Podcast
Questions and Answers
Which type of ossification occurs within mesenchymal or fibrous connective tissue?
Which type of ossification occurs within mesenchymal or fibrous connective tissue?
What is the main role of osteoclasts in bone formation?
What is the main role of osteoclasts in bone formation?
What happens to chondrocytes after they produce a calcified matrix?
What happens to chondrocytes after they produce a calcified matrix?
Which bones are primarily formed through intramembranous ossification?
Which bones are primarily formed through intramembranous ossification?
Signup and view all the answers
During bone growth in thickness, what is formed when periosteal cells differentiate into osteoblasts?
During bone growth in thickness, what is formed when periosteal cells differentiate into osteoblasts?
Signup and view all the answers
What change occurs to the epiphyseal plate after adolescence?
What change occurs to the epiphyseal plate after adolescence?
Signup and view all the answers
Which of the following describes the process of bone growth in length at the epiphyseal plate?
Which of the following describes the process of bone growth in length at the epiphyseal plate?
Signup and view all the answers
What happens during the fusion of ridges in the process of bone growth in thickness?
What happens during the fusion of ridges in the process of bone growth in thickness?
Signup and view all the answers
Which of the following describes the primary function of long bones?
Which of the following describes the primary function of long bones?
Signup and view all the answers
What type of tissue is primarily responsible for producing red and white blood cells in the bones?
What type of tissue is primarily responsible for producing red and white blood cells in the bones?
Signup and view all the answers
Which bone type is characterized as being roughly cuboidal in shape?
Which bone type is characterized as being roughly cuboidal in shape?
Signup and view all the answers
Which type of cartilage is characterized by a gel-like matrix with fine fibers and is commonly found in most joints?
Which type of cartilage is characterized by a gel-like matrix with fine fibers and is commonly found in most joints?
Signup and view all the answers
Which component of bone tissue aids in energy metabolism and insulin production?
Which component of bone tissue aids in energy metabolism and insulin production?
Signup and view all the answers
What role do compression lines and tension lines play in bone structure?
What role do compression lines and tension lines play in bone structure?
Signup and view all the answers
What distinguishes sutural bones from flat bones?
What distinguishes sutural bones from flat bones?
Signup and view all the answers
Which of the following best describes the function of the bony skeleton?
Which of the following best describes the function of the bony skeleton?
Signup and view all the answers
Which of the following is NOT a function of bones?
Which of the following is NOT a function of bones?
Signup and view all the answers
In which type of ossification does bone form directly from mesenchymal tissue?
In which type of ossification does bone form directly from mesenchymal tissue?
Signup and view all the answers
Which type of bone has air pockets or is hollow in structure?
Which type of bone has air pockets or is hollow in structure?
Signup and view all the answers
What is the primary shape characteristic of flat bones?
What is the primary shape characteristic of flat bones?
Signup and view all the answers
What is a key characteristic of fibrocartilage that distinguishes it from hyaline cartilage?
What is a key characteristic of fibrocartilage that distinguishes it from hyaline cartilage?
Signup and view all the answers
Which of the following bones is an example of an irregular bone?
Which of the following bones is an example of an irregular bone?
Signup and view all the answers
Which component of bone tissue is responsible for storing minerals and fats?
Which component of bone tissue is responsible for storing minerals and fats?
Signup and view all the answers
Which of the following best describes the classification of bones by shape?
Which of the following best describes the classification of bones by shape?
Signup and view all the answers
Which tissue types contribute to the composition of bone?
Which tissue types contribute to the composition of bone?
Signup and view all the answers
Which type of cartilage is absent of perichondrium and helps resist compression and tension forces?
Which type of cartilage is absent of perichondrium and helps resist compression and tension forces?
Signup and view all the answers
What distinguishes spongy bone from compact bone at the microscopic level?
What distinguishes spongy bone from compact bone at the microscopic level?
Signup and view all the answers
What is a primary function of the extracellular matrix in bone tissue?
What is a primary function of the extracellular matrix in bone tissue?
Signup and view all the answers
Which function is NOT performed by the periosteum?
Which function is NOT performed by the periosteum?
Signup and view all the answers
What primary function does the endosteum serve?
What primary function does the endosteum serve?
Signup and view all the answers
How do the structures within the periosteum contribute to bone health?
How do the structures within the periosteum contribute to bone health?
Signup and view all the answers
In which area are nutrient arteries and veins primarily located?
In which area are nutrient arteries and veins primarily located?
Signup and view all the answers
What is an accurate description of the orientation of bone tissues in response to stress?
What is an accurate description of the orientation of bone tissues in response to stress?
Signup and view all the answers
Which bone cell type is primarily responsible for bone resorption and regulation of calcium levels?
Which bone cell type is primarily responsible for bone resorption and regulation of calcium levels?
Signup and view all the answers
What percentage of the bone matrix is made up of minerals?
What percentage of the bone matrix is made up of minerals?
Signup and view all the answers
Which layer of the periosteum is responsible for the generation of new bone cells?
Which layer of the periosteum is responsible for the generation of new bone cells?
Signup and view all the answers
What is the main function of spongy bone tissue?
What is the main function of spongy bone tissue?
Signup and view all the answers
What is found within the lacunae of spongy bone tissue?
What is found within the lacunae of spongy bone tissue?
Signup and view all the answers
What characterizes the matrix of bone tissue compared to other types of connective tissue?
What characterizes the matrix of bone tissue compared to other types of connective tissue?
Signup and view all the answers
Which of the following minerals is NOT typically found in the bone matrix?
Which of the following minerals is NOT typically found in the bone matrix?
Signup and view all the answers
Which feature distinguishes compact bone from spongy bone?
Which feature distinguishes compact bone from spongy bone?
Signup and view all the answers
Which type of bone responds to stress by aligning its trabeculae along the lines of force?
Which type of bone responds to stress by aligning its trabeculae along the lines of force?
Signup and view all the answers
What is the primary role of collagen fibers within the bone matrix?
What is the primary role of collagen fibers within the bone matrix?
Signup and view all the answers
Osteoblasts are responsible for the breakdown of bones.
Osteoblasts are responsible for the breakdown of bones.
Signup and view all the answers
When periosteal cells differentiate, they create ridges around blood vessels.
When periosteal cells differentiate, they create ridges around blood vessels.
Signup and view all the answers
Chondrocytes die during bone growth due to the calcification of the matrix they produce.
Chondrocytes die during bone growth due to the calcification of the matrix they produce.
Signup and view all the answers
Dermal bones are primarily formed through endochondral ossification.
Dermal bones are primarily formed through endochondral ossification.
Signup and view all the answers
After adolescence, the epiphyseal plate remains active and continues to allow bone growth.
After adolescence, the epiphyseal plate remains active and continues to allow bone growth.
Signup and view all the answers
The process of ossification within mesenchymal tissue is called dermis ossification.
The process of ossification within mesenchymal tissue is called dermis ossification.
Signup and view all the answers
During bone growth in thickness, the periosteum becomes the endosteum.
During bone growth in thickness, the periosteum becomes the endosteum.
Signup and view all the answers
Osteoclasts play a role in the creation of new bone by forming new lamellae.
Osteoclasts play a role in the creation of new bone by forming new lamellae.
Signup and view all the answers
Fibrocartilage is characterized by large bundles of elastin and is primarily found in joints.
Fibrocartilage is characterized by large bundles of elastin and is primarily found in joints.
Signup and view all the answers
The axial skeleton is primarily responsible for protecting vital organs such as the heart and lungs.
The axial skeleton is primarily responsible for protecting vital organs such as the heart and lungs.
Signup and view all the answers
The primary function of bones includes hormone production that influences fat storage and insulin production.
The primary function of bones includes hormone production that influences fat storage and insulin production.
Signup and view all the answers
Compact bone tissue is structured to withstand tension by forming trabeculae that align randomly.
Compact bone tissue is structured to withstand tension by forming trabeculae that align randomly.
Signup and view all the answers
Pneumatized bones are characterized as having a solid structure without any air pockets.
Pneumatized bones are characterized as having a solid structure without any air pockets.
Signup and view all the answers
Hyaline cartilage is the least common type of cartilage found in the human body.
Hyaline cartilage is the least common type of cartilage found in the human body.
Signup and view all the answers
The femur is classified as a flat bone due to its elongated shape.
The femur is classified as a flat bone due to its elongated shape.
Signup and view all the answers
Short bones have an elongated shape and are primarily found in the limbs.
Short bones have an elongated shape and are primarily found in the limbs.
Signup and view all the answers
Sesamoid bones are typically located within tendons and provide additional support.
Sesamoid bones are typically located within tendons and provide additional support.
Signup and view all the answers
Intramembranous ossification occurs within hyaline cartilage.
Intramembranous ossification occurs within hyaline cartilage.
Signup and view all the answers
Chondrocytes are responsible for producing the collagen matrix in cartilage.
Chondrocytes are responsible for producing the collagen matrix in cartilage.
Signup and view all the answers
The rib cage functions primarily to assist in the movement of limbs.
The rib cage functions primarily to assist in the movement of limbs.
Signup and view all the answers
Irregular bones, such as the vertebrae, have a shape that can vary significantly.
Irregular bones, such as the vertebrae, have a shape that can vary significantly.
Signup and view all the answers
Spongy bone contains a network of trabecular that allows for the storage of red and white blood cells.
Spongy bone contains a network of trabecular that allows for the storage of red and white blood cells.
Signup and view all the answers
The extracellular matrix of bone tissue is primarily composed of chondrocytes and collagen fibers.
The extracellular matrix of bone tissue is primarily composed of chondrocytes and collagen fibers.
Signup and view all the answers
Flat bones consist of two layers of spongy bone sandwiched between layers of compact bone.
Flat bones consist of two layers of spongy bone sandwiched between layers of compact bone.
Signup and view all the answers
The perichondrium is absent in articular cartilage, which provides a smooth surface for joints.
The perichondrium is absent in articular cartilage, which provides a smooth surface for joints.
Signup and view all the answers
Bones primarily serve to absorb shock and prevent fractures during high-impact activities.
Bones primarily serve to absorb shock and prevent fractures during high-impact activities.
Signup and view all the answers
Blood cell production occurs in red bone marrow, which is found mainly in long bones.
Blood cell production occurs in red bone marrow, which is found mainly in long bones.
Signup and view all the answers
The epiglottis is a type of bone located in the rib cage.
The epiglottis is a type of bone located in the rib cage.
Signup and view all the answers
The periosteum is fully continuous at all instances on bone surfaces.
The periosteum is fully continuous at all instances on bone surfaces.
Signup and view all the answers
Endosteum is comprised of multiple layers of mature bone cells.
Endosteum is comprised of multiple layers of mature bone cells.
Signup and view all the answers
The nutrient foramen is typically associated with multiple nutrient arteries.
The nutrient foramen is typically associated with multiple nutrient arteries.
Signup and view all the answers
Spongy bone adapts better to multidirectional tension compared to compact bone.
Spongy bone adapts better to multidirectional tension compared to compact bone.
Signup and view all the answers
Surface markings on bones are present at birth for all types.
Surface markings on bones are present at birth for all types.
Signup and view all the answers
The matrix of bone tissue is composed of 15% water, 30% collagen fibers, and 55% minerals.
The matrix of bone tissue is composed of 15% water, 30% collagen fibers, and 55% minerals.
Signup and view all the answers
Osteocytes are the only bone cells that can divide and are found in the endosteum.
Osteocytes are the only bone cells that can divide and are found in the endosteum.
Signup and view all the answers
Spongy bone tissue contains central canals that house blood vessels.
Spongy bone tissue contains central canals that house blood vessels.
Signup and view all the answers
The periosteum consists of an outer fibrous layer and an inner cellular layer containing osteoblasts.
The periosteum consists of an outer fibrous layer and an inner cellular layer containing osteoblasts.
Signup and view all the answers
Minerals such as hydroxyapatite and calcium phosphate contribute to the rigidity of bone.
Minerals such as hydroxyapatite and calcium phosphate contribute to the rigidity of bone.
Signup and view all the answers
Osteoclasts are derived from nerve cells and are important for regulating calcium levels in the body.
Osteoclasts are derived from nerve cells and are important for regulating calcium levels in the body.
Signup and view all the answers
Trabeculae in spongy bone tissue are arranged randomly and do not follow lines of stress.
Trabeculae in spongy bone tissue are arranged randomly and do not follow lines of stress.
Signup and view all the answers
The external layer of compact bone is referred to as the cortex.
The external layer of compact bone is referred to as the cortex.
Signup and view all the answers
Bone marrow is present within spongy bone tissues but lacks a marrow cavity.
Bone marrow is present within spongy bone tissues but lacks a marrow cavity.
Signup and view all the answers
Osteoblasts are responsible for the breakdown of bone tissue and are found concentrated in the periosteum.
Osteoblasts are responsible for the breakdown of bone tissue and are found concentrated in the periosteum.
Signup and view all the answers
Study Notes
Bone formation
- Bone formation occurs through two primary processes: endochondral ossification and intramembranous ossification.
- Endochondral ossification involves the replacement of hyaline cartilage with bone.
- Intramembranous ossification occurs within mesenchymal or fibrous connective tissue, forming dermal bones.
- Mesenchymal cells differentiate into osteoblasts, chondrocytes, and osteoclasts.
- Osteoblasts build bone tissue, chondrocytes form cartilage, and osteoclasts break down bone.
Bone growth
- Bone growth in length occurs at the epiphyseal plate, a layer of hyaline cartilage.
- The process involves chondrocyte division and growth, followed by calcification and replacement by bone tissue.
- Bone growth in thickness occurs through the activity of osteoblasts in the periosteum.
- Periosteal cells differentiate into osteoblasts, forming ridges around blood vessels.
- These ridges fuse, forming canals that are then filled with new bone tissue.
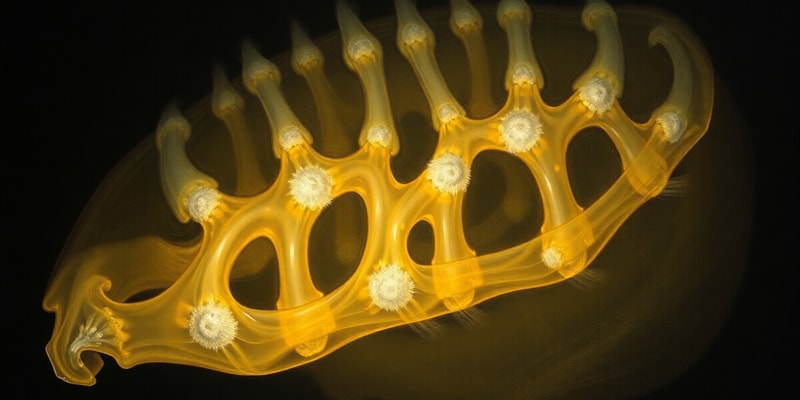
Cartilage
- Cartilage is a connective tissue composed of collagen and/or elastic fibers embedded in a gel-like matrix.
- Chondrocytes are the cells found within cartilage.
- Cartilage is avascular, meaning it lacks blood vessels.
- The three types of cartilage are hyaline cartilage, fibrocartilage, and elastic cartilage.
Functions of bones
- Bones provide support for the body, facilitating movement through lever systems with muscles.
- They protect vital organs such as the brain, heart, and lungs.
- Bones store minerals like calcium and phosphate.
- They produce blood cells in the red bone marrow.
- Bones play a role in energy metabolism, producing a hormone called osteocalcin.
Types of bones
- Bones are categorized based on their shape:
- Long bones: elongated with a shaft and two ends, providing strength and mobility (e.g., femur, tibia).
- Short bones: roughly cuboidal, designed for stability and shock absorption (e.g., carpals, tarsals).
- Flat bones: thin and flat, offering protection and muscle attachment (e.g., skull bones, ribs, sternum).
- Irregular bones: varied shapes, customized for specific functions (e.g., vertebrae, facial bones).
- Sesamoid bones: small, round bones embedded in tendons, reducing friction and increasing leverage (e.g., patella).
- Sutural bones: small, oddly shaped bones found between flat bones of the skull.
- Pneumatized bones: hollow bones or containing air pockets, like the ethmoid bone.
Anatomy of a long bone
- A long bone consists of a diaphysis (shaft), two epiphyses (ends), and a metaphysis (region between the diaphysis and epiphysis).
- The diaphysis contains the medullary cavity, which houses bone marrow.
- The epiphysis contains spongy bone and articular cartilage.
- The periosteum covers the outer surface of the bone, while the endosteum lines the medullary cavity.
Composition of bone tissue
- Bone tissue consists of an extracellular matrix and cells.
- The matrix is composed of collagen fibres, providing elasticity, and mineral salts (hydroxyapatite), providing rigidity.
- Bone cells include:
- Osteogenic cells: undifferentiated cells responsible for bone repair and growth.
- Osteoblasts: bone-building cells that secrete collagen fibres.
- Osteocytes: mature bone cells responsible for bone maintenance.
- Osteoclasts: bone-resorbing cells that breakdown bone tissue.
Compact bone
- Compact bone is the dense, hard outer layer of bone, providing strength and support.
- It is organized into osteons, containing lamellae, canaliculi, a central canal, and osteocytes.
Spongy bone
- Spongy bone is the lighter, porous inner layer of bone, providing support and housing red bone marrow.
- It is composed of trabeculae, which are interconnected struts of bone tissue.
- Spongy bone is found in areas subjected to less stress compared to compact bone.
Periosteum and Endosteum
- The periosteum is a fibrous membrane covering the outer surface of bone.
- It participates in bone growth and repair, houses blood vessels and nerves, and attaches to tendons and ligaments.
- The endosteum lines the medullary cavity and covers trabeculae in spongy bone.
Blood and Nerve Supply
- Bone tissue is richly supplied by blood vessels and nerves.
- The nutrient artery provides blood supply to the diaphysis, while other arteries and veins supply the epiphyses and metaphyses.
- Nerves follow blood vessels and are essential for pain sensation.
Forces at work
- Bone tissue is designed to withstand tension and compression forces.
- Compact bone is thicker in areas where forces are greater, while spongy bone is better suited for multidirectional tension.
- Bone tissue is continuously remodeled throughout life, adapting to changes in force.
Bone surface markings
- Bones have distinctive markings, including projections, depressions, and openings.
- These markings serve as attachment points for tendons and ligaments, provide passageways for blood vessels and nerves, and may indicate the direction of force.
- Bone surface markings can change over time due to tension and compression forces.
Osteogenesis
- Osteogenesis is bone formation, which involves the activity of osteoblasts and osteoclasts.
- Two types of ossification occur: intramembranous and endochondral.
- Intramembranous ossification forms dermal bones directly within mesenchymal tissue.
- Endochondral ossification involves the replacement of cartilage by bone, forming most bones in the body.
Bone fracture healing
- Fracture healing involves several stages:
- Hematoma formation: blood clot forms at the fracture site.
- Soft callus formation: fibrocartilaginous tissue replaces the clot.
- Hard callus formation: bone tissue replaces the soft callus.
- Remodeling: the hard callus is remodeled into a more normal bone shape.
- Factors affecting healing include age, nutrition, and the type of fracture.
Skeletal System
- The skeletal system is composed of cartilage and bones, connected by joints.
- It is divided into the axial skeleton (skull, vertebral column, ribs, and sternum) and the appendicular skeleton (limbs, girdles, and bones of the hands and feet).
- The skeletal system provides support, protection, movement, mineral storage, and blood cell production, playing a critical role in maintaining overall body function.
Bone Formation - Endochondral Ossification
- Mesenchymal cells can differentiate into various cell types, including osteoblasts, chondrocytes, and osteoclasts.
- Osteoblasts are bone cells responsible for bone formation.
- Chondrocytes are cartilage cells that produce cartilage.
- Osteoclasts are responsible for breaking down bone tissue.
Bone Formation - Intramembranous Ossification
- Intramembranous ossification occurs when osteoblasts differentiate within mesenchymal or fibrous connective tissue.
- This process is also called dermis ossification and occurs in the deeper layers of the dermis.
- Bones formed through this process are called dermal bones.
- Examples of dermal bones include the flat bones of the skull, facial bones, mandible, medial part of the clavicle.
Bone Growth (Length)
- The growth of long bones in length is determined by the epiphyseal plate.
- The epiphyseal plate is made of hyaline cartilage and has several zones responsible for bone growth.
- Zone one anchors the epiphyseal plate to the epiphysis.
- Zone two consists of chondrocytes that divide and form columns.
- Zone three features chondrocytes that enlarge and produce a calcified matrix, leading to cell death.
- Zone four witnesses the dissolution of calcified cartilage by osteoclasts.
- Zone five marks the invasion of the area by osteoblasts and blood vessels from the diaphysis, forming new bone tissue.
- After adolescence, the epiphyseal plate becomes ossified, ending bone growth.
Bone Growth (Thickness)
- Bone growth in thickness is achieved through the activity of the periosteum.
- Periosteal cells differentiate into osteoblasts, producing bone matrix and forming ridges around blood vessels.
- These ridges eventually fuse, forming a canal surrounding the blood vessel.
- The periosteum transforms into endosteum, with osteoblasts creating new lamellae, effectively closing the canal.
- This process forms a new osteon, with further growth resulting in new circumferential lamellae.
Cartilage
- Cartilage is a type of connective tissue composed of collagen and/or elastic fibers embedded in a gel-like matrix.
- Chondrocytes reside within lacunae (small cavities) within the cartilage.
- Cartilage lacks nerves and blood vessels.
- Some cartilage is surrounded by perichondrium, a connective tissue layer containing fibroblasts and chondroblasts.
Types of Cartilage
- Hyaline cartilage: The most common type, featuring fine fibers in a gel-like matrix. Found in most articulations, joints.
- Fibrocartilage: Composed of large bundles of collagen, resisting compression and tension forces. Found in the anulus fibrosus.
- Elastic cartilage: Rich in elastic fibers, providing flexibility. Present in the epiglottis.
Bones
- Bones are considered organs, comprised of different types of tissues: bone, cartilage, adipose, blood, epithelial tissue, blood vessels and nervous tissue.
Functions of Bones
- Provide structural support and framework for the body.
- Work with muscles for movement, acting as levers.
- Protect vital organs within the skull, rib cage, vertebral column, and pelvis.
- Store minerals like calcium and phosphate, which can be released into the bloodstream.
- Produce red and white blood cells, storing energy in the red bone marrow.
- Play a role in energy metabolism by producing osteocalcin, a hormone that influences bone production, fat storage, and insulin production.
Types of Bones
- Flat bones: Thin compact bone layer surrounding spongy bone, called the diploë. Examples include the roof of the skull, ribs, sternum, and scapula.
- Sutural bones: Oddly shaped bones found between flat bones of the skull.
- Pneumatized bones: Hollow bones containing air pockets, like the ethmoid bone.
- Long bones: Elongated shape, composing the limbs, fingers, and toes.
- Short bones: Roughly cuboidal shape, found in the carpals and tarsals.
- Sesamoid bones: Present within tendons, like the patella.
- Irregular bones: Varying shape, including vertebrae, some facial bones, and the heel bone.
Anatomy of a Long Bone
- Long bones, like the femur and tibia, are subjected to significant loads and are crucial for skeletal mobility.
- They consist of a diaphysis (shaft) and two epiphyses (ends).
- The diaphysis houses the medullary cavity, filled with bone marrow.
- The epiphyses are covered in articular cartilage, facilitating smooth joint movement.
- The metaphysis region connects the diaphysis and epiphysis, housing the epiphyseal plate responsible for longitudinal growth.
- The periosteum, a fibrous membrane covering the outer surface of the bone, facilitates growth and repair.
Structure of Short, Irregular, and Flat Bones
- These bones have external layers of compact bone covered by the periosteum and internal layers of spongy bone (diploë) covered by the endosteum.
- They lack a distinct marrow cavity but contain bone marrow.
- Blood vessels and nerves penetrate these bones similar to long bones.
Composition of Bone Tissue
- Bone tissue consists of an extracellular matrix composed of water, collagen fibers, and minerals, primarily hydroxyapatite.
- Collagen fibers provide elasticity, while mineral salts impart rigidity.
- The matrix contains various cell types, including:
- Osteogenic cells: Unspecialized cells capable of dividing and forming other bone cell types.
- Osteoblasts: Actively synthesize and secrete bone matrix.
- Osteocytes: Mature bone cells responsible for maintaining the bone matrix.
- Osteoclasts: Large, multinucleated cells that dissolve bone tissue for remodeling and calcium regulation.
Compact Bone
- The outer layer of bone, providing strength and support.
- Composed of osteons, or Haversian systems, which are cylindrical units containing concentric lamellae, containing lacunae with osteocytes.
- Canaliculi connect osteocytes to each other and to the central canal, providing a pathway for nutrients and waste removal.
- Central canals house blood vessels and nerves.
Spongy Bone Tissue
- The internal layer of bone, characterized by a porous structure with trabeculae.
- Trabeculae lack a central canal, and osteocytes receive nutrients via diffusion from blood vessels in the endosteum.
- Spongy bone reduces the weight of bones, provides support, protects red bone marrow, and is found in areas subjected to lighter stress.
Periosteum and Endosteum
- Periosteum: A fibrous membrane covering the outer surface of bone, composed of an outer fibrous layer and an inner cellular layer containing osteoprogenitor cells.
- Endosteum: A single layer of osteoprogenitor cells lining the medullary cavity and the central canals of osteons, actively involved in growth and remodeling.
Blood and Nerve Supply
- Bones receive blood supply from the nutrient artery, branching into the medullary cavity, epiphyses, and periosteum.
- Nerves follow the blood vessels, providing sensory innervation, making fractures painful.
Forces at Work
- The arrangement of compact and spongy bone tissues aligns along lines of stress.
- Compact bone is thicker in areas of high stress, while the meshwork of spongy bone is oriented to counteract stress.
- Spongy bone is ideal for multidirectional tension.
Bone Surface Markings
- Bones develop surface markings, providing attachment points for tendons and ligaments, influenced by tension and compression forces.
- These markings are not present at birth and develop as muscles are used.
- Other markings facilitate the passage of nerves and blood vessels.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the processes of bone formation, including endochondral and intramembranous ossification. Learn how bones grow in length and thickness through specific cellular activities at the epiphyseal plate and periosteum. This quiz will test your understanding of the biological mechanisms behind bone and cartilage development.