingling, worsened by prolonged sitting and transitioning from sitting to standing. Based on the provided information, which condition is MOST likely contributing to her symptoms?
A 35-year-old female patient who recently gave birth reports low back pain. She describes the pain as sharp and occasionally tingling, worsened by prolonged sitting and transitioning from sitting to standing. Based on the provided information, which condition is MOST likely contributing to her symptoms?
Which of the following activities is LEAST likely to aggravate pain originating from the sacroiliac (SI) joint, according to the provided information?
Which of the following activities is LEAST likely to aggravate pain originating from the sacroiliac (SI) joint, according to the provided information?
A physical therapist is designing a treatment plan for a patient diagnosed with sacroiliac (SI) joint dysfunction related to hypermobility. Which conservative treatment strategy would be MOST directly aimed at addressing the underlying cause of this patient's SI joint pain?
A physical therapist is designing a treatment plan for a patient diagnosed with sacroiliac (SI) joint dysfunction related to hypermobility. Which conservative treatment strategy would be MOST directly aimed at addressing the underlying cause of this patient's SI joint pain?
Degenerative Disc Disease (DDD) is characterized by a decrease in proteoglycans within the intervertebral disc. How does this biochemical change DIRECTLY contribute to increased facet joint loading?
Degenerative Disc Disease (DDD) is characterized by a decrease in proteoglycans within the intervertebral disc. How does this biochemical change DIRECTLY contribute to increased facet joint loading?
Imaging studies reveal disc degeneration in a 70-year-old patient presenting with back pain. Considering the prevalence of Degenerative Disc Disease (DDD) in asymptomatic individuals of this age group, what is the MOST accurate interpretation of these imaging findings?
Imaging studies reveal disc degeneration in a 70-year-old patient presenting with back pain. Considering the prevalence of Degenerative Disc Disease (DDD) in asymptomatic individuals of this age group, what is the MOST accurate interpretation of these imaging findings?
According to the provided information, which statement BEST compares the prevalence of disc bulge and disc herniation in asymptomatic individuals aged 60-80?
According to the provided information, which statement BEST compares the prevalence of disc bulge and disc herniation in asymptomatic individuals aged 60-80?
While lifestyle factors are considered potential contributors to Degenerative Disc Disease (DDD), the provided text emphasizes a 'strong genetic link'. What does this imply regarding the relative influence of genetics versus lifestyle in the development of DDD?
While lifestyle factors are considered potential contributors to Degenerative Disc Disease (DDD), the provided text emphasizes a 'strong genetic link'. What does this imply regarding the relative influence of genetics versus lifestyle in the development of DDD?
Flashcards
Spondylolysis
Spondylolysis
A fracture in the pars interarticularis without vertebral displacement.
Spondylolisthesis
Spondylolisthesis
Fracture of the pars interarticularis with anterior displacement of the vertebral body.
Spondylolysis cause
Spondylolysis cause
Often caused by repeated or excessive end-range extension.
Scotty Dog collar sign
Scotty Dog collar sign
Signup and view all the flashcards
Spondylolysis treatment
Spondylolysis treatment
Signup and view all the flashcards
Meyerding Scale
Meyerding Scale
Signup and view all the flashcards
Schmorl's Nodes
Schmorl's Nodes
Signup and view all the flashcards
Spondylosis/DJD/OA
Spondylosis/DJD/OA
Signup and view all the flashcards
Facet Joint Symptoms
Facet Joint Symptoms
Signup and view all the flashcards
Posterolateral Disc Herniation
Posterolateral Disc Herniation
Signup and view all the flashcards
Disc Degeneration
Disc Degeneration
Signup and view all the flashcards
Disc Prolapse
Disc Prolapse
Signup and view all the flashcards
Disc Extrusion
Disc Extrusion
Signup and view all the flashcards
Disc Sequestration
Disc Sequestration
Signup and view all the flashcards
Nerve Mechanosensitivity
Nerve Mechanosensitivity
Signup and view all the flashcards
Nerve Entrapment Symptoms
Nerve Entrapment Symptoms
Signup and view all the flashcards
Double Crush
Double Crush
Signup and view all the flashcards
Nerve Health Essentials
Nerve Health Essentials
Signup and view all the flashcards
Muscle Strain
Muscle Strain
Signup and view all the flashcards
CPG
CPG
Signup and view all the flashcards
Radiculopathy
Radiculopathy
Signup and view all the flashcards
Spinal Stenosis
Spinal Stenosis
Signup and view all the flashcards
Nerve Entrapment
Nerve Entrapment
Signup and view all the flashcards
Central Stenosis
Central Stenosis
Signup and view all the flashcards
Foraminal Stenosis
Foraminal Stenosis
Signup and view all the flashcards
Nerve Tethering
Nerve Tethering
Signup and view all the flashcards
Central Stenosis Symptoms
Central Stenosis Symptoms
Signup and view all the flashcards
Facet Arthritis Treatment
Facet Arthritis Treatment
Signup and view all the flashcards
SI Joint Dysfunction - Causes
SI Joint Dysfunction - Causes
Signup and view all the flashcards
SI Joint Dysfunction - Symptoms
SI Joint Dysfunction - Symptoms
Signup and view all the flashcards
SI Joint Dysfunction - Treatment
SI Joint Dysfunction - Treatment
Signup and view all the flashcards
Disc Herniation Prevalence
Disc Herniation Prevalence
Signup and view all the flashcards
DDD Prevalence
DDD Prevalence
Signup and view all the flashcards
Disc Bulge Prevalence
Disc Bulge Prevalence
Signup and view all the flashcards
Degenerative Disc Disease
Degenerative Disc Disease
Signup and view all the flashcards
Study Notes
- Lumbopelvic Pathology addresses the classification of low back pain and lumbopelvic pathologies.
Objectives
- Understand impairment-based classification of low back pain
- Demonstrate understanding of common Lumbopelvic pathologies
Pathology
- Pathology includes structural and functional deviations from the normal that constitute or characterize a disease.
- Pathology also covers the study of the essential nature of diseases and structural/functional changes they produce.
- Pathology does not always equal pain or limitation
Lumbar Clinical Practice Guideline
- Published in 2012 and updated in 2021
- Classifications for low back pain are impairment-based and not pathology based.
- Low back pain with mobility deficits are usually acute, subacute, or chronic.
- Low back pain with movement coordination impairments can be acute, subacute, or chronic.
- Low back pain with radiating pain can be acute, subacute, or chronic.
- Physical therapy diagnoses classifies low back pain
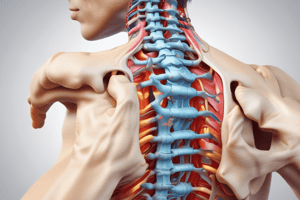
Overview of Pathology
- Serious/Systemic Pathology
- Bone Pathology
- Joint Pathology
- Disc Pathology
- Nerve Pathology
- Contractile Tissue Pathology
Serious/Systemic Pathology Overview
- Spondyloarthropathies
- including Ankylosing Spondylitis
- Cauda Equina
- Abdominal Aortic Aneurysm (AAA)
- Cancer
- Fracture
Ankylosing Spondylitis
- Ankylosing Spondylitis is an inflammatory condition of the spine that can result in spinal fusion.
- Onset is commonly in early adulthood (80% of cases occur in those <40 years old), and it is more prevalent in men than women.
- The incidence rate is 0.2-0.5%.
- Symptoms include SI joint and lumbar pain, pain with inactivity that improves with movement, uveitis, and Achilles enthesitis
- Diagnosis is aided by X-rays which show sacroiliitis, and blood tests which check for HLA-B27.
- Treatment includes medication (anti-inflammatories) and exercise for mobility and strengthening.
- There is not a known cure.
Cauda Equina Syndrome
- Cauda Equina Syndrome involves compression of the cauda equina
- Causes can include trauma, disc protrusion, hemorrhage, and tumors
- Incidence is 0.005 to 0.03% of back pain cases.
- Signs and symptoms include urinary retention/incontinence, "Saddle Anesthesia", and loss of anal sphincter tone.
- Cauda Equina Syndrome is considered a medical emergency that requires quick decompression to avoid permanent damage.
Abdominal Aortic Aneurysm (AAA)
- AAA involves dilation of the abdominal aorta greater then 3 cm (1.2 inches).
- Symptoms include abdominal pain and backache
- Risk factors include being an older male (4-8% prevalence) versus older women (0.5-1.5% prevalence), age, smoking, and family history.
- Diagnosis can be achieved through palpation and imaging (Ultrasound, CT, MRI)
Compression Fracture
- Compression fractures most frequently occur at T8, T12, L1, and L5
- Trauma is a cause and has a higher correlation when significant in younger persons and minor in order persons
- Risk Factors include being post-menopausal, osteoporosis, and long-term corticosteroid use.
- Symptoms include site pain and limited motion
- Diagnosed via X-Ray
- Treatment options are conservative and involve time, kyphoplasty, and fusion
Tumors
- Primary tumors are rare, originate in spine, osteosarcoma, and multiple myeloma.
- Secondary tumors are common and metastasize from another area, such as breast, lung, thyroid, kidney, and prostate.
- Red flags include unexplained weight loss, pain not relieved with rest or position change, and night pain.
Bone Pathologies Overview:
- Spondylolysis
- Spondylolisthesis
- Schmorl's Nodes
Spondylolysis
- Spondylolysis is a fracture of the pars interarticularis without vertebral displacement.
- Occurs due to repeated or excessive end-range extension
- Common in dancers and gymnasts
- Signs of Spondylolysis is pain which can present as either acute and/or chronic
- Localized to the low back.
- Diagnosis includes X-rays and the Scotty Dog Collar Sign
- Treatment is conservative and involves flexion bias, bracing, and time.
Spondylolisthesis
- Spondylolisthesis is a pars fracture with anterior displacement of the vertebral body.
- Low back pain as a result of movement coordination impairments usually in the lumbar region, especially L5/S1.
- Etiology: congenital, arthritis, trauma, and stress fracture.
- Diagnosis made via X-ray.
Meyerding Scale
- Used in order to measure displacement/slippage
- Grade 1 = 0 - 25%
- Grade 2 = 25 - 50%
- Grade 3 = 50 - 75%
- Grade 4 = 75 - 100%
- Spondyloptosis = >100%
- Symptoms include step-off deformity, neurological symptoms with higher grades, and pain.
- Treatment involves conservative therapy for low grades and injections.
- Surgery may be required for high grades.
Schmorl's Nodes
- Involves disc herniation through the vertebral endplate into the body of the vertebrae
- It is usually asymptomatic
Joint Pathology Overview:
- Low back pain with mobility deficits according to CPG.
- Degenerative Joint Disease (DJD) Facet arthropathy, Spondylosis, and Osteoarthritis (OA) are all different words for the same thing.
- Genetic and lifestyle factors, and trauma all contribute towards joint pathologies/conditions.
- Arthritic changes includes Osteophytes, Cartilage loss, and Thickening of the capsule
Facet Joint Signs/Symptoms
- Pain stiffness can be relieved with movement.
- ROM is limited.
- Closed positions are often the most uncomfortable such as standing and walking.
- The population most affected tend to be older.
- Conservative care is one treatment alongside mobility work and manual therapy. Another treatment pathway is injections, and radiofrequency ablation.
SI Joint
- Usually related to hypermobility.
- More pertinent in Peripartum women vs men.
- Hypermobile people
- Connective tissue disorders
- CPG: with low back pain with movement coordination impairments
- Symptoms include stiff, sharp, tingling, pain that's localized and/or generalized, sitting inactivity, shifting weight to affected side, or lifting & running.
- Treatments include conservative care with bracing work and manual therapy. Strengthening, injections, RFA, or surgery is also common.
Disc Pathology Overview
- Estimated prevalence of pain related to disc herniation is 1.6-13.4% (Wong et al 2023).
- DDD involves 88-96% in patients 60-80 y/o that have disc degeneration.
- Numbers increase every decade of life starting at age 20.
- Disc herniation: 69-84% of asymptomatic patients between 60-80 y/o are said to bulge the disk.
Degenerative Disc Disease (DDD)
- Decrease in proteoglycans decreases water imbibition into nucleus
- Decreased vertical height
- Increased facet joint loading
- Ligamentous laxity: bulging into spinal canal causing stenosis
- Loss of nutrients, strong genetic link, and lifestyle factors all lead to DDD.
Disc Herniation
- Posterolateral is most common
- Degeneration causes breakdown of inner rings and no outer ring deformation
- Prolapse causes bulging with normal annular margin and outer rings intact
- Extrusion is nuclear material escapes but is still one piece. Portions typically extrude out of broken annulus.
- Finally, during sequestration the nuclear material breaks free from disc causing the annular material to break free.
- Low back pain with radiating pain and related signs/symptoms. Back and radiating pain causes +/- neurological signs which include (Bend/twist > standing/walking with nerve mechanosensitivity.)
- Treatment pathway is to start with time and directional, and if that fails use treatment such as Surgery.
Can disc herniations heal without surgery?
- YES
Nerve Pathology Overview
- CPG - Low back pain with radiating pain
- Radiculopathy
- Stenosis
- Nerve Entrapment
- Nerve Mechanosensitivity
- "Double Crush" Syndrome
Radiculopathy
- Prevalence rate is 3-5%, with age a major risk factor.
- Men: 40s
- Women: 50-60s
- Includes degenerative spondyloarthropathies, disc herniation, and spondylolisthesis as factors.
- True neurological deficits are present.
Signs/Symptoms
- Pain: dermatomes, myotomes & reflexes.
- Pain associated with the nerve root.
- Decreased ROM nerve mechanosensitivity.
- Treatment: Conservative, injection & surgery
Central Stenosis
- Stenosis includes narrowing of a canal or tube.
- Narrowing of spinal cord space
- "Buckling"/thickening of PLL & ligamentum flavum.
- Symptoms
- Bilateral LE symptoms, +/- true neurological signs, neurogenic claudication & upper motor neuron deficits.
- Treatment: conservative care and direction specific treatments, combined with injections and/or surgery.
Foraminal Stenosis
- Narrowing of foramen
- Facet hypertrophy
- Disc pathology
- Unilateral symptoms are common.
- Additional symptoms include neurogenic Claudication, Lower Motor Neuron deficits and +/- true neurological signs.
- Treatment encompasses direction-specific conservative care, injections, and surgery.
Nerve Entrapment
- Theory: Minor injury to nerve, connective tissue causes:
- Adherence/ "tethering"
- Shortening.
- Loss of Elasticity
- Results in pain, paresthesia along affected nerve.
Often, nerves are sensitized to pressure (stretch, compression) and prevalence varies based on body area.
Symptoms include pain and paresthesia along nerve, or deficits to the motor system. - Be wary of "Double Crush"
- Compression and irritation of nerves along two distinct areas.
Nerve Treatment
- Nerves require space, movement, cardiovascular to thrive.
Contractile Pathology
- CPG - Low back pain with mobility deficits can be overlooked here as a pain generator. Muscle strain is typically the result of acute or chronic overuse leading to myofascial pain. Similarly, muscle spasm is a potential contributor to protective mechanisms in the spine by causing a contractile or nerve-injury response within a joint or disc. Treatment and management may vary.
- Symptoms may manifest as sharp pain within/around lumbar musculature accompanied by limited ROM upon assessment. Treatment typically takes different forms - ranging anywhere from time, conservative care of joint systems, and therapeutic trigger point injections (amongst other things).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.