Podcast
Questions and Answers
Which characteristic is NOT a clinical sign of gingivitis?
Which characteristic is NOT a clinical sign of gingivitis?
Which systemic factor is known to exacerbate plaque-induced gingivitis?
Which systemic factor is known to exacerbate plaque-induced gingivitis?
What is the primary cause of plaque-induced gingivitis?
What is the primary cause of plaque-induced gingivitis?
Which of the following symptoms is NOT typically reported by patients with gingivitis?
Which of the following symptoms is NOT typically reported by patients with gingivitis?
Signup and view all the answers
How is gingivitis primarily diagnosed?
How is gingivitis primarily diagnosed?
Signup and view all the answers
Which factor may lead to an increased accumulation of dental plaque in individuals with gingivitis?
Which factor may lead to an increased accumulation of dental plaque in individuals with gingivitis?
Signup and view all the answers
In the context of gingivitis, what differentiates generalized gingivitis from localized gingivitis?
In the context of gingivitis, what differentiates generalized gingivitis from localized gingivitis?
Signup and view all the answers
What is one of the significant factors that can lead to the reversibility of gingivitis?
What is one of the significant factors that can lead to the reversibility of gingivitis?
Signup and view all the answers
Which of the following is a clinical sign of gingival inflammation?
Which of the following is a clinical sign of gingival inflammation?
Signup and view all the answers
Which classification describes conditions that are not caused by dental plaque?
Which classification describes conditions that are not caused by dental plaque?
Signup and view all the answers
What is the effect of reducing dental plaque on gingival lesions?
What is the effect of reducing dental plaque on gingival lesions?
Signup and view all the answers
Which of the following is NOT a risk factor for gingival lesions?
Which of the following is NOT a risk factor for gingival lesions?
Signup and view all the answers
Which type of gingivitis is characterized by inflammation independent of plaque?
Which type of gingivitis is characterized by inflammation independent of plaque?
Signup and view all the answers
Which of the following is a characteristic of autoimmune diseases affecting gingival tissue?
Which of the following is a characteristic of autoimmune diseases affecting gingival tissue?
Signup and view all the answers
Which of these lesions is classified as a neoplasm associated with gingival tissue?
Which of these lesions is classified as a neoplasm associated with gingival tissue?
Signup and view all the answers
What is a common misconception regarding gingival pigmentation?
What is a common misconception regarding gingival pigmentation?
Signup and view all the answers
Which type of gingival condition is primarily associated with hereditary factors?
Which type of gingival condition is primarily associated with hereditary factors?
Signup and view all the answers
What type of viral infection is primarily characterized by multiple vesicles that rupture to form painful ulcers on the gingiva?
What type of viral infection is primarily characterized by multiple vesicles that rupture to form painful ulcers on the gingiva?
Signup and view all the answers
Which condition could potentially lead to linear gingival erythema in immunocompromised patients?
Which condition could potentially lead to linear gingival erythema in immunocompromised patients?
Signup and view all the answers
Which of the following is NOT a recognized bacterial origin of gingival lesions?
Which of the following is NOT a recognized bacterial origin of gingival lesions?
Signup and view all the answers
What is a notable feature of contact allergy-related gingival lesions?
What is a notable feature of contact allergy-related gingival lesions?
Signup and view all the answers
Which type of hypersensitivity reaction may present lesions resembling oral lichen planus or leukoplakia?
Which type of hypersensitivity reaction may present lesions resembling oral lichen planus or leukoplakia?
Signup and view all the answers
What distinguishes localized gingivitis from generalized gingivitis?
What distinguishes localized gingivitis from generalized gingivitis?
Signup and view all the answers
Which organism is primarily responsible for generalized gingival candidiasis?
Which organism is primarily responsible for generalized gingival candidiasis?
Signup and view all the answers
Study Notes
Attempts at Classification
- Classification of disease is essential for distinct categories to aid clinical and lab diagnosis, and specific treatment.
- Ideally, criteria should be based on etiology, histopathology, and genetics, rather than age of onset or disease progression rates.
- Over the past three decades, there have been four major attempts to classify periodontal disease.
- The 1999 classification of periodontitis was reclassified in 1999 and used for 19 years.
- Reclassified into chronic, aggressive (local and generalized), necrotizing, and as a systemic disease manifestation.
- A 2017 workshop established a classification framework for periodontitis.
- This framework includes a multidimensional staging and grading system that can adapt to new information.
Classification of Periodontal Diseases and Conditions (2017)
-
1. Periodontal health and gingival diseases and conditions:
- a. Periodontal health and gingival health
- b. Dental biofilm-induced gingivitis
- c. Non-dental biofilm-induced gingival disease
-
2. Periodontitis:
- a. Periodontitis
- b. Necrotizing periodontal diseases
- c. Periodontitis as a manifestation of systemic disease
-
3. Other conditions affecting the periodontium:
- a. Periodontal abscess and endodontic periodontal lesions
- b. Mucogingival deformity and conditions
- c. Traumatic occlusal force
- d. Tooth and prosthetic-related factors
- e. Peri-implant disease and conditions
- a. Peri-implant health
- b. Peri-implant mucositis
- c. Peri-implantitis
- d. Peri-implant soft and hard tissue deficiency
Periodontal Health and Gingival Health
- Defined by the absence of clinically detectable inflammation.
- There is a biological level of immune surveillance consistent with clinical gingival health and homeostasis.
- Clinical gingival health can be assessed using a bleeding-on-probing score (BOP%).
- Clinical gingival health on an intact periodontium is characterized by the absence of bleeding on probing (less than 10%), lack of symptoms, and attachment and bone loss ≤3mm probing pocket depth.
- Clinical gingival health on a reduced periodontium includes non-periodontitis patients with recession due to any cause except periodontitis. Characterized by the absence of bleeding on probing (less than 10%), and possible reduced clinical attachment and bone levels with probing pocket depth ≤3mm.
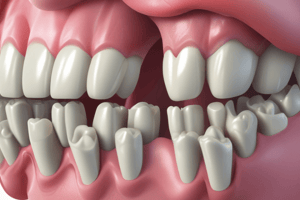
Dental Biofilm-Induced Gingivitis
- Defined at the site level as an inflammatory lesion resulting from interactions between dental plaque biofilm and the host's inflammatory response,
- Contained within the gingiva, does not extend to periodontal attachment.
- Reversible by reducing dental plaque at and apical to the gingival margin.
- Localized gingivitis = BOP score 10% to ≤30%
- Generalized gingivitis = BOP score >30%
- Gingivitis on an intact periodontium characterized by BOP score ≥10%, probing pocket depth ≤3mm, no pseudo pocket, no attachment loss, and no radiographic bone loss.
- Gingivitis on a reduced periodontium is in a non-periodontitis patient characterized by BOP score ≥10%, probing pocket depth ≤3mm, possible presence of attachment loss and/or radiographic bone loss.
Classification of Dental Biofilm-Induced Gingivitis
- A. Associated with bacterial dental biofilm only
-
B. Mediated by systemic or local risk factors
-
- Systemic conditions
- a. Sex steroid hormones
- b. Hyperglycemia
- c. Leukemia
- d. Smoking
- e. Malnutrition
-
- Oral factors enhancing plaque accumulation
- a. Prominent subgingival restoration margins
- b. Hyposalivation
-
- C. Drug-influenced gingival enlargements
Dental Plaque-Induced Gingivitis, Associated with Specific Infections
- Genetic/developmental disorders (Hereditary gingival fibromatosis)
- Bacterial infections ( Neisseria gonorrhoeae, Treponema pallidum, Streptococcal species , others)
- Viral infections (Herpes simplex, Varicella-zoster, Epstein-Barr)
Inflammatory and Immune Conditions Gingiva (Hypersensitivity)
- Contact allergy
- Plasma cell gingivitis:
- Erythema multiforme
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the key classifications of periodontal diseases established in 2017. Understanding the criteria used, such as etiology and histopathology, is essential for clinicians and researchers. This quiz covers the multidimensional staging and grading systems for periodontal health and diseases.