Podcast
Questions and Answers
What primarily differentiates lentigo from freckles?
What primarily differentiates lentigo from freckles?
- Lentigo shows no change in color with sun exposure. (correct)
- Freckles are a type of benign neoplasm.
- Lentigo is affected by UV exposure.
- Freckles have an increased number of melanocytes.
Which feature is characteristic of dysplastic nevi compared to regular melanocytic nevi?
Which feature is characteristic of dysplastic nevi compared to regular melanocytic nevi?
- Presence of atypical features suggesting malignancy. (correct)
- Increased number of normal melanocytes.
- Greater uniformity in shape.
- Higher likelihood of being uniformly colored.
What describes the morphology of freckles?
What describes the morphology of freckles?
- Dark raised lesions with irregular borders.
- Small brown/dark macules that can darken with sun exposure. (correct)
- Uniform smooth texture with scaling.
- Benign pigmented lesions with increased melanocyte density.
What is a key microscopic feature that helps differentiate lentigo from melanoma?
What is a key microscopic feature that helps differentiate lentigo from melanoma?
What genetic alterations are associated with an increased risk of developing melanoma in dysplastic nevi?
What genetic alterations are associated with an increased risk of developing melanoma in dysplastic nevi?
What is the most common location for squamous cell carcinoma to develop?
What is the most common location for squamous cell carcinoma to develop?
Which of the following is a classic pathological finding associated with squamous cell carcinoma?
Which of the following is a classic pathological finding associated with squamous cell carcinoma?
Which risk factor is NOT associated with the development of squamous cell carcinoma?
Which risk factor is NOT associated with the development of squamous cell carcinoma?
What effect does chronic immunosuppression have in relation to squamous cell carcinoma?
What effect does chronic immunosuppression have in relation to squamous cell carcinoma?
What distinguishes basal cell carcinoma from squamous cell carcinoma?
What distinguishes basal cell carcinoma from squamous cell carcinoma?
What is the primary cause of actinic keratosis?
What is the primary cause of actinic keratosis?
Which of the following is a characteristic feature of inclusion cysts?
Which of the following is a characteristic feature of inclusion cysts?
What is the relationship between adnexal tumors and sweat glands?
What is the relationship between adnexal tumors and sweat glands?
Which of the following features is associated with actinic keratosis?
Which of the following features is associated with actinic keratosis?
What is a common consequence of torsion in polyps?
What is a common consequence of torsion in polyps?
Which subtype of melanoma is the most common?
Which subtype of melanoma is the most common?
What is a key characteristic of nodular melanoma compared to other types?
What is a key characteristic of nodular melanoma compared to other types?
Which of the following describes the ABCDE criteria for melanoma detection?
Which of the following describes the ABCDE criteria for melanoma detection?
What is one of the typical appearances of acral lentiginous melanoma?
What is one of the typical appearances of acral lentiginous melanoma?
Which type of melanoma is often referred to as melanoma in situ?
Which type of melanoma is often referred to as melanoma in situ?
Acanthosis nigricans is most commonly associated with which condition?
Acanthosis nigricans is most commonly associated with which condition?
Which of the following is a common location for fibroepithelial polyps?
Which of the following is a common location for fibroepithelial polyps?
The Leser-Trélat sign is associated with which skin condition?
The Leser-Trélat sign is associated with which skin condition?
Flashcards
Freckles definition
Freckles definition
Small, flat, brown spots caused by increased melanin, not affecting melanocyte numbers.
Lentigo definition
Lentigo definition
Benign spots with increased melanocytes; not sun-sensitive like freckles.
Melanocytic nevi
Melanocytic nevi
Benign growth of melanocytes, often round or oval, uniform color.
Dysplastic nevi
Dysplastic nevi
Signup and view all the flashcards
Skin cancer risk and Dysplastic nevi
Skin cancer risk and Dysplastic nevi
Signup and view all the flashcards
Inclusion cyst definition
Inclusion cyst definition
Signup and view all the flashcards
Actinic keratosis cause
Actinic keratosis cause
Signup and view all the flashcards
Actinic keratosis morphology
Actinic keratosis morphology
Signup and view all the flashcards
Fibrovascular polyp cause
Fibrovascular polyp cause
Signup and view all the flashcards
Adnexal tumor characteristics
Adnexal tumor characteristics
Signup and view all the flashcards
Squamous Cell Carcinoma (SCC)
Squamous Cell Carcinoma (SCC)
Signup and view all the flashcards
SCC Risk Factors
SCC Risk Factors
Signup and view all the flashcards
SCC Appearance
SCC Appearance
Signup and view all the flashcards
Basal Cell Carcinoma (BCC)
Basal Cell Carcinoma (BCC)
Signup and view all the flashcards
BCC Key Point
BCC Key Point
Signup and view all the flashcards
Melanoma
Melanoma
Signup and view all the flashcards
ABCDE (Melanoma)
ABCDE (Melanoma)
Signup and view all the flashcards
Superficial Spreading Melanoma
Superficial Spreading Melanoma
Signup and view all the flashcards
Nodular Melanoma
Nodular Melanoma
Signup and view all the flashcards
Lentigo Maligna Melanoma
Lentigo Maligna Melanoma
Signup and view all the flashcards
Acanthosis Nigricans
Acanthosis Nigricans
Signup and view all the flashcards
Fibroepithelial Polyp
Fibroepithelial Polyp
Signup and view all the flashcards
Leser-Trelat Sign
Leser-Trelat Sign
Signup and view all the flashcards
Study Notes
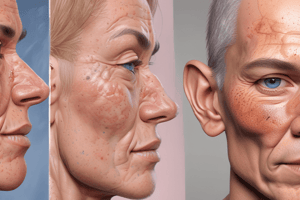
Disorders of Hyperpigmentation (1/2)
-
Freckles: Small brown/dark macules (flat). Darken in sun exposure. Increased melanin. Normal melanocyte number/density.
-
Lentigo: Benign pigmented lesion. Increased number of melanocytes in the basal layer of epidermis. Not affected by UV/sun exposure. Morphology: small, flat, uniform brown, tan or black coloration. Smooth with no scaling or thickening. Commonly on sun-exposed areas (face, hands, forearms). Increased melanocytes at dermal-epidermal junction. No nesting or clustering of melanocytes (distinguishes from melanoma). Hyperpigmentation due to increased melanin production.
-
Melanocytic Nevi: Benign neoplasm of melanocytes. Tan/brown pigmented lesions. Uniform color. Often round or oval shape.
Disorders of Hyperpigmentation (2/2)
-
Hemosiderin Hyperpigmentation: Brownish skin discoloration. Caused by deposition of hemosiderin (breakdown of hemoglobin). Induration, scaling or atrophy in chronic cases. Occurs in lower extremities (ankles and shins). Symmetrical involvement is common. Secondary to chronic venous insufficiency (CVI). Extravasation of RBCs into the dermis. Macrophages phagocytose hemosiderin. Diagnosis: Clinical based on pigmentation associated with CVI or trauma. Dermoscopy: Hemosiderin deposition. Benign. Indicates underlying venous pathology. Chronic may lead to permanent discoloration or venous ulcers.
-
Post-Inflammatory Hyperpigmentation (PIH): Acquired hyperpigmentation after skin injury or inflammation. Abnormal distribution of melanin in epidermis or dermis (skin's inflammatory response). Morphology: Hyperpigmented macules or patches with irregular borders. Color ranges: light brown-black (epidermal)or blue-gray (dermal). Epidermal PIH: Fades over months to years. Dermal PIH: More persistent and harder to treat.
Disorders of Hypo-pigmentation
-
Albinism (Oculocutaneous Albinism (OCA)): Family of genetic disorders. Autosomal recessive. Absent/reduced melanin synthesis in melanocytes. Normal number of melanocytes. Most common forms: decrease tyrosinase activity. Hypopigmentation of hair, skin, eyes. White hair, pink skin color, blue eyes. Increased risk of sunburns, Increased risk of skin cancer, No UV light protection.
-
Vitiligo: Acquired, localized pigment disorder. Autoimmune destruction of melanocytes.
-
Idiopathic Hypomelanosis (IGH): Benign condition. Asymptomatic depigmented (white) macules/patches. No clinical signs of inflammation (warmth). Treatment: steroids, immunosuppressants. Dark skinned individuals: Obvious areas of depigmentation. Light skinned individuals: Failure to tan in localized region.
Other Disorders of Skin Pigmentation
- Multiple small, round or oval, hypopigmented macules. Seen in middle-aged and older adults. Results from chronic sun exposure and aging.
- Affects sun-exposed areas of skin. Hypopigmented macules (lighter than surrounding skin). Smooth surface with no scaling or atrophy.
Benign Epithelial Tumors
-
Seborrheic Keratosis: Common benign tumors. Proliferation of immature keratinocytes. Arise spontaneously. Commonly on the trunk. Flat, well-demarcated, round or oval. Dark, velvety surface, appear "stuck on."
-
Acanthosis Nigricans: Hyperpigmented (dark) plaques on skin. Intertriginous sites (folds). Associated with insulin resistance. Often seen in obesity, diabetes. Rarely associated with malignancy.
Other Skin Tumors
- Pityriasis Alba: Common, benign, self-limiting skin condition characterized by hypopigmented, scaly patches primarily in children and adolescents. Often in the face (cheeks) and neck, arms, and trunk. Form of atopic dermatitis associated with xerosis (dry skin. Hypopigmented light colored patches. Initially pink or red, fading to pale white over time. Fine scaling. Round, oval irregular shape (0.5-2cm). Lesions persist weeks to months, gradual repigmentation. Associated with atopic dermatitis and xerosis. Increased transepidermal water loss, dryness, and mild inflammation.
Premalignant and Malignant Epidermal Tumors
-
Actinic Keratosis: Premalignant skin lesions, caused by sun exposure. Growth of atypical epidermal keratinocytes; can lead to squamous cell carcinoma. Round, red/brown papules or plaques. Sun-exposed areas.
-
Squamous Cell Carcinoma (SCC): 2nd most common skin cancer. Arises from squamous cells in the epidermis. Occurs in sun-exposed areas (face, lips, ears, hands). DNA damage by UV light. Common in older adults (>75). Less than 5% metastasize to regional nodes. Rarely metastasize beyond nodes. Red, scaling plaques with sharp borders. More advanced lesions: ulcerate, keratin production. May crust or bleed. Risk factors: Sun exposure. Chronic immunosuppression. Organ transplants, HIV, long-term glucocorticoids. Chronic skin inflammation. Burns, chronic ulcers, and draining sinus tracts. Arsenic exposure.
-
Basal Cell Carcinoma (BCC): Most common skin cancer. Slow growing. Rarely metastasizes. Most are found early and excised. Occur in sun-exposed areas. Lowest potential for recurrence or metastases. Pearly papules or nodules. May have telangiectasia on surface.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.