Podcast
Questions and Answers
What is the most common site for cellulitis to occur?
What is the most common site for cellulitis to occur?
Which of the following is NOT a predisposing factor for cellulitis?
Which of the following is NOT a predisposing factor for cellulitis?
Which treatment is often prescribed in addition to antibiotics for cellulitis?
Which treatment is often prescribed in addition to antibiotics for cellulitis?
What condition can resemble cellulitis and requires leg ultrasound for investigation?
What condition can resemble cellulitis and requires leg ultrasound for investigation?
Signup and view all the answers
Which of the following types of bacteria is most commonly involved in the development of cellulitis?
Which of the following types of bacteria is most commonly involved in the development of cellulitis?
Signup and view all the answers
Which of the following best describes erysipelas?
Which of the following best describes erysipelas?
Signup and view all the answers
What is the significance of pain relief in the treatment of cellulitis?
What is the significance of pain relief in the treatment of cellulitis?
Signup and view all the answers
Which of the following could increase a person's risk of developing cellulitis?
Which of the following could increase a person's risk of developing cellulitis?
Signup and view all the answers
What is the primary reason for administering high doses of intravenous antibiotics in necrotizing infections?
What is the primary reason for administering high doses of intravenous antibiotics in necrotizing infections?
Signup and view all the answers
Which combination of antibiotics would be appropriate for a patient with a penicillin allergy suffering from a necrotizing infection?
Which combination of antibiotics would be appropriate for a patient with a penicillin allergy suffering from a necrotizing infection?
Signup and view all the answers
In the prognosis of necrotizing soft tissue infections, which group category indicates the highest mortality risk based on admission variables?
In the prognosis of necrotizing soft tissue infections, which group category indicates the highest mortality risk based on admission variables?
Signup and view all the answers
Which of the following factors does NOT contribute to the scoring for mortality risk according to the admission variables?
Which of the following factors does NOT contribute to the scoring for mortality risk according to the admission variables?
Signup and view all the answers
When considering empirical therapy for necrotizing infections, which antibiotic should always accompany a broad-spectrum beta-lactam?
When considering empirical therapy for necrotizing infections, which antibiotic should always accompany a broad-spectrum beta-lactam?
Signup and view all the answers
What is a characteristic feature that differentiates erysipelas from cellulitis?
What is a characteristic feature that differentiates erysipelas from cellulitis?
Signup and view all the answers
What type of infection is caused by the synergistic action of streptococci and staphylococci?
What type of infection is caused by the synergistic action of streptococci and staphylococci?
Signup and view all the answers
Which statement is true regarding the treatment of synergistic gangrene?
Which statement is true regarding the treatment of synergistic gangrene?
Signup and view all the answers
What is a common clinical finding associated with gas gangrene?
What is a common clinical finding associated with gas gangrene?
Signup and view all the answers
What is one of the key characteristic symptoms of gas gangrene?
What is one of the key characteristic symptoms of gas gangrene?
Signup and view all the answers
What is a critical factor that can increase the mortality rate of gas gangrene?
What is a critical factor that can increase the mortality rate of gas gangrene?
Signup and view all the answers
Which preventive measure is critical after the resolution of an initial infection?
Which preventive measure is critical after the resolution of an initial infection?
Signup and view all the answers
Which of the following describes gas gangrene's bacterial involvement?
Which of the following describes gas gangrene's bacterial involvement?
Signup and view all the answers
What typical areas of the body are most commonly affected by erysipelas?
What typical areas of the body are most commonly affected by erysipelas?
Signup and view all the answers
Which of the following organisms is primarily responsible for most cases of erysipelas?
Which of the following organisms is primarily responsible for most cases of erysipelas?
Signup and view all the answers
What is a distinguishing feature of erysipelas compared to cellulitis?
What is a distinguishing feature of erysipelas compared to cellulitis?
Signup and view all the answers
Which symptom is considered a constitutional symptom of erysipelas?
Which symptom is considered a constitutional symptom of erysipelas?
Signup and view all the answers
What is a common complication of untreated erysipelas?
What is a common complication of untreated erysipelas?
Signup and view all the answers
Which antibiotic is generally preferred for treating erysipelas?
Which antibiotic is generally preferred for treating erysipelas?
Signup and view all the answers
What occurs approximately 10 days after the onset of erysipelas?
What occurs approximately 10 days after the onset of erysipelas?
Signup and view all the answers
What may happen if erysipelas recurs after antibiotic treatment?
What may happen if erysipelas recurs after antibiotic treatment?
Signup and view all the answers
What is the main reason for the immediate removal of muscle groups in gas gangrene?
What is the main reason for the immediate removal of muscle groups in gas gangrene?
Signup and view all the answers
What is the typical mortality rate for untreated gas gangrene?
What is the typical mortality rate for untreated gas gangrene?
Signup and view all the answers
Which of the following is a common symptom of necrotizing fasciitis?
Which of the following is a common symptom of necrotizing fasciitis?
Signup and view all the answers
What treatment is typically required after excision of the affected area in necrotizing fasciitis?
What treatment is typically required after excision of the affected area in necrotizing fasciitis?
Signup and view all the answers
What agents are primarily responsible for necrotizing fasciitis?
What agents are primarily responsible for necrotizing fasciitis?
Signup and view all the answers
What can hyperbaric oxygen treatments potentially reduce in cases of gas gangrene?
What can hyperbaric oxygen treatments potentially reduce in cases of gas gangrene?
Signup and view all the answers
How quickly can symptoms of necrotizing fasciitis manifest after infection occurs?
How quickly can symptoms of necrotizing fasciitis manifest after infection occurs?
Signup and view all the answers
What is a characteristic feature of the tissue destruction caused by necrotizing fasciitis?
What is a characteristic feature of the tissue destruction caused by necrotizing fasciitis?
Signup and view all the answers
Flashcards
What is cellulitis?
What is cellulitis?
Inflammation of the deeper layers of skin, often affecting the face or lower legs. It's caused by bacteria like Group A streptococcus, which enter through skin cracks or breaks.
What are predisposing factors for cellulitis?
What are predisposing factors for cellulitis?
Factors that increase the risk of developing cellulitis, for example, skin cracks, cuts, burns, insect bites, or weak immune systems.
How is cellulitis diagnosed?
How is cellulitis diagnosed?
Cellulitis is often diagnosed based on symptoms and appearance. Swabs may not always show the specific bacteria. Blood cultures are usually positive only if there is sepsis.
How is cellulitis treated?
How is cellulitis treated?
Signup and view all the flashcards
What is Erysipelas?
What is Erysipelas?
Signup and view all the flashcards
Who is at risk for Erysipelas?
Who is at risk for Erysipelas?
Signup and view all the flashcards
What makes Erysipelas and Cellulitis hard to tell apart?
What makes Erysipelas and Cellulitis hard to tell apart?
Signup and view all the flashcards
What is Necrotizing Fasciitis?
What is Necrotizing Fasciitis?
Signup and view all the flashcards
Erysipelas
Erysipelas
Signup and view all the flashcards
Necrotizing Fasciitis
Necrotizing Fasciitis
Signup and view all the flashcards
Constitutional Symptoms of Erysipelas
Constitutional Symptoms of Erysipelas
Signup and view all the flashcards
Characteristic Appearance of Erysipelas
Characteristic Appearance of Erysipelas
Signup and view all the flashcards
Treatment for Erysipelas
Treatment for Erysipelas
Signup and view all the flashcards
Recurrent Erysipelas
Recurrent Erysipelas
Signup and view all the flashcards
Common Areas Affected by Erysipelas
Common Areas Affected by Erysipelas
Signup and view all the flashcards
Distinguishing Erysipelas from Cellulitis
Distinguishing Erysipelas from Cellulitis
Signup and view all the flashcards
What is synergistic gangrene?
What is synergistic gangrene?
Signup and view all the flashcards
What causes Gas gangrene?
What causes Gas gangrene?
Signup and view all the flashcards
What is Gas gangrene?
What is Gas gangrene?
Signup and view all the flashcards
How does Gas gangrene affect the muscle?
How does Gas gangrene affect the muscle?
Signup and view all the flashcards
How is Gas gangrene diagnosed?
How is Gas gangrene diagnosed?
Signup and view all the flashcards
Why are prophylactic antibiotics sometimes used?
Why are prophylactic antibiotics sometimes used?
Signup and view all the flashcards
Why are combination antibiotics important in Necrotizing Fasciitis?
Why are combination antibiotics important in Necrotizing Fasciitis?
Signup and view all the flashcards
What types of antibiotics are often used for Necrotizing Fasciitis?
What types of antibiotics are often used for Necrotizing Fasciitis?
Signup and view all the flashcards
What's the mortality rate of Necrotizing Fasciitis if left untreated?
What's the mortality rate of Necrotizing Fasciitis if left untreated?
Signup and view all the flashcards
How can we predict the outcome of Necrotizing Fasciitis?
How can we predict the outcome of Necrotizing Fasciitis?
Signup and view all the flashcards
What bacteria are involved in Necrotizing Fasciitis?
What bacteria are involved in Necrotizing Fasciitis?
Signup and view all the flashcards
What tissue does Necrotizing Fasciitis affect?
What tissue does Necrotizing Fasciitis affect?
Signup and view all the flashcards
What is a major symptom of Necrotizing Fasciitis?
What is a major symptom of Necrotizing Fasciitis?
Signup and view all the flashcards
How is Necrotizing Fasciitis treated?
How is Necrotizing Fasciitis treated?
Signup and view all the flashcards
When is amputation a possible treatment for Necrotizing Fasciitis?
When is amputation a possible treatment for Necrotizing Fasciitis?
Signup and view all the flashcards
What is a supplementary treatment for Necrotizing Fasciitis?
What is a supplementary treatment for Necrotizing Fasciitis?
Signup and view all the flashcards
What is the prognosis for Necrotizing Fasciitis?
What is the prognosis for Necrotizing Fasciitis?
Signup and view all the flashcards
Study Notes
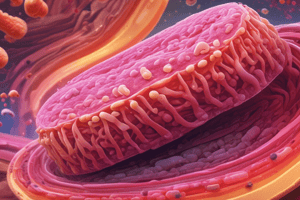
Skin and Soft-Tissue Infections
- Cellulitis is a diffuse inflammation of connective tissue (dermal and subcutaneous layers)
- Commonly affects skin on the face or lower legs
- Caused by normal skin flora or exogenous bacteria (e.g., Group A streptococci)
- Bacteria easily breach defensive barriers due to toxins
- Lymphatic system is involved
Predisposing Factors
- Cracks in skin (dry skin, eczema, tattoos)
- Cuts and blisters
- Burns
- Insect bites
- Animal bites
- Surgical wounds
- Intravenous catheter insertion sites
- Injecting drug use
- Pregnancy, diabetes, obesity, chronic venous insufficiency, and varicose veins (affect circulation)
- Breaks in the skin do not need to be visible
Diagnosis
- Often a clinical diagnosis
- Local cultures may not identify the causative organism
- Blood cultures are positive only if generalized sepsis develops
- Conditions that mimic cellulitis include deep vein thrombosis, stasis dermatitis, and Lyme disease
Treatment
- Rest the affected limb/area
- Clean the wound (with debridement of dead tissue if needed)
- Oral antibiotics, but in severe cases, IV antibiotics are used
- Example antibiotics: Flucloxacillin, benzylpenicillin, ampicillin/amoxicillin
- Pain relief is important, but excessive pain may indicate necrotizing fasciitis (requires emergency surgery)
- Hyperbaric oxygen therapy can be helpful but not widely available
Erysipelas
- An acute streptococcal infection of the superficial dermis (upper subcutaneous dermis)
- Results in inflammation
- Has a well-defined edge
- Often coexists with cellulitis, making differentiation difficult
- Commonly affects the face, arms, fingers, legs, and toes.
- Older people, infants, children are at increased risk
- Risk factors include compromised immune systems, diabetes, alcoholism, skin ulceration, fungal infections, impaired lymphatic drainage (e.g., after mastectomy, pelvic surgery).
Signs and Symptoms Erysipelas
- Constitutional symptoms (high fevers, chills, fatigue, headaches, vomiting)
- Rapidly enlarging, erythematous (red) skin lesion
- Sharply demarcated, raised edge
- Warm, hardened, painful rash
- Rash similar in consistency to an orange peel
- More severe cases may result in vesicles, bullae, and petechiae, with possible skin necrosis
- Lymph nodes may be swollen or lymphedema may occur
- Fat tissue is particularly susceptible to infection
Etiology Erysipelas
- Most cases are due to Streptococcus pyogenes (beta-hemolytic group A streptococci)
Diagnosis Erysipelas
- Appearance of well-demarcated rash and inflammation
- Blood cultures are unreliable
- Distinguished from cellulitis by raised advancing edges and sharp borders
- Elevation of antistreptolysin O titre around 10 days after illness
Complications
- Spread to other body areas (bacteremia), including septic arthritis and infective endocarditis (heart valves)
- Septic shock
- Recurrence (18-30% even after antibiotic treatment)
- Lymphatic damage
- Necrotizing fasciitis (a potentially deadly exacerbation)
- Death
Treatment (Erysipelas)
- Oral or preferably intravenous antibiotics
- Penicillin
- Clindamycin
- Erythromycin
- Cephalosporins
- Symptoms usually resolve in a day or two; skin may take weeks to return to normal
Prevention
- Clean and appropriately dress wounds
- Change bandages daily
- Remove retained foreign bodies
Necrotizing Infections
-
Synergistic gangrene: Chronic, progressive bacterial gangrene caused by the synergistic action of streptococci and staphylococci
- Incubation period: 7-14 days
- Cellulitis progression with gangrenous ulceration
- Treatment: Radical excision of the ulcerated lesion and large systemic doses of penicillin
-
Gas gangrene: Anaerobic infection of muscle by Clostridium perfringens, producing toxins that destroy tissue and blood cells
- Disrupts and fragments normal muscle ,causes hemorrhage and edema, progresses to a purplish black
- Fluid discharge is commonly present and is brownish and malodorous
- Often affected areas initially are mottled (ecchymotic) and progress to blackening, and sloughing
- Diagnosis based on typical clinical findings in wound fluid, presence of large Gram-positive rods
- Delays in diagnosis, greatly increase the mortality
- Immediate removal of involved muscle groups may be necessary, with potential amputation
- High intravenous doses of penicillin and whole blood, possibly multiple hyperbaric oxygen treatments.
-
Necrotizing fasciitis: Serious mixed infection of hemolytic streptococci/staphylococci and peptostreptococci, producing toxins that destroy connective tissue
- Characterized by intense pain, rapid swelling, discoloration, blisters, necrosis, diarrhea, vomiting, high fever.
- Infection originates at operative wounds, lacerations, abrasions, or punctures.
- It may be immediately fulminant or dormant for several days before rapidly spreading
-
Aggressive surgical debridement and large intravenous doses antibiotics (including penicillin, vancomycin, and clindamycin)
- Possible amputation, intensive treatment, high fatality rate untreated.
Management of Necrotizing Infections
- IV antibiotics in high doses, to quickly reach bactericidal concentrations.
- Empirical therapy must comprehensively cover all possible pathogens (aerobes and anaerobes) and must be supplementary to surgical procedures.
Empirical therapy
- Broad-spectrum penicillin (amoxicillin) + metronidazole + aminoglycoside (gentamicin)
- Second-generation cephalosporin (cefuroxime) + metronidazole
- Penicillin allergy: clindamycin + quinolone (e.g., ciprofloxacin)
- Immunocompromised patients, require quinolones for possible Pseudomonas infections.
Prognosis (Mortality) - Necrotizing Soft Tissue Infections
- Clinical score on admission can predict mortality.
- High heart rate, low body temperature, high creatinine, advancing age, high white blood cell count, and high hematocrit are all risk factors.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on cellulitis and related soft tissue infections with this quiz. Explore essential questions about causes, treatments, and characteristics, including the comparison with conditions that resemble cellulitis. Ideal for medical students and healthcare professionals alike.