Podcast
Questions and Answers
What percentage of calcium in the blood plasma exists in the ionized or biologically active form?
What percentage of calcium in the blood plasma exists in the ionized or biologically active form?
- 50% (correct)
- 60%
- 30%
- 45%
What is the approximate weight of calcium in the average adult human body?
What is the approximate weight of calcium in the average adult human body?
- 1.5kg
- 500g
- 1kg (correct)
- 2kg
What is the primary carrier of protein-bound calcium in plasma?
What is the primary carrier of protein-bound calcium in plasma?
- Fibrinogen
- Albumin (correct)
- Globulin
- Transferrin
What happens to the plasma total [Ca2+] when the serum albumin concentration decreases by 1g/dL?
What happens to the plasma total [Ca2+] when the serum albumin concentration decreases by 1g/dL?
What is the ratio of intracellular [Ca2+] to extracellular [Ca2+]?
What is the ratio of intracellular [Ca2+] to extracellular [Ca2+]?
What is the primary function of calcium in muscle physiology?
What is the primary function of calcium in muscle physiology?
What is the form in which calcium is stored in bones?
What is the form in which calcium is stored in bones?
What is the percentage of calcium in the blood plasma that is complexed to phosphate and citrate?
What is the percentage of calcium in the blood plasma that is complexed to phosphate and citrate?
What is the corrected Ca2+ formula in mg/dL?
What is the corrected Ca2+ formula in mg/dL?
What is the effect of a decrease in blood pH on ionized Ca2+?
What is the effect of a decrease in blood pH on ionized Ca2+?
What is the approximate change in ionized [Ca2+] in response to a change in pH?
What is the approximate change in ionized [Ca2+] in response to a change in pH?
What is the role of parathyroid hormone (PTH) in response to low extracellular [Ca2+]?
What is the role of parathyroid hormone (PTH) in response to low extracellular [Ca2+]?
What is the effect of metabolic alkalosis on ionized Ca2+ levels?
What is the effect of metabolic alkalosis on ionized Ca2+ levels?
What is the role of calcitriol in calcium homeostasis?
What is the role of calcitriol in calcium homeostasis?
Which hormone stimulates production of calcitriol in the kidney?
Which hormone stimulates production of calcitriol in the kidney?
What is the primary function of calcium homeostasis?
What is the primary function of calcium homeostasis?
What is the primary function of chief cells in the parathyroid gland?
What is the primary function of chief cells in the parathyroid gland?
What is the effect of parathyroid hormone on bones?
What is the effect of parathyroid hormone on bones?
What is the primary mechanism of action of loop diuretics in treating hypercalcemia?
What is the primary mechanism of action of loop diuretics in treating hypercalcemia?
What is the minimum number of parathyroid glands required for normal function?
What is the minimum number of parathyroid glands required for normal function?
What is the effect of calcitonin on calcium levels in blood circulation?
What is the effect of calcitonin on calcium levels in blood circulation?
What is the primary goal of treatment in hypercalcemia?
What is the primary goal of treatment in hypercalcemia?
What is the effect of parathyroid hormone on phosphate levels in blood circulation?
What is the effect of parathyroid hormone on phosphate levels in blood circulation?
What is the location of the parathyroid glands in relation to the thyroid gland?
What is the location of the parathyroid glands in relation to the thyroid gland?
What is the effect of parathyroid hormone (PTH) on osteoclasts?
What is the effect of parathyroid hormone (PTH) on osteoclasts?
What is the effect of PTH on calcium reabsorption in the distal convoluted tubule and collecting duct?
What is the effect of PTH on calcium reabsorption in the distal convoluted tubule and collecting duct?
What is the role of 1-alpha-hydroxylase in the proximal convoluted tubule of the kidney?
What is the role of 1-alpha-hydroxylase in the proximal convoluted tubule of the kidney?
What is the characteristic of primary hyperparathyroidism?
What is the characteristic of primary hyperparathyroidism?
What is the cause of secondary hyperparathyroidism?
What is the cause of secondary hyperparathyroidism?
What is the effect of calcitriol on intestinal calcium absorption?
What is the effect of calcitriol on intestinal calcium absorption?
What is tertiary hyperparathyroidism?
What is tertiary hyperparathyroidism?
What is the effect of PTH on phosphate reabsorption in the proximal tubule?
What is the effect of PTH on phosphate reabsorption in the proximal tubule?
What is the primary indication for using cinacalcet?
What is the primary indication for using cinacalcet?
What is the effect of raloxifene on bone?
What is the effect of raloxifene on bone?
What is the primary route of excretion of raloxifene?
What is the primary route of excretion of raloxifene?
What is the primary adverse effect of cinacalcet?
What is the primary adverse effect of cinacalcet?
What is the primary indication for using raloxifene?
What is the primary indication for using raloxifene?
What is the effect of decreased parathyroid hormone levels?
What is the effect of decreased parathyroid hormone levels?
What is the treatment for hypoparathyroidism?
What is the treatment for hypoparathyroidism?
What is the bioavailability of raloxifene?
What is the bioavailability of raloxifene?
Study Notes
Calcium and Calcium Homeostasis
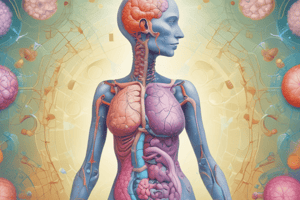
- Calcium is essential for:
- Current flow across excitable membranes (action potential)
- Fusion and release of storage vesicles (e.g., acetylcholine)
- Muscle contraction
- Second messenger intracellular (PLC, DAG, IP3)
- Blood coagulation
- Supporting the formation of bone (skeleton)
- Composition of calcium:
- Ca2+ is the most abundant mineral in the human body
- 99% of calcium is stored in bones in the form of phosphate and hydroxide salts, predominantly as hydroxyapatite
- The concentration of Ca2+ inside cells is 100,000 times less than in blood plasma
- In plasma, Ca2+ exists in three forms: 50% as ionized or biologically active form, 45% bound to plasma proteins, and 5% complexed to phosphate and citrate
Regulation of Calcium Homeostasis
- The biologic effect of Ca2+ is determined by the amount of ionized Ca2+, which is tightly regulated to remain within very narrow limits by homeostatic negative feedback
- Decrease in blood pH (metabolic acidosis) increases unbound (ionized) Ca2+ in blood plasma
- Increase in blood pH (metabolic alkalosis) leads to hypocalcemia
- Chelators such as citrate may transiently decrease ionized Ca2+
Parathyroid Hormone (PTH)
- PTH is secreted by the parathyroid gland in response to low calcium levels in the blood
- PTH regulates calcium and phosphate levels in blood circulation
- PTH is partially antagonistic to calcitonin
- PTH effects are present in the bones, kidneys, and small intestines
Effects of PTH
- On bones: PTH stimulates the release of calcium indirectly via osteoclasts, which causes resorption/destruction of bones
- On kidneys: PTH directly stimulates calcium reabsorption in the distal convoluted tubule and collecting duct
- On small intestines: PTH stimulates the production of 1-alpha-hydroxylase in the proximal convoluted tubule of the kidney, which catalyzes the synthesis of active vitamin D (calcitriol) from the inactive form (calcifediol)
Disorders of Calcium Homeostasis
- Hypercalcemia: characterized by an elevated level of calcium in the blood, treated by decreasing intestinal calcium absorption, increasing urinary calcium excretion, decreasing bone resorption, or removing excess calcium through dialysis
- Hypocalcemia: characterized by a low level of calcium in the blood, treated by correcting hypocalcemia by administering high-calcium diet, calcium supplements, and supplementary vitamin D
Disorders of Parathyroid Hormone
- Hyperparathyroidism: characterized by excessive production of PTH, which can be primary, secondary, or tertiary
- Hypoparathyroidism: characterized by decreased levels of PTH due to accidental removal of parathyroid glands during thyroid surgery or synthesis of biologically inactive PTH, leading to hypocalcemia.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the importance of calcium in the human body, including its role in muscle contraction, blood coagulation, and bone formation. Learn about the composition of calcium and its functions in various bodily processes.